The National Diabetes Audit (2018) showed that there were approximately 3.3 million people living with diabetes in England and Wales, including over half a million people from the black, Asian and minority ethnic (BAME) communities. People within BAME communities are disproportionately at risk of developing diabetes at a younger age and, consequently, are at greater risk of experiencing the complications associated with type 2 diabetes (Tillin et al, 2012), including developing cardiovascular complications such as coronary heart disease and stroke.
In Scotland, people living in BAME communities form 6.7% of the recorded population of people living with diabetes, compared to 5.5% in the overall population (Scottish Diabetes Data Group, 2018). In Northern Ireland, diabetes is more prevalent in Asian and black ethnic groups (12.4% and 8.4%, respectively) compared to the overall population (5.4%; Belfast Health and Social Care Trust, 2018).
The first-line management of type 2 diabetes includes the provision of dietary advice. NICE guideline NG28 (2015) recommends that this is both individualised and culturally relevant:
Evidence shows that when information, education or advice is culturally focused, the outcomes for people living with diabetes are improved (Zeh, 2012; Attridge et al, 2014). The challenges for healthcare professionals are to ensure that dietary advice fulfils this remit.
Ensuring that dietary advice is culturally specific and relevant, rather than generic and trans-located to another culture, is a skill that some professionals find difficult to achieve with the current available resources. This was the day-to-day experience of two primary care healthcare professionals working in north-west London. The London Borough of Brent is an area with an ethnically diverse population, where the majority of residents are from BAME communities and as many as 149 languages are spoken (Brent CCG and London Borough of Brent, 2015). It has one of the highest prevalences of diabetes in the country.
Our experience in Brent was that people were asking for dietary information that related to food they recognised and advice in a format that they could understand. Many people eat a wide variety of food from different sources, but the traditional diets of people from BAME communities can be up to 60% carbohydrate in content (Leung and Stanner, 2011; Thaker and Barton, 2012; Goff et al, 2014; Dehghan et al, 2017). Carbohydrates are the nutrients that exert the greatest effect on blood glucose, but we found that people were mainly aware of free sugars and often did not recognise the other sources of carbohydrate in their traditional foods.
Within this landscape, we decided to design three culturally specific, dietary information booklets for people living with diabetes from the African and Caribbean, Gujarati and Pakistani communities. Our aims were to keep the message simple, pictorial and culturally relevant, so that people with diabetes would not have difficulty understanding the message about the carbohydrate content of the traditional foods they were eating.
We wanted to ensure that: healthcare professionals and people from BAME communities, who may not have the same cultural experience or speak the same language, would be able to communicate effectively; people with diabetes from the BAME communities would engage with these resources because of its cultural relevance; and that the sometimes-negative experiences of healthcare (e.g. in terms of communication) reported by BAME communities (such as in the Health Survey for England [Department of Health, 2009]) were not replicated.
The finished booklets provided photographs of foods commonly eaten in the selected communities, alongside their carbohydrate content (Figure 1). This was to enable people to have a better understanding of the carbohydrate content of the food they were eating and how this might affect their blood glucose. To evaluate the effectiveness of the booklets, a pilot study, involving 34 people recently diagnosed with type 2 diabetes and who attended an intermediary, multidisciplinary diabetes clinic, was conducted over 2 months.
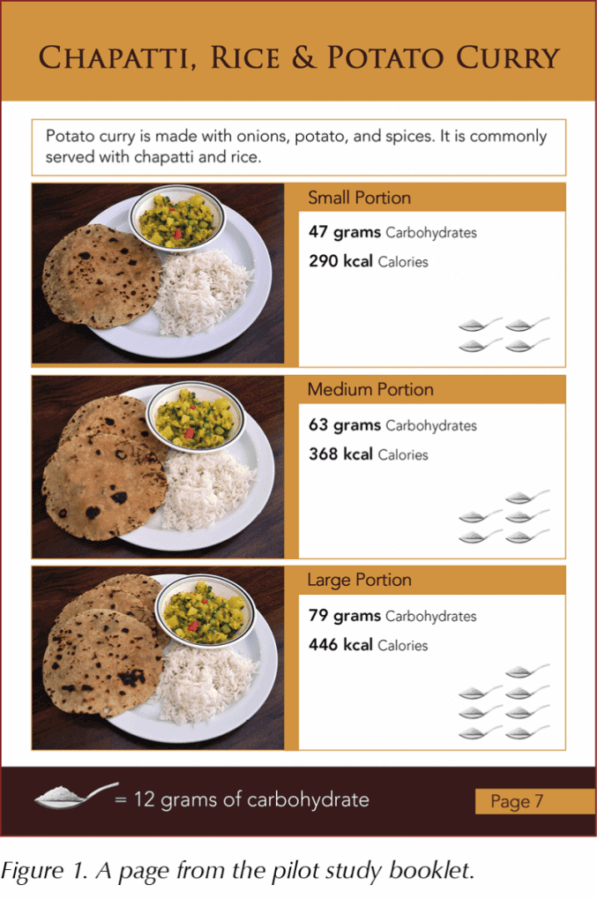
Before any intervention, an investigator worked through a questionnaire with each participant to assess their baseline knowledge and understanding of carbohydrate. They then attended an appointment with a dietitian, during which the booklets were used to inform the individual about the carbohydrate content of the foods that they were eating. Following this session, the participants were taken through the same questions to establish the effectiveness of the intervention.
The results of the pilot study indicated that the majority of the participants did not recall receiving any dietary information prior to the appointment with the dietitian. For those that had received information, 76.5% said that it had not been culturally relevant.
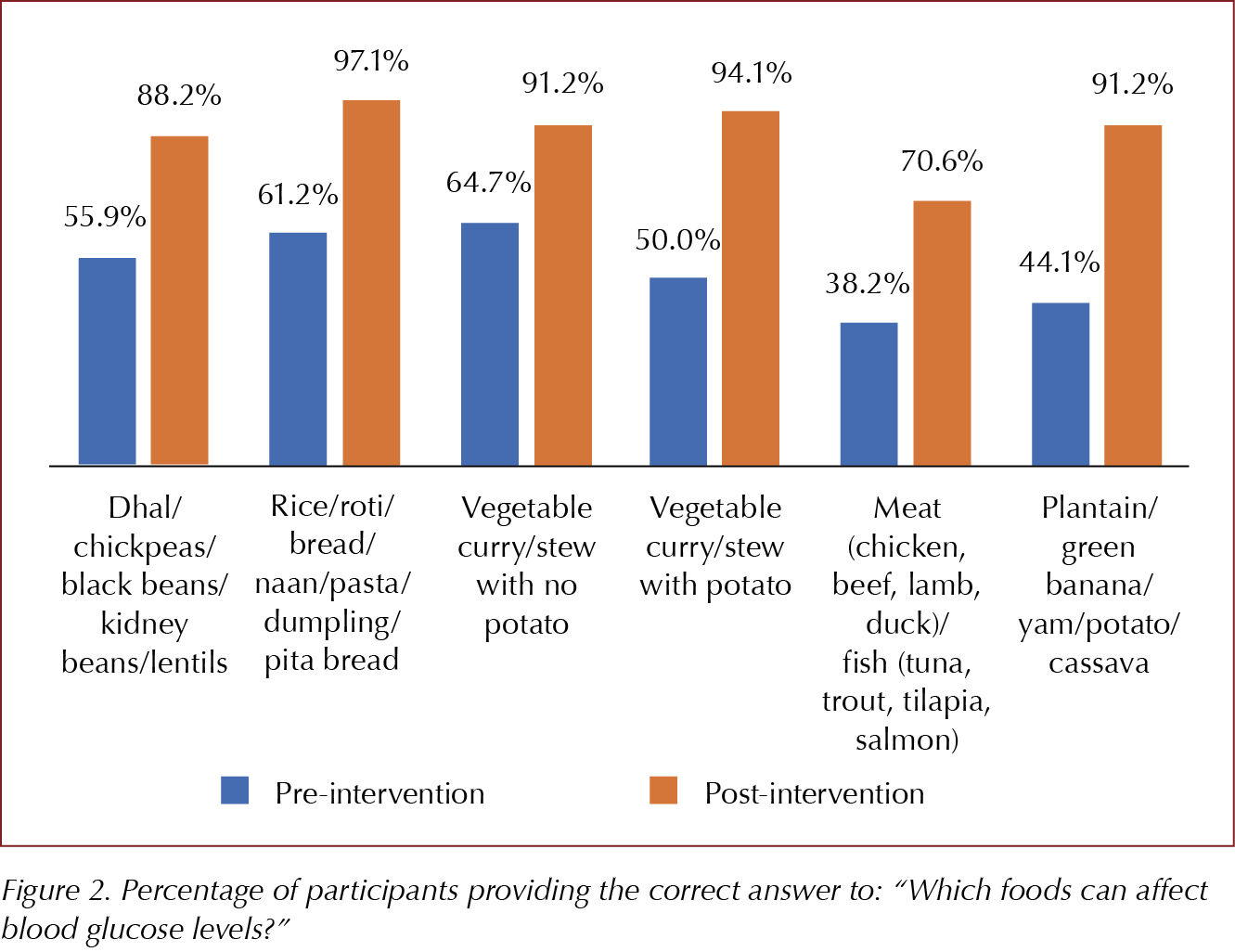
Prior to the intervention, 38.2% of participants could name three carbohydrate (starch) foods that they ate, compared to 100% post-intervention. Using the culturally relevant booklets as a learning resource significantly improved individuals’ knowledge, understanding and ability to estimate the carbohydrate content of traditional and commonly eaten foods within their communities, and enabled greater awareness of carbohydrate and its possible impact on their blood glucose levels (Figure 2). These skills could result in more informed food choices. The cultural relevance of the booklets resonated with the participants, who were keen to retain them afterwards.
Development of a new resource
Brent is part of the North West London Sustainability and Transformation Plan (STP) for Diabetes. This area consists of eight Clinical Commissioning Groups (CCGs) and more than 130000 people living with diabetes. In four of the CCGs, ethnic minorities make up the majority of the population and, in six, BAME communities have a higher prevalence of diabetes than the London average. An element of the plan’s aim to improve diabetes self-management involved developing the booklets to cover four of the largest minority ethnic groups in this area: the African, Arabic, Caribbean and South Asian communities.
To enable informed food choices, it was important to retain the cultural relevance and simple messages of the original booklets, while providing visual representations of the carbohydrate content of food eaten by these communities so that written language would not act as a barrier to understanding. To inform the design of the new resource and to ensure that the right foods were included, surveys were conducted and family food diaries were examined.
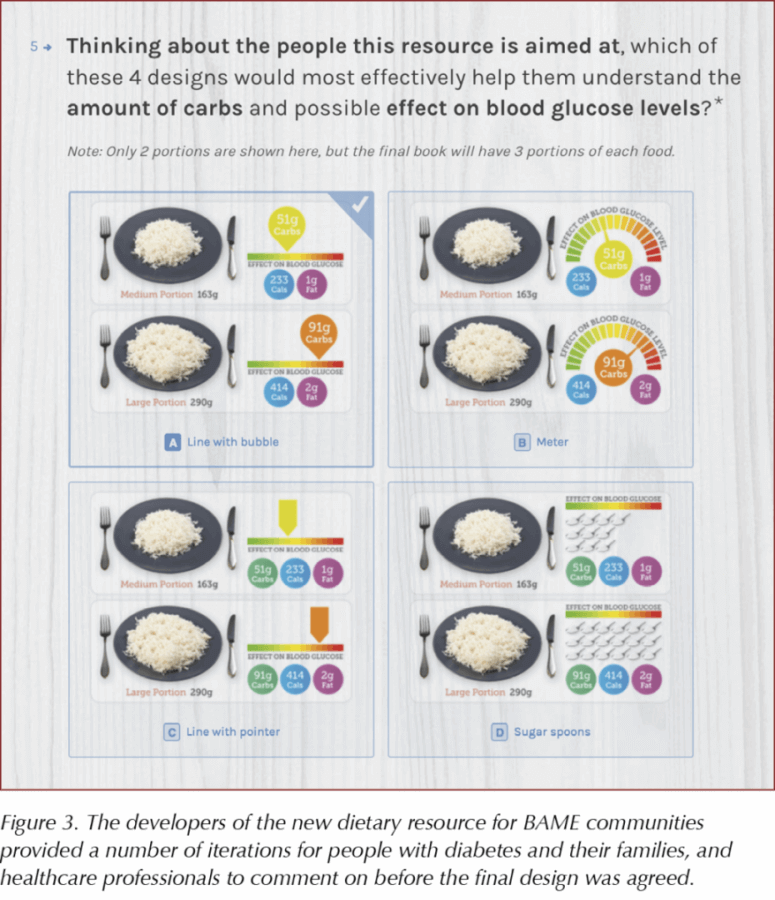
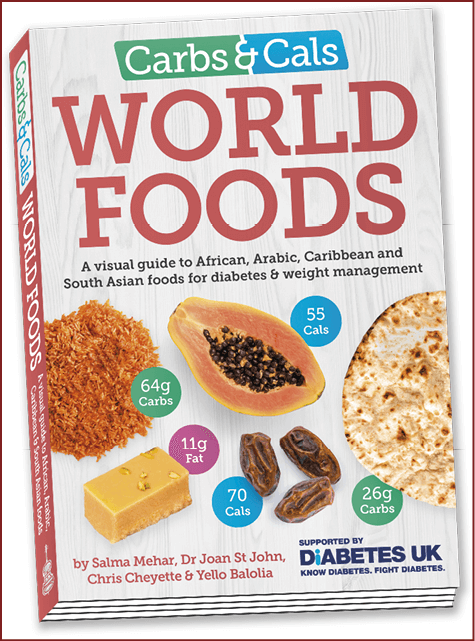
To develop our designs, we worked with the publishers of the Carbs & Cals books and apps, which assist with carbohydrate and calorie counting. After working through a number of design iterations (Figure 3), a book called Carbs & Cals World Foods resulted.
World Foods includes over 700 photographs, highlighting the different foods eaten by people from the four featured communities. Carbohydrate, calorie and fat content information is displayed alongside different portion sizes, while representative icons indicate the effect the food may have on blood glucose. Full meals are included, and snacks and drinks are also incorporated. Foods that are sources of fibre are indicated (Figure 4) to encourage the reader to choose fibre-rich foods for general health. All of the items from the book will be incorporated in the Carbs & Cals app.
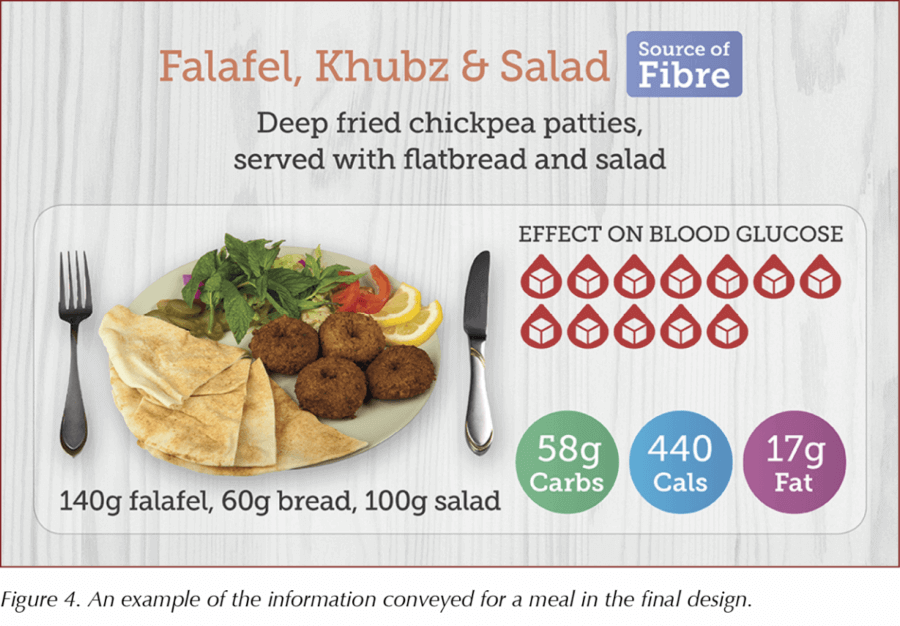
Our intention is to inform people from BAME communities about the carbohydrate content of the food they are eating, but not to dictate what type, or quantity, of food we would recommend. We want to empower them to make healthier food choices, so we have also highlighted some possible food swaps, should people want guidance about how to lower the carbohydrate content of their diet.
The Carbs & Cals World Foods book will be freely distributed to libraries, each GP practice, and all secondary care and intermediary care settings in the NW London STP area.
This resource will provide benefit to those areas with a significant proportion of people from the featured BAME communities, but also to any individual from these communities throughout the UK who needs culturally specific dietary advice.
Conclusions
- BAME communities form a significant part of the population of people living with diabetes in the UK.
- BAME communities have an increased risk of developing type 2 diabetes at a young age (from 25 years old) and a greater risk of developing complications associated with the condition.
- Dietary advice is the cornerstone of management of diabetes and works best when it is culturally relevant.
- A pilot study showed that a culturally relevant booklet with information about the carbohydrate content of food commonly eaten by BAME communities resulted in improved understanding, confidence and ability to estimate the carbohydrate content of the food commonly eaten.
- Keeping the message simple, pictorial, and culturally specific and relevant is important for anyone living with diabetes who may have low health literacy (i.e. not exclusively people from BAME communities) or whose first language is not English.
- The World Foods book was developed by surveying people living with diabetes, their friends and family, and healthcare professionals to ascertain the design that best informs people about the carbohydrate content of food in a pictorial format.
- The book will be freely available in libraries, every GP practice and other healthcare settings in the NW London area. Visit www.carbsandcals.com for information about the book and app.
An outline of the pilot study won first prize in the poster competition at the 14th National Conference of the Primary Care Diabetes Society. To read the poster abstract (P24), go to http://bit.ly/2GBeZ0d





How to minimise loss of muscle mass when using GLP-1-based therapies for weight loss.
26 Mar 2025