People with type 2 diabetes have a two- to four-fold increase in risk of cardiovascular disease (CVD) risk compared to those without the condition (Vergès, 2015) and around half of all deaths in this population are related to CVD (Holman et al, 2008; Preis et al, 2009). Strokes and myocardial infarctions (MIs) are also more likely to be fatal in people with diabetes compared to those without (Betteridge, 2011).
The prevalence of type 2 diabetes has increased dramatically in recent decades (Daniel, 2011) and is paralleled by an increasing incidence of CVD attributable to the condition (Fox et al, 2007).
The increased cardiovascular (CV) risk associated with type 2 diabetes is largely due to diabetic dyslipidaemia (Scicali et al, 2018). This condition is characterised by quantitative, qualitative and kinetic lipoprotein abnormalities, which result in a more atherogenic lipid profile (Vergès, 2015). The main abnormalities are increased triglyceride levels, increased cholesterol-enriched remnant lipoprotein particles and decreased high-density lipoprotein cholesterol (HDL-C) levels (Betteridge, 2011).
Raised triglycerides are a recognised risk factor for CVD. In the PROCAM (Prospective Cardiovascular Münster) study, the risk of CVD increased with the level of triglycerides up to 9 mmol/L, with a lower risk above this value (Assman et al, 1998). While triglyceride levels are usually checked in the fasting state, some evidence suggests that non-fasting triglyceride levels, which reflect post-prandial levels, may be more closely aligned with CVD risk (Bansai et al, 2007; Nordestgaard et al, 2007). Raised triglycerides are not, however, included in the Framingham (http://bit.ly/2M3QIR9), ASSIGN Score (http://assign-score.com/estimate-the-risk) or QRISK®2 and QRISK®3 (https://qrisk.org/2017) risk calculators, so the effect of triglyceride lowering on CV risk reduction has been difficult to quantify.
While total and low-density lipoprotein cholesterol (LDL-C) levels are usually normal in people with type 2 diabetes, the LDL-C particles become smaller, denser and potentially more atherogenic (Betteridge, 2011). These changes may contribute a 3-fold increase in the risk of developing coronary artery disease, owing to the smaller particles’ ability to enter the blood vessels more quickly than the normal, larger, less-dense LDL-C particles, which increases the risk of thrombosis (Cornell and Vito, 2006).
HDL-C levels are inversely related to CVD risk. In the UKPDS (United Kingdom Prospective Diabetes Study), a 0.1 mmol/L increase in HDL-C was associated with a 15% decrease in the risk of coronary artery disease (Turner et al, 1998).
While the pathophysiology of diabetic dyslipidaemia has not been fully elucidated, the insulin resistance and relative insulin deficiency seen in patients with type 2 diabetes, are likely contributors (Vergès, 2015).
Lipid management trials
Numerous clinical studies and meta-analyses have examined the relationship between management of dyslipidaemia and CVD prevention in people with diabetes, the most significant of which will be discussed below.
Secondary prevention
Statins
Statins currently form the cornerstone of lipid-lowering treatment. They work by stopping the liver from making too much cholesterol, while also reducing inflammation and improving the function of vascular endothelial cells.
The role of statins for CVD prevention was initially investigated in secondary prevention studies. The randomised, double-blind, placebo-controlled Scandinavian Simvastatin Survival Study (4S) evaluated the effect of lowering cholesterol with simvastatin (20–40 mg/day) on morbidity and mortality in 4444 patients with coronary heart disease (CHD). Participants were aged 35–70 years, had angina pectoris or previous MI, a serum cholesterol of 5.5–8.0 mmol/L, serum triglycerides ≤2.5 mmol/L and were on a lipid-lowering diet (as defined by the European Atherosclerosis Society [1987]). Over a median 5.4 years of follow-up, simvastatin treatment was associated with a 25% reduction in total cholesterol (TC), a 35% reduction in LDL-C and an 8% increase in HDL-C, with few side effects. 8% of participants in the simvastatin group died versus 12% in the placebo group. Treatment also reduced the risk of myocardial revascularisation procedures by 37% (P<0.00001; Scandinavian Simvastatin Survival Study Group, 1994).
These benefits were assessed specifically in people with diabetes in two subgroup analyses. The first, involving 202 participants with and 4242 without diabetes, confirmed that the simvastatin-related changes in serum lipids were similar between the groups. Both groups experienced significant reductions in major CHD events (relative risk [RR], 0.45 [P=0.002] for those with diabetes versus 0.68 [P<0.0001] for those without) and any atherosclerotic event (RR, 0.63 [P=0.018] for those with diabetes versus 0.74 [P<0.0001] for those without; Pyorälä et al, 1997). However, this may be considered an atypical diabetes population, in light of them having hypercholesterolaemia but low triglyceride levels (Betteridge, 2011).
The second subgroup analysis included additional participants with diabetes, identified via baseline fasting plasma glucose (>7.0 mmol/L), increasing the cohort to 483. It confirmed the previously identified benefits, with simvastatin-treated people with diabetes experiencing significant reductions in major coronary events (RR, 0.58 [P=0.001]) and revascularisations (RR, 0.52 [P=0.005]; Haffner et al, 1999).
These benefits have been confirmed in other long-term studies involving people with diabetes. The CARE (Cholesterol and Recurrent Events) trial compared the effect of pravastatin with placebo in over 4000 individuals, of whom 586 had diabetes. The mean baseline lipid concentrations in the diabetes group (LDL-C 3.5 mmol/L, HDL-C 0.98 mmol/L and triglycerides 1.9 mmol/L) were similar to the general population. Pravastatin reduced LDL-C by 27% and 28% in the diabetes and non-diabetes groups, respectively. It reduced the absolute risk of coronary events in those with and without diabetes by 8.1% and 5.2%, and the relative risk by 25% (P=0.05) and 23% (P<0.001), respectively. It also reduced the risk of revascularisation procedures by 32% (P=0.04) in those with diabetes (Goldberg et al, 1998).
The more recently published randomised, blinded, placebo-controlled LIPID trial investigated secondary prevention of CV events with pravastatin 40 mg/day in 9014 individuals aged 31–75 years with a total cholesterol of 4.0–7.0 mmol/L, including 1077 with diabetes. The responses of blood lipids to pravastatin (reductions in TC, LDL-C and apolipoprotein B, and increases in HDL-C) were very similar between the impaired fasting glucose, normal fasting glucose and diabetes groups, with the exception of triglycerides, which fell most in the diabetes group (Keech et al, 2003). The effect on apolipoprotein B is significant here because this reflects the total number of atherogenic lipoprotein particles and predicts the risk of fatal MI (Walldius et al, 2001; Sniderman et al, 2003). Over a median follow-up of 6 years, in those with diabetes, pravastatin reduced the risk of any cardiovascular event by 21% (P<0.008), the risk of stroke by 39% (P=0.02) and prevented one major CVD event for every 18 people treated (Keech et al, 2003).
These and other secondary prevention trials confirmed that people with diabetes with CHD respond to statin therapy in a similar manner to their counterparts without diabetes, and experience highly significant benefits in terms of a reduced incidence of major vascular events. Furthermore, because those with diabetes are at increased risk of CVD, the absolute benefit of statin therapy is greater in these individuals than in those without the condition (Betteridge, 2011).
Ezetimibe
By inhibiting the absorption of cholesterol, the lipid-lowering compound ezetimibe works in a different way to statins. The double-blind IMPROVE-IT trial investigated whether adding ezetimibe (10 mg) to simvastatin (40 mg) treatment would achieve further reductions in the rate of CV events. It included 18144 participants who had been hospitalised for an acute coronary syndrome within the preceding 10 days. Baseline LDL-C levels ranged between 1.3 and 2.6 mmol/L in those who were receiving lipid-lowering therapy and 1.3 and 3.2 mmol/L in those who were not.
Individuals were randomised to simvastatin plus ezetimibe or simvastatin plus placebo. The primary endpoint was a composite of CV death, non-fatal MI, unstable angina requiring hospitalisation, coronary revascularisation, or non-fatal stroke. Over a median follow-up of 6 years, the median time-weighted LDL-C level was 1.4 mmol/L in the statin–ezetimibe group versus 1.8 mmol/L in the statin monotherapy group (P<0.001). The Kaplan–Meier event rate for the primary endpoint at 7 years, was 32.7% in the statin–ezetimibe groups versus 34.7% in the statin monotherapy group, equating to an absolute risk difference of 2.0 percentage points (HR, 0.94 [P=0.016]). Ezetimibe–statin combination achieved greater reductions in LDL-C versus statin monotherapy, and improved CV outcomes. Lowering LDL-C levels below previous targets provided additional benefit (Cannon et al, 2015).
PCKS9 inhibitors
PCKS9 inhibitors block the action of the PCSK9 proteins to reduce serum LDL-C levels. The randomised placebo-controlled FOURIER trial investigated the efficacy and safety of the PCSK9 inhibitor evolocumab in 27564 people with atherosclerotic disease and LDL-C levels ≥1.8 mmol/L, who were on statin therapy, over a mean follow-up period of 2.2 years. Participants received either evolocumab (140 mg/fortnight or 420 mg/month) or placebo as subcutaneous injections. The primary endpoint was a composite of CV death, MI, stroke, coronary revascularisation or hospitalisation for unstable angina. At 48 weeks, the least squares mean percentage reduction in LDL-C with evolocumab versus placebo was 59%, from a mean baseline value of 2.4 mmol/L to 0.78 mmol/L (P<0.001). Evolocumab also significantly reduced the risk of the primary endpoint versus placebo (9.8% versus 11.3% of participants, respectively; HR, 0.85 [P<0.001]; Sabatine et al, 2017a).
A prespecified analysis of the FOURIER trial investigated the efficacy and safety of evolocumab by diabetes status, and its effect on glycaemia and risk of developing diabetes. At study baseline, 40% of participants had diabetes and 60% did not. The HR for the primary composite endpoint was 0.83 (P=0.0008) for those with diabetes and 0.87 (P=0.0052) for those without. Evolocumab significantly and consistently reduced CV risk in participants with and without diabetes at baseline, without increasing the risk of new-onset diabetes or worsening glycaemia (Sabatine et al, 2017b).
Primary prevention
Statins
The randomised, placebo-controlled Heart Protection Study investigated the cholesterol-lowering effect of simvastatin 40 mg/day in 5963 people with diabetes and 14573 with occlusive arterial disease but no diabetes, who were aged 40–80 years. Both groups experienced a significant reduction, of around 25%, in the first event rate for major coronary events, strokes and revascularisations. There were also highly significant reductions of 33% (P=0.0003) in the 2912 participants with diabetes who did not have any diagnosed occlusive arterial disease at study entry, and 27% (P=0.0007) in the 2426 participants with diabetes who had a pre-treatment LDL-C <3.0 mmol/L. This study provides evidence for the benefits of cholesterol-lowering therapy in people with diabetes, including those without manifest coronary disease or high cholesterol levels. The study authors estimated that in people with diabetes without occlusive arterial disease, using this statin regimen over 5 years could prevent around 45 people per 1000 from having one or more major vascular events (Collins et al, 2003).
The multicentre, randomised, placebo-controlled CARDS study assessed the effectiveness of atorvastatin 10 mg/day for the primary prevention of major CV events specifically in people with diabetes and normal LDL-C levels. It included 2838 participants with type 2 diabetes and no prior history of CVD, who were aged 40–75 years and had an LDL-C level ≤4.14 mmol/L, a fasting triglyceride level ≤6.78 mmol/L and at least one of the following: hypertension, retinopathy, albuminuria or current smoking. The trial was stopped 2 years early, owing to meeting the prespecified early-stopping rule. The median duration of follow-up was 3.9 years. At least one major CV event occurred in 127 people allocated to placebo versus one in 83 allocated to atorvastatin, resulting in a substantial rate reduction of 37% (P=0.001). The risk of stroke was reduced by 48%. There was a 27% reduction in all-cause mortality in the atorvastatin group, but stopping the trial early meant fewer deaths were observed than envisaged. Post-hoc analysis showed that the benefits of statin therapy appeared fairly quickly after starting treatment, with a 33% relative reduction in risk of the primary endpoint at 1 year and 45% at 2 years (P=0.002 at 2 years). The study authors estimated that in people with type 2 diabetes who had no prior history of CVD and normal LDL-C levels, this statin regimen used over 4 years could prevent at least 37 major vascular events per 1000 people. This study confirmed that a particular LDL-C threshold should not be the sole determinant in deciding which individuals with type 2 diabetes should receive statins, and the authors proposed that we should, instead, focus on which people are at sufficiently low risk for this treatment to be withheld (Colhoun et al, 2004).
Meta-analyses
While the primary and secondary prevention trials confirmed that statin therapy reduces the risk of vascular events in people with diabetes, there remained some uncertainty about the effects on certain outcomes and whether these effects were dependent on the type of diabetes, lipid profile or other factors. The Cholesterol Treatment Trialists’ (CTT) Collaborators performed a prospective meta-analysis to investigate this. They analysed data from 14 randomised trials of statin therapy, which included 18686 people with diabetes (1466 type 1 and 17220 type 2) and 71370 people without the condition. Standard-dose statin therapy reduced LDL-C by around 40%, equating to a minimum 1.5 mmol/L reduction for many people with diabetes. Over a mean follow-up of 4.3 years, the people with diabetes experienced a 9% proportional reduction in all-cause mortality per mmol/L reduction in LDL-C (P=0.02), which was similar to the 13% reduction in those without the disease (P<0.0001). Participants with and without diabetes benefited from a significant 21% proportional reduction in major vascular events per mmol/L reduction in LDL-C (P<0.0001).
This study confirmed that in people with diabetes, the proportional effects of statin therapy were similar irrespective of a prior history of vascular disease and other baseline features, including age, sex, type of diabetes, BMI, systolic or diastolic blood pressure, treated hypertension and estimated glomerular filtration rate. The study authors concluded that a statin regimen sufficient to produce a substantial reduction in LDL-C should be considered for all people with diabetes, irrespective of their lipid profile and whether or not they have vascular disease (CTT Collaborators, 2008).
A meta-analysis of 38 trials comparing PCSK9 inhibitors with placebo or active drugs evaluated their effects on glucose metabolism, LDL-C and CV morbidity and mortality in individuals with and without diabetes. It concluded that the PCKS9 inhibitors do not affect glucose metabolism, and their effect on LDL-C and major CV events is similar between those with and without diabetes (Monami et al, 2018).
From trial evidence to clinical practice
Because diabetic dyslipidaemia is a modifiable risk factor for CVD, optimal lipid management is a key component in a multifactorial approach for preventing CVD and CV events (Daniel, 2011).
A heart-healthy lifestyle, including a Mediterranean diet and plenty of exercise, should be recommended to all patients with diabetes.
Prior to starting lipid modification therapy for the primary prevention of CVD, NICE recommends taking at least one non-fasting blood sample for a full lipid profile, including TC, HDL-C, non-HDL-C and triglyceride concentrations (NICE, 2014).
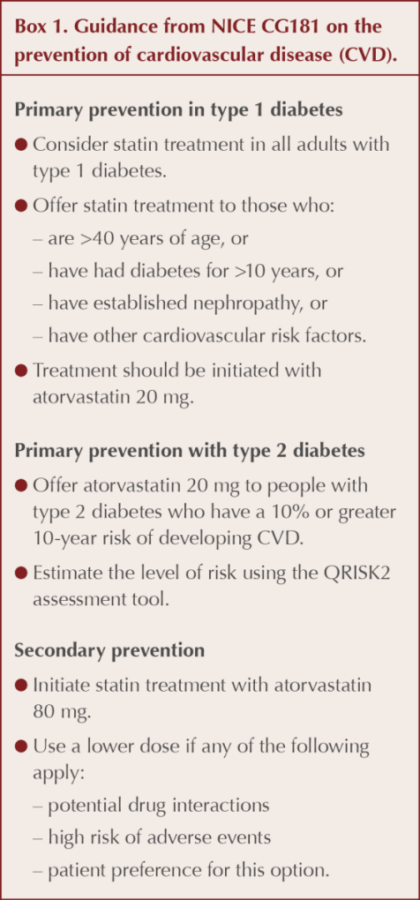
For the primary prevention of CVD, NICE recommends considering statin treatment for all adults with type 1 diabetes and offering it to those who are over 40 years of age, have had diabetes for more than 10 years, have established nephropathy or have other CVD risk factors (NICE, 2014; see Box 1).
For primary prevention in people with type 2 diabetes, NICE recommends offering atorvastatin 20 mg to those with a ≥10% 10-year risk of developing CVD, with their level of risk estimated using the QRISK2 assessment tool (or QRISK3 as it becomes more widely available; NICE, 2014). This treatment threshold, however, is based on cholesterol/HDL-C ratio and does not include triglyceride levels.
For secondary prevention in people with established CVD, NICE recommends that statin treatment is initiated with atorvastatin 80 mg. A lower dose should be used if there is a high risk of adverse effects, the potential for drug interactions, or the patient prefers this option (NICE, 2014). Liver and renal function should be kept under review and contraindications and cautions borne in mind.
Regarding follow-up, NICE recommends that TC, HDL-C and non-HDL-C are measured at 3 months in all people started on any dose of statin treatment (for both primary and secondary prevention, including atorvastatin 20 mg for primary prevention), with treatment aiming for a >40% reduction in non-HDL-C (NICE, 2014).
NICE recommends ezetimibe for primary hypercholesterolaemia (i.e. the presence of high concentrations of cholesterol in the blood associated with an underlying genetic cause) in adults who cannot tolerate statin therapy. It also recommends combining ezetimibe with statin therapy when serum total or LDL-C levels are not appropriately controlled (NICE, 2016a).
In its technology appraisal guidance, NICE recommends the PCSK9 inhibitors alirocumab and evolocumab as potential options for primary hypercholesterolaemia or mixed dyslipidaemia only if LDL-C levels remain persistently >4 mmol/L and >3.5 mmol/L in people at high and very high risk of CVD respectively, despite maximal tolerated lipid-lowering therapy (NICE, 2016b; 2016c).
New American guidelines differ from NICE in their recommendation that people with diabetes who are aged 40–75 years and have an LDL-C ≥1.9 mmol/L can start moderate statin therapy without having their 10-year atherosclerotic CVD (ACVD) risk calculated (Grundy et al, 2018).
They also recommend that in people with diabetes who are at higher risk, especially those aged 50–75 years or with multiple risk factors, high-intensity statin therapy is used to lower LDL-C to ≥50%. In very-high-risk atherosclerotic CVD (ASCVD) patients, an LDL-C threshold of 1.8 mmol/L should be used to consider the addition of non-statins to statin therapy.
Ezetimibe is their drug of choice when LDL-C remains ≥1.8 mmol/L despite maximum tolerated statin therapy, and adding a PCSK9 inhibitor is deemed reasonable when LDL-C remains ≥1.8 mmol/L, despite maximally tolerated statin–ezetimibe therapy, although the long-term safety of this (>3 years) is uncertain.
The guidelines also recommend assessing adherence and response to LDL-C-lowering medication and lifestyle changes with repeat lipid measurement 4–12 weeks after starting statin treatment or dose adjustment, and every 3–12 months thereafter.
While the measurement of serum triglycerides can provide extra information about dietary intake of carbohydrates and additional CV risk, NICE does not recommend specific treatments for raised triglyceride levels. However, the raised levels provide an ideal opportunity to stress a reduction in carbohydrate intake combined with an appropriate daily exercise regimen.
The new American guidelines do include recommendations on the management of hypertriglyceridaemia. These include addressing lifestyle factors, secondary factors and medications that may increase triglyceride levels in people aged >20 years with moderate hypertriglyceridaemia (fasting or non-fasting triglycerides 1.9–5.6 mmol/L), plus initiation or intensification of statin therapy, in people aged 40–70 years with moderate or severe hypertriglyceridaemia (severe defined as fasting triglycerides ≥5.6 mmol/L) and an ASCVD risk ≥7.5%. For people with severe hypertriglyceridaemia (fasting triglycerides ≥5.7 mmol/L), they also advise consumption of omega-3 fatty acids and the use of fibrates to prevent pancreatitis if required, particularly when triglyceride levels are ≥11.3 mmol/L (Grundy et al, 2018). Fenofibrate has been shown to slow the progression of diabetic retinopathy, reducing the need for laser photocoagulation and vitrectomy and, in appropriate patients, should be discussed with the ophthalmology consultant as an option (Morgan et al, 2013).
Regarding omega-3 fatty acids, the UK-based ASCEND trial assessed the effect of these supplements in 15480 people with diabetes but no atherosclerotic disease. The recently published results show that severe vascular events occurred in around 10% of people, regardless of whether they took daily omega-3 capsules or placebo over a 7-year period (ASCEND Study Collaborative Group, 2018). Its findings corroborate those of the recent large Cochrane review, which investigated efficacy of omega-3 fatty acids for the primary and secondary prevention of CVD. The conclusions were that moderate and high-quality evidence suggests that increasing EPA and DHA has little or no effect on mortality and CV health (Abdelhamid et al, 2018). These findings support NICE recommendations that omega-3 fatty acids should not be offered to people with type 1 or type 2 diabetes for the primary or secondary prevention of CVD (NICE, 2014).
However, the recently published REDUCE-IT trial did meet its primary endpoint in a global study of 8179 statin-treated adults with elevated CV risk, demonstrating an approximately 25% RR reduction, to a high degree of statistical significance (P<0.001), in major adverse CV events (MACE) in the intent-to-treat patient population with use of icosapent ethyl 4 g/day, as compared to placebo.
Conclusion
To reduce CVD-related morbidity and mortality in people with type 2 diabetes, a multifaceted approach is required. We need to increase efforts to prevent type 2 diabetes from occurring in the first place, and aggressively treat and control CVD risk factors in those with the condition. Statins currently represent the main treatment for diabetic dyslipidaemia, and have been shown to be well tolerated and safe. Ezetimibe and the PCSK9 inhibitors are additional options. We await more evidence to support the long-term safety of the PCSK9 inhibitors.





SURMOUNT-5 trial pits tirzepatide against semaglutide, plus behaviour change support, for weight loss.
12 May 2025