February saw the publication of Investment and Evolution: A five-year framework for GP contract reform to implement The NHS Long Term Plan, which includes a major overhaul of the Quality and Outcomes Framework (QOF) across England for 2019/20 (NHS England, 2019).
Twenty-eight QOF indicators, worth 175 points, are being retired. Seventy-four points will be used to create a new Quality Improvement Domain, with the first two modules focusing on prescribing safely and end-of-life care. The remaining 101 points will be used to introduce 15, more clinically appropriate, indicators, including on diabetes and blood pressure (BP). Current exception reporting will be replaced with “personalised care adjustment” designed to better reflect individual clinical situations and patients’ wishes. The new Network Contract Directed Enhanced Service (DES) will offer incentives to encourage practices to work together across their neighbourhood, similar to cluster working in Wales. This DES is expected to be rolled out across England by July 2019. There is a promise that future contract changes will be tested prior to introduction.
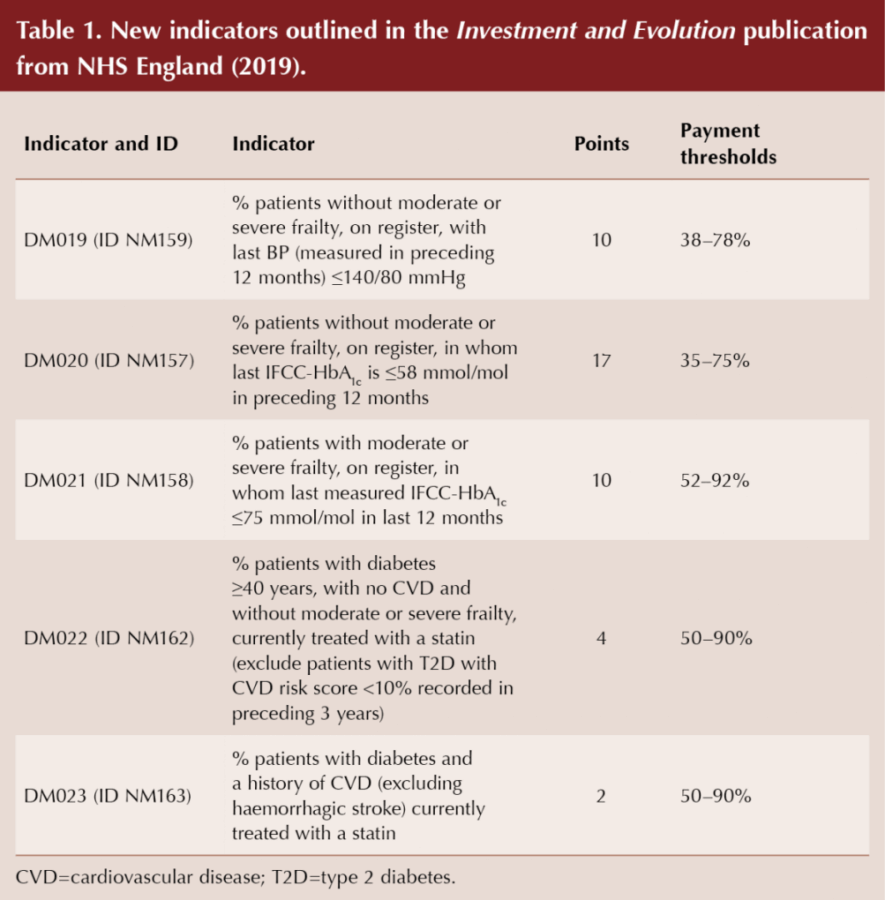
So, what does this mean for primary care diabetes? Indicators DM002 and DM003 (BP targets), DM004 (cholesterol), and DM007, DM008 and DM009 (glycaemic targets of ≤58 mmol/mol, ≤64 mmol/mol and ≤75 mmol/mol) have been retired. Diabetes remains a priority area for NHS England, and the retired indicators will be replaced with treatment targets (negotiated by Partha Kar [NHS England’s Clinical Director of Diabetes] and his team) stratified to take account of moderate or severe frailty. Likewise, CHD002 (BP target for patients with coronary heart disease) has been replaced with a more clinically appropriate target. PAD002 and PAD003 (BP and aspirin/anti-platelet therapy in those with peripheral arterial disease) are no longer felt to be priorities for incentivisation, as there is significant overlap with other cardiovascular disease areas. However, data extraction for these two areas will continue, supported through the Indicators No Longer Incentivised in QOF (INLIQ). SMOK003, supporting patients who smoke to stop, is seen as core professional practice and the incentivisation has been removed.
Data collection via INLIQ for previous DM016 (advice and assessment for ED) and STIA004 (percentage of patients with a stroke or transient ischaemic attack who have a record of total cholesterol in the preceding 12 months) may cease from April 2019, together with HYP004 and HYP005, which monitored physical activity coding and brief intervention regarding physical activity in the 16–74 age range.
Partha Kar told the PCDS: “This has been the culmination of months of close working between the NHS England diabetes team and the BMA, and we are delighted that the important issue of frailty is being looked into, with focus on individualised care, rather than a non-evidence-based, target-driven culture. We hope this will help with issues of safety and avoid pitfalls of over-treatment. My thanks to David Strain and Andrew Green for their hard work to make this come to life.”
The new diabetes domain is designed to reduce under-treatment and encourage ongoing good practice in those without frailty, while reducing potential for over-treatment and iatrogenic harm to patients with moderate or severe frailty. Clinical systems can already calculate the electronic Frailty Index (eFI) and alert us to moderate or severe frailty. This should not be used on its own to diagnose frailty, but should help us consider whether the diagnosis is appropriate, based primarily on whether we think it would benefit the patient. A SNOMED code would then be manually entered into the record, which would trigger the interventions for frail patients, as specified in the General Medical Services (GMS) contract (e.g. medication review, falls assessment, consent for enriched data sharing and the appropriate diabetes indicators).
The new diabetes indicators are summarised in Table 1.
Indicators DM017 (maintaining a register – 6 points), DM006 (treatment of those with nephropathy or albuminuria with ACEI or ARB – 3 points), DM012 (foot examination and risk coding – 4 points), DM014 (referral to structured education within 9 months of diagnosis – 11 points) and DM018 (flu immunisation – 3 points) persist unchanged.
In Wales, for 2018/19, only maintenance of the diabetes register is in the active indicators, with the potential for 2 points only to be awarded, based on maintaining this at 31 March 2019. The remainder of the diabetes domain indicators are in the inactive group and, therefore, for year 2018/19, payment will be based on achievement points used to calculate payment in year 2017/18. Contract negotiations for 2019/20 are underway in Wales and Northern Ireland.
PCDS Clinical Hubs
For over 20 years, the PCDS has focused on making quality education easily accessible to our members and other clinicians. During 2017/18, our commitment expanded significantly, including updating our website with the addition of interactive online journals and additional CPD modules. To date, the most widely used module has been Six Steps to Insulin Safety, which has been completed by nearly 26000 healthcare professionals across the UK.
Early last year, after a rigorous brainstorming session where we reviewed diabetes education resources available to us and identified important educational gaps we wanted to fill, the PCDS Clinical Hubs project began to take shape. We wanted to create a resource that would engage members with different initial levels of knowledge and experience, and provide more in-depth coverage of topics for those who wanted a “deep dive” into additional content. As clinical practice is changing rapidly, we agreed to start with a comprehensive cardiovascular hub where we could share best practice for assessing and managing cardiovascular disease, including an overview of the outcomes from published cardiovascular outcomes trials (CVOTs) and how these can be incorporated in guidelines and day-to-day consultations.
After months of intensive work, very ably supported by our in-house team, I am excited to announce that the first two PCDS Clinical Hubs, the Cardiovascular Hub and the GLP-1 Hub, are now live and free to access at https://diabetesonthenet.com/pcds-hubs. Designed to help busy healthcare professionals stay abreast of advances in diabetes, each hub contains four interactive modules designed to take around 30 minutes each to complete. 0.5 CPD credits are available on completion of each module, and a certificate can be downloaded for appraisal and revalidation. A suite of short consultation guides accompanies each Hub, summarising the key messages and acting as a prompt in consultations. Patient leaflets facilitate interaction in consultations and can be retained by people with diabetes to remind them of their discussion. Although I had seen and contributed to the materials at various stages in their development, I was impressed by the finished interactive Hubs, and found them concise, easy and enjoyable to use. I hope you will try them out and share your feedback with us.
Credit is due to: David Millar-Jones, who took on the challenging task of writing the Hub modules; Kevin Fernando, who wrote the consultation aids; Jane Diggle and Nicki Milne, who shared their expertise in the patient leaflets; and all the other PCDS education committee members who helped review the modules, happily sharing their time and knowledge. Katherine Brady, Sean Delaney and all our in-house team worked tirelessly to keep us on track and make the project happen. We are extremely grateful to Novo Nordisk who, through a sponsorship, fully funded all costs for the development and hosting of the Clinical Hubs, while giving us complete freedom to develop the content. Full editorial control remains the sole responsibility of the PCDS.
Cardiovascular risk in Scotland improves – but less so in those with diabetes
Although the incidence of myocardial infarction (MI), angina and revascularisation decreased across Scotland between 2006 and 2015, the increased risk in those with type 2 diabetes persisted (Read et al, 2019). Acute MI declined by an average of 2% per year. Likewise, despite there being a decline in 30-day mortality in both those with and without type 2 diabetes, rates remained higher in those with the condition. QOF’s focus on those with chronic disease, including diabetes, during that time would have been anticipated to incentivise increased efforts to reduce and manage cardiovascular risk factors in people with diabetes.
The authors attributed the population-wide reductions in cardiovascular disease to smoking cessation, reduced salt intake and improved BP and lipid treatment. Smoking prevalence across the Scottish population decreased from 28% to 21% between 2003 and 2015, while it decreased by around half the amount, from 21.4% to 18.1% over the 10 years to 2015 in those with diabetes.This retrospective cohort study, undertaken by the Scottish Diabetes Research Network, examined nearly 35 million person-years of follow-up. If you are interested in becoming involved with your local Research Network to participate in studies like this, learn more about how participating in primary care research can be mentally stimulating and academically rewarding by reading Philip Evans and Lisa Gibbons’ commentary in the current issue.
In this issue
Also in this issue, we encourage you to read about childhood obesity and the sugar tax with Rachel Pryke, and to learn about our primary care responsibilities in helping children with diabetes stay safe in our featured CPD module. Learn more about the papers that changed clinical practice in lipid management with Mike Kirby, and learn How to diagnose and manage NAFLD with Jane Diggle and Andrew Yeoman. If you missed Joan St John’s award-winning poster at the PCDS National Conference in November, read more about her team’s development of dietary resources for BAME communities in north-west London and how you can share those resources. If you were not able to attend the Scottish Conference of the PCDS in October, summary messages can be read in our mini-conference report.
Finally, I wanted to say a very big additional “thank you” to David for all his hard work as Chairman of PCDS, leading the society over the last 6 years. That responsibility has now passed seamlessly onto the very capable shoulders of Clare Hambling, GP in Norfolk, who is already busy in her new role. I hope to tempt Clare to write for Diabetes & Primary Care again soon, to share the work she has done on diabetes management in the elderly, including de-prescribing.Sadly, I’ll miss the Diabetes UK Professional Conference this year, as I am travelling in New Zealand, but I have plans to learn more about primary care management of diabetes while I am there and will share that on my return. In the meantime, don’t forget to give us feedback on our Clinical Hubs and, if you want to write for the journal, email us at [email protected].





Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025