DiRECT route to type 2 diabetes remission
Mike Lean, Professor of Human Nutrition, Glasgow
- Life expectancy remains significantly reduced by type 2 diabetes, despite management.
- Previous studies have demonstrated that 83% of people with type 2 diabetes achieve remission following the loss of >15% or 15 kg of body weight. A very-low-calorie diet reliably achieves this.
- In the DiRECT study, all blood pressure and diabetes medications were stopped, and 30 minutes’ physical activity daily was aimed for (Lean et al, 2018).
– Stepped food reintroduction.
– Weight loss maintenance, with relapse management if 2 kg of weight is regained.
- Co-primary outcomes from DiRECT:
– Diabetes remission (HbA1c <48 mmol/mol for ≥2 months) in 68/149 (46%) vs 6/149 (4%) in control.
- Criteria for remission (partial or complete) – off all glucose-lowering medication:
• Complete: both HbA1c <6% (42 mmol/mol) and FPG <5.6 mmol/L, off treatment, maintained for 1 year.
- Code “diabetes in remission”, not “diabetes resolved”, so that patient remains on recall registers and receives regular checks.
Resource
- The DiRECT trial: http://bit.ly/2BEvq8N
Diabetes and pregnancy: A primary care focus
David Carty, Consultant Physician, Glasgow
- Stillbirth and perinatal mortality remains 3–5-fold higher in women with diabetes than in those without.
- Amongst women with type 2 diabetes, the National Pregnancy in Diabetes Audit demonstrated that: 42% were not seen in a joint clinic until after 10 weeks’ gestation; only 22% had taken 5 mg folic acid; and only 38% had an HbA1c <48 mmol/mol at conception.
- Discuss pregnancy preparation, where appropriate, at each visit. Pre-conception counselling may have to occur in primary care, but ensure women are seen urgently once pregnancy has been achieved.
- Avoid ACEI/ARBs, SGLT2 inhibitors, GLP-1 receptor agonists (RAs) and statins in women planning pregnancy.
- Flash and continuous glucose monitoring (CGM) can aid tight control and reduce the risk of hypoglycaemic episodes when planning and during pregnancy.
- In the CONCEPTT study of women with type 1 diabetes, CGM resulted in more time in target range, less hyperglycaemia, which translated into fewer large-for-gestational-age babies (53% vs 69%), less neonatal hypoglycaemia (15% vs 28%) and fewer intensive care admissions (27% vs 43%; Feig et al, 2017).
- Gestational diabetes is treated with lifestyle, self-monitoring of blood glucose and metformin. Around half require insulin therapy.
- After gestational diabetes, there is an increased risk of type 2 diabetes (RR, 7.43 [95% CI, 4.8–11.5]), with a doubling of relative risk for each 4.5 kg of weight gain. Weight loss and exercise reduce risk, and, after a fasting glucose test at 6 weeks, an annual HbA1c test is required.
At the heart of diabetes
Kevin Fernando, GPwSI in Diabetes and Medical Education, North Berwick
- The key outcomes from cardiovascular outcomes trials (CVOTs) were discussed by drug class.
- Type 2 diabetes is an independent risk factor for developing heart failure (HF).
• HF with preserved ejection fraction (HFpEF; diastolic HF) is common in diabetes. There are no current treatments to reduce mortality or morbidity. Treat the symptoms.
• Avoid thiazolidinediones (TZDs) at any time in NYHA III/IV.
• Saxagliptin increased hospitalisation for HF in SAVOR-TIMI (Scirica et al, 2013), while a non-significant trend for alogliptin was reported in EXAMINE (White et al, 2013).
- For those with established CV disease:
– The 2018 ADA/EASD consensus report recommends metformin as first-line treatment, then an SGLT2i or GLP-1 RA with CV benefit (Davies et al, 2018).
- The ASCEND (2018) trial found no significant net benefit of low-dose aspirin for primary prevention in those with diabetes.
- Sacubitril/valsartan combination:
– PARADIGM-HR study showed an absolute risk reduction of 5% in CV admissions and death (McMurray et al, 2014).
- PCSK9 inhibitors reduce LDL-C by 60%. Self-administered subcutaneous injection costing £4000 pa.
– ODYSSEY OUTCOMES trial of alirocumab showed a significant reduction in major adverse cardiovascular events (MACE), including in those with diabetes (Schwartz et al, 2018).
Diabetes care for older people
David Strain, Senior Clinical Lecturer, Exeter
- In the UK, 1 in 5 people over the age of 80 have diabetes. This may double over the next 5 years.
- Older people have significant differences in all major systems compared to younger people (e.g. increased body weight is a bad prognostic indicator in younger people, but confers benefit if older).
- Older adults have a lower red cell turnover, and membranes are more friable and prone to glycation. The same average glucose level is, therefore, associated with higher HbA1c.
- Paradoxically, an “average” or “good” HbA1c is associated with lower average glucose. If there is also variability, hypoglycaemia can result.
- Older people with diabetes are at higher risk than those without diabetes:
– Functional disability.
– Geriatric syndromes – depression and cognitive impairment.
- Dementia is increased in those with diabetes, particularly if there is hypoglycaemia.
- Hypoglycaemia is more common in older people and the physiology is different:
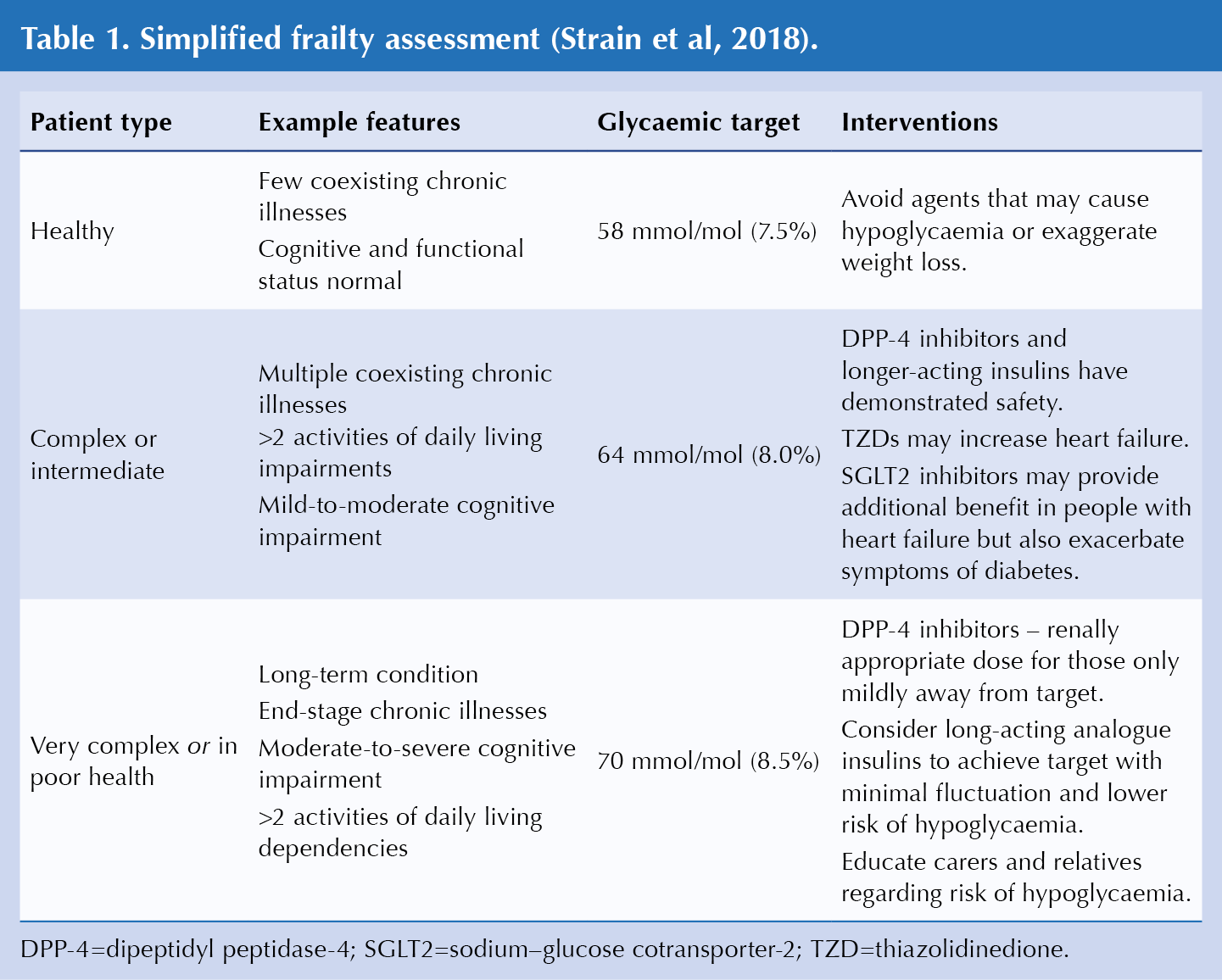
- New a new assessment protocol for the UK includes recommended therapeutic targets based on patient type (Table 1).
- Consider following the “Compelling need to minimize hypoglycaemia” algorithm in the new ADA/EASD consensus on glycaemic treatment (Davies et al, 2018).
- DPP-4 inhibitors in elderly patients have been demonstrated to have a complication rate comparable with younger patients. They are not particularly potent and are relatively well tolerated.
- Some GLP-1 RAs may reduce stroke risk more than other glucose-lowering methods (SUSTAIN-6 demonstrated that semaglutide reduced risk of non-fatal stroke in people with type 2 diabetes; Marso et al, 2016). They are associated with weight loss – the effect on those with sarcopaenia is unknown.
- SGLT2is may be associated with higher stroke risk (empagliflozin). They reduce hospitalisations and delay death from HF (empagliflozin and canagliflozin). They are associated with weight loss, with unknown effect on those with sarcopaenia. They may exacerbate symptoms of diabetes.
- TZDs are associated with fluid retention and HF. They reduce stroke risk (pioglitazone), increase fracture risk and may be associated with bladder cancer. Their effect on those with sarcopaenia is not known.
- Guidance was offered on de-escalation thresholds for each frailty group and which drugs to withdraw first from a safety standpoint.
Diabetes Distilled
Colin Kenny, GP, Dromore
A brief overview of topics not recently covered in the journal.
- No evidence of increased risk of congenital abnormalities when metformin is used in the first trimester of pregnancy, but no evidence of benefit in maternal and fetal outcomes.
- Changes in ACR are an important predictor of development of CV disease, renal disease and all-cause mortality, so it is important to continue to measure it.
- 5.6% of all incident cancers are attributable to diabetes and obesity.
- There is a significant association between HbA1c, diabetes status and long-term cognitive decline.
- A retrospective observational study demonstrated that, at 2 years, adherence was best with metformin, followed by SGLT2is, sulfonlyureas (SUs), DPP-4is and pioglitazone (McGovern et al, 2018).
- The HARMONY CVOT with albiglutide demonstrated a 22% reduction in 3-point MACE (CV death, non-fatal MI or stroke), but there are no plans to launch this drug in the UK (Hernandez et al, 2018).
- The CARMELINA study demonstrated the CV safety of linagliptin, with no increased risk of HF (Rosenstock et al, 2018).
- DECLARE-TIMI CVOT with dapagliflozin was published in November (Wiviott et al, 2018).
- At first intensification in type 2 diabetes, SUs are the commonest drug initiated in England and Scotland, with DPP-4is more common in Wales and Northern Ireland. There has been a shift from use of TZDs and SUs at first intensification to DPP-4is and SGLT2is since 2006.
Masterclasses
Diabetes, cancer and end-of-life care
Paul Newman, GP, Glasgow
- Diabetes can complicate cancer management and some cancer treatments can worsen diabetes (e.g. steroids, chemotherapy).
- Steroids are used as part of chemotherapy to improve side effects, manage cancer symptoms and improve appetite.
- Monitor those at risk of steroid-induced hyperglycaemia and with diabetes. Steroids have more impact on post-prandial glucose; test after meals rather than fasting. HbA1c is not useful for short-term steroid courses.
- Chemotherapy can cause hyperglycaemia, hypoglycaemia (due to vomiting and anorexia) and neuropathy.
- If type 1 diabetes, more frequent monitoring of glucose and ketones is needed. Discuss with specialist team.
- Mood changes are common. Patients may feel alone and frightened.
- End of life (likely to die within 12 months):
- There are four illness stages with specific guidance for each (see link below for more details).
- In the final days, minimise symptoms, invasive testing and treatment. If on insulin, simplify to once daily:
– If >20 mmol/L, increase by 10–20%; if <10 mmol/L, reduce by 10–20%.
- Diabetes UK recommendations on end-of-life diabetes care: http://bit.ly/2X13yEX
Diabetes life hacks
Lyndsey McConnell, GPwSI in Diabetes, Argyll
- Learn about and aim to prevent acute kidney injury (AKI), hyperosmolar hyperglycaemic state and DKA.
- Teach those testing blood ketones how to use the results:
– 1.6–3 mmol/L – give extra insulin and contact diabetes team for guidance.
– >3 mmol/L – urgent, same-day assessment and specialist care.
- Hypoglycaemia – blood glucose <4 mmol/L.
- Sick-day rules – temporarily stop SADMAN drugs (SGLT2is, SUs, ACEIs, diuretics, metformin, ARBs and NSAIDs) to reduce the risk of AKI.
- Admit if persistent vomiting, high glucose, ketones or sepsis.
- What’s new? Oral semaglutide, fast-acting insulin Fiasp, insulin degludec combined with liraglutide, ultra-long-acting insulins, care with high-strength insulins (200 and 300 IU/mL) and biosimilar insulin.
- Think Kidneys resource on restarting medications after an episode of AKI: http://bit.ly/1TNQNqe
Introduction to flash glucose monitoring and continuous glucose monitoring
Brian Kennon, Consultant Diabetologist, Glasgow
- Freestyle Libre is a flash glucose monitoring system that measures interstitial glucose levels.
– SMBG (fingerprick testing) is needed for driving, for confirmation and management of hypoglycaemia, and if unwell.
– Use on airlines may be prohibited, so carry test strips and lancets.
– Various reader reports are available. This technology can help to stabilise glucose levels.
– It is also useful as an educational tool.
- 42 factors can influence blood glucose, but “keep it simple”.
- Use an app (e.g. Carbs & Cals or mySugr) to estimate carbohydrate (CHO) content accurately.
- Common pitfalls in continuous glucose monitoring (CGM): Over-treating hypos; not getting insulin on board 15 minutes before eating; not rotating sites/changing pump sets (lipohypertrophy); persisting with incorrect insulin:CHO ratios, correction factors or basal insulin.
- CGM measures glucose continuously and sends data to the display device without the need to scan. Some fingertip readings are still needed. CGM provides large amounts of data.
- CGM use is approved for frequent, severe hypos, impaired or loss of hypo awareness, and pregnancy.
- Hybrid closed-loop systems use sensor data to alter the insulin dose from the pump.
Resource
- My Diabetes My Way, NHS Scotland. Patients can sign up to access their own test results, clinic letters and treatment plans: http://bit.ly/2UZKl4M
Diabetes and comorbidities
Sarah Davies, GPwSI in Diabetes, Cardiff
Chronic obstructive pulmonary disease
- People with chronic obstructive pulmonary disease (COPD) have increased risk of type 2 diabetes, but the mechanism is unclear. Oral steroids increase diabetes risk and some studies demonstrate increased risk with inhaled steroids.
- Diabetes increases hospital stays, death from exacerbations, multiple sputum pathogens and accelerated decline in those with COPD and diabetes.
Liver disease and NAFLD
- Alcoholic cirrhosis and non-alcoholic fatty liver disease (NAFLD) are the commonest types of liver disease.
- NAFLD ranges from hepatic steatosis, through non-alcoholic steatohepatitis (NASH), to fibrosis/cirrhosis. The prevalence in those with type 2 diabetes is >50%.
- LFTs may be abnormal, but 80% of those with NAFLD have normal LFTs. In those with type 2 diabetes, NAFLD is the most common cause of raised ALT (not statins). Test for other causes of liver disease.
- CVD risk management is important as there is an increased risk of atrial fibrillation (AF), myocardial infarction, ischaemic stroke and CV death in those with type 2 diabetes and NAFLD. Lifestyle advice and management are important.
- Statins can be used in NAFLD if ALT is <3 × the upper-limit normal. Stop if AST/ALT ratio doubles from baseline within 3 months of starting statin.
- In the treatment of NAFLD, pioglitazone, liraglutide and empagliflozin have been demonstrated to decrease liver fat.
Obstructive sleep apnoea (OSA)
- OSA is an independent risk factor for CVD and can cause decreased sleep, resulting in abnormal metabolism and CV function.
- Comorbidities with OSA include drug-resistant hypertension, obesity, HF, pacemaker, AF, all hypertension and coronary artery disease.
- Use the Epworth Sleepiness Scale to identify those who may be at risk, then refer for formal sleep studies.
- Behavioural changes, dental appliances and continuous positive airway pressure (CPAP) are mainstays of treatment. There is no evidence that CPAP improves glycaemic control, but reducing CV risk is the main goal.
Diabetes and mental health
Debbie Cooke, Senior Lecturer, University of Surrey
- The session opened by exploring whether the audience routinely assess for emotional issues in those with diabetes, and how confident they feel asking a patient with diabetes about distress/depression.
- Depression in people with diabetes is three times more common than in the general population (with 1 in 5 affected).
– Glycaemic control is significantly poorer in people with depression and makes self-management more difficult.
- Anxiety disorders are also increased. Little is known about effects on metabolic control.
- It is important to differentiate between depression and diabetes distress:
– Assess using a validated questionnaire, such as the Diabetes Distress Scale-2:
• These two questions are answered on a scale of 1–6. Mean score >3 suggests further assessment.
– Assist in agreeing a joint action plan.
– Arrange more frequent follow-up or support, preferably with a diabetes team, rather than mental health team.
- Prolonged diabetes distress can lead to diabetes burnout – a collection of feelings and behaviours that occur after taking care of diabetes over and over again.
Resources
- NDSS Diabetes and Emotional Health Handbook (for healthcare professionals): http://bit.ly/2IcNahb
- Diabetes UK’s diabetes and mood information prescription: http://bit.ly/2S2YNqS




SURMOUNT-5 trial pits tirzepatide against semaglutide, plus behaviour change support, for weight loss.
12 May 2025