A tsunami of type 2 diabetes is upon us. In the UK, there are approximately 3.7 million people diagnosed with diabetes, a further 1 million with undiagnosed diabetes, and a staggering 12.3 million thought to be at risk of developing the condition (Diabetes UK, 2018a). These numbers have doubled over the last 20 years and, in type 2 diabetes, are set only to increase further owing to the growing prevalence of obesity.
Type 2 diabetes is predominantly a progressive disorder defined by deficits in insulin secretion and action that lead to abnormal glucose metabolism and related metabolic derangements. Significant complications include those that are macrovascular – for example, cardiovascular disease – and those that are microvascular – including nephropathy, retinopathy, neuropathy and erectile dysfunction.
Globally, in 2017, there were 4 million deaths due to diabetes complications (International Diabetes Federation, 2017). This is one death every 8 seconds, despite research demonstrating that these complications can be avoided with early, appropriate lifestyle and medical treatment of all risk factors in type 2 diabetes (King et al, 1999; Gæde et al, 2016). The aim of type 2 diabetes care, therefore, is to give a timely, holistic approach to include not just the management of hyperglycaemia but also cardiovascular and additional risk factors, so that we can add “years to life and life to years”.
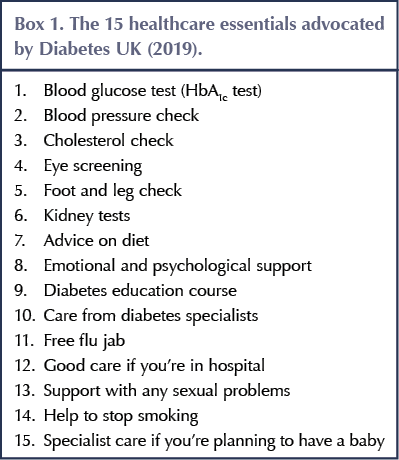
Each person with type 2 diabetes should have a clinical review at least annually, and they are entitled to 15 healthcare essentials, as advocated by Diabetes UK (2019). These essentials are listed in Box 1.
Many annual type 2 diabetes reviews will be conducted by non-diabetes-specialist healthcare professionals. This article is designed to highlight and advise on the basics that healthcare professionals should be aware of to effectively review a person with type 2 diabetes. All of the 15 healthcare essentials will be discussed in order, and there will be an emphasis on signposting to useful resources for both healthcare professionals and individuals with type 2 diabetes to facilitate enhanced learning.
The 15 healthcare essentials
1. HbA1c test: glycaemic review
The NICE (2015a) NG28 guideline recommends that, in adults with type 2 diabetes, HbA1c levels should be measured at 3–6-monthly intervals until they are stable on unchanging therapy, and thereafter at 6-monthly intervals. Note, however, that HbA1c blood tests may not be reliable for certain cohorts, such as those with haemoglobinopathies, severe anaemia and those with HIV. In such cases, there may be a need to use other tests, such as fructosamine levels, in discussion with the local specialist diabetes team.
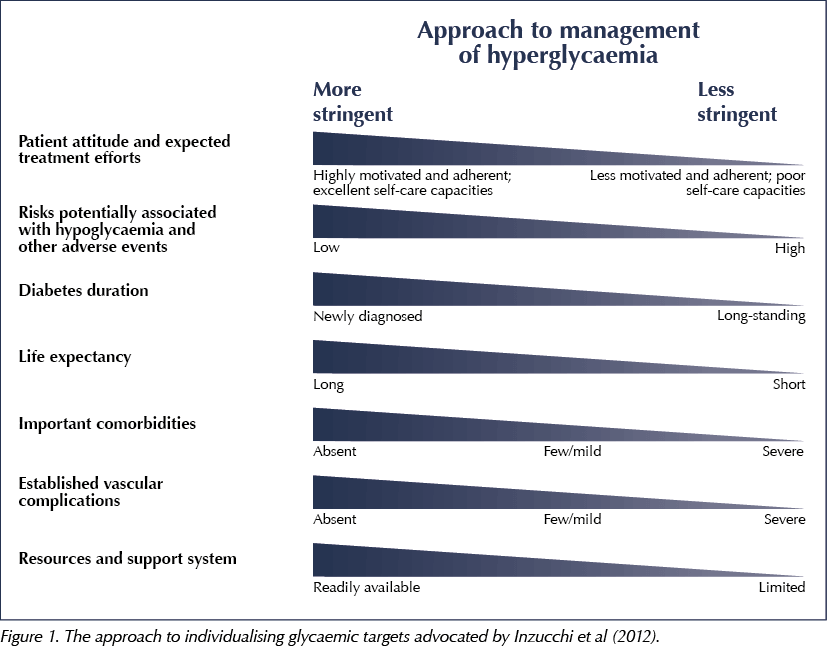
There is debate around optimal HbA1c levels, but most certainly one size does not fit all, and targets should be individualised based on many factors, such as age, duration of diabetes and frailty. A useful approach to individualising HbA1c targets is advocated by Inzucchi et al (2012), and is shown in Figure 1.
The management of those with suboptimally raised HbA1c levels is set out in the NICE (2015a) NG28 guidance and, more recently, in the SIGN 116 guidance (SIGN, 2017) and a joint position statement from the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD; Davies et al, 2018). All current national and global diabetes guidance advocates lifestyle advice with metformin as the first choice of oral therapy, unless contraindicated. Of note, however, is that the newer guidelines, such as SIGN and ADA/EASD, have taken into account the positive cardiovascular outcomes trial data relating to the sodium–glucose cotransporter 2 (SGLT2) inhibitors empagliflozin, canagliflozin and dapagliflozin, and the glucagon-like peptide-1 (GLP-1) receptor agonists liraglutide and semaglutide. The guidelines suggests that, after metformin, the second-line choice for those with a history of atherosclerotic cardiovascular disease or heart failure should be one of these medications. For a brief summary of the ADA/EASD guideline, click here (Down, 2018).
In contrast to intensifying therapies for the treatment of raised blood glucose, there is also a need to consider de-escalating therapies in those who may have lowered HbA1c or are experiencing hypoglycaemia. This is particularly relevant in people prescribed insulin and/or sulfonylureas. Those who are older, frail, have had significant weight loss or are receiving end-of-life care are a notable cohort at risk of overtreatment of hyperglycaemia (Strain et al, 2018). This can contribute to episodes of hypoglycaemia, which has significant implications in terms of quality of life, morbidity and even mortality (Frier et al, 2011).
2. Blood pressure/hypertension review
The treatment of hypertension is the single most effective intervention to reduce the risk of macrovascular complications in type 2 diabetes (Yudkin et al, 2010). A meta-analysis by Ray et al (2009) has shown that, for every 200 people treated over 5 years, reducing blood pressure by 4 mmHg prevented 13 cardiovascular events, compared with eight events by reducing LDL-cholesterol by 1 mmol/L and only two events by reducing HbA1c by 10 mmol/mol (0.9%). Indeed, the landmark UKPDS (UK Prospective Diabetes Study) showed that tight blood pressure control reduced the risk of overall diabetes-related endpoints by 24% (UKPDS Group, 1998).
The pathways for the diagnosis and management of hypertension in diabetes are described in SIGN 116 and NICE CG127 guidance (SIGN, 2010; NICE, 2011). There is growing evidence to support aiming for a blood pressure of <130/80 mmHg (Whelton et al, 2018), and the SIGN guidance recommends this level, while the NICE guidance still recommends a target of <140/90 mmHg. Again, however, blood pressure targets should be individualised, not only to avoid the overtreatment of the frail and elderly, but also to avoid undertreating those with compounding risk factors, such as renal disease, retinopathy, heart failure and a history of stroke.
People who are found to be hyper- or hypotensive should be reviewed monthly (or sooner if the blood pressure is particularly high or low). Lifestyle advice and the titration or de-escalation of medications, in line with NICE/SIGN guidance, until an appropriate blood pressure level has been attained, is indicated for effective management. An angiotensin-converting enzyme (ACE) inhibitor, such as ramipril, is generally the first-line drug of choice in type 2 diabetes unless the person is of African–Caribbean descent or planning to conceive, in which cases a calcium channel blocker (CCB) should be considered (SIGN, 2010; NICE, 2011).
3. Cholesterol/lipid review
Having diabetes doubles the risk of having a heart attack or stroke; therefore, managing lipids is an important component of the diabetes review. The recommended management of lipids is set out in SIGN 116 and NICE CG181 guidance (SIGN, 2010; NICE, 2014a). NICE advocates that, in primary prevention, those with a QRISK2 score above 10% should be offered atorvastatin 20 mg, titrating upwards to achieve a >40% reduction in non-HDL cholesterol. SIGN recommends that all those with type 2 diabetes aged >40 years be offered simvastatin 40 mg or atorvastatin 10 mg. In secondary prevention, both guidelines recommend atorvastatin 80 mg, if tolerated.
Of concern is that, although cardiovascular disease is the most common cause of death in diabetes, in a recent survey of those with and without a link to diabetes, only 2% spontaneously said that stroke was a complication of the condition, and only 6% mentioned heart attacks (Diabetes UK, 2018b). There is a clear education piece missing about the association of complications with diabetes, which underlines the need to convey the seriousness of diabetes and its potential consequences, whilst being mindful to present a positive view that, with lifestyle modification and correct medical management, these complications can be minimised or prevented.
4. Eye/retinopathy screening
Diabetes is the leading cause of preventable sight loss in the UK. All those living with diabetes should receive annual retinal screening by an optometrist or ophthalmologist. It is important that we promote the importance of this at the diabetes review, but also that we manage other risk factors, such as smoking, hypertension and blood glucose levels, so that retinopathy might be prevented or its trajectory changed.
Diabetic retinopathy is classified in four stages: background, pre-proliferative, proliferative and maculopathy. Early detection and treatment of retinopathy is vital in halting this progression.
5. Foot and leg check
Diabetes leads to 169 amputations every week, which equates to 24 amputations a day, or one per hour; however, only 25% of people with diabetes in the Diabetes UK (2018b) survey said that foot problems could be a complication of diabetes. Clearly, again, this demonstrates the need not only to perform a foot assessment (checking for appearance, foot pulses, monofilament wire and vibration sensations) but also the need to educate the person in front of us that diabetes can cause major foot problems, and to promote the importance of looking after their feet, being aware of any signs for concern and knowing what to do if such signs are present.
Each area should have a relevant pathway for foot referrals to podiatry based on whether the foot is deemed to be low-, moderate- or high-risk. Immediate referral to a footcare specialist is vital for those with infection, active ulceration or suspected Charcot foot. There is a wealth of resources from Diabetes UK on foot care, including Information Prescriptions, which have been separated into advice for the effective management of low- and moderate/high-risk feet.
Full guidance on diabetes foot care and the management of painful neuropathy is described within SIGN 116 (SIGN, 2010) and NICE NG19 and CG173 guidance (NICE, 2013; 2015b). The foot examination is not easily learnt from a text book; however, NHS Scotland has some good illustrative modules, including videos on how to physically check the foot (available at: www.diabetesframe.org).
6. Renal assessment
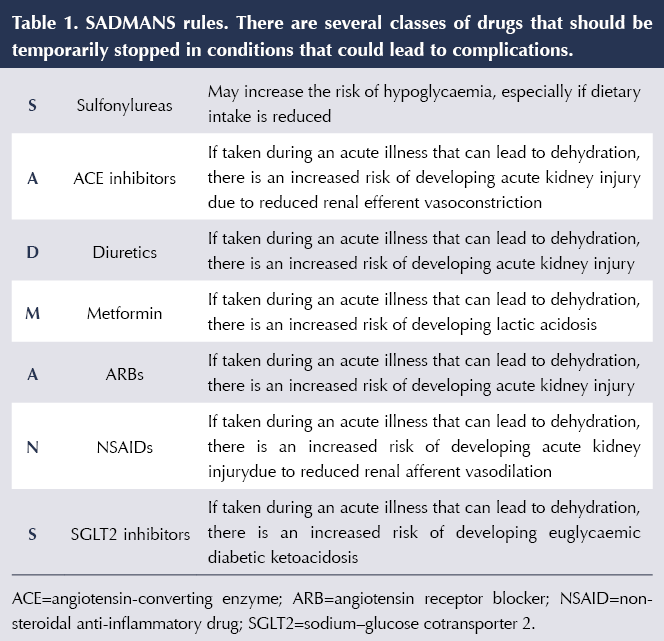
People who have diabetes in addition to chronic kidney disease (CKD) have an approximately 50% higher risk of end-stage renal disease, cardiovascular complications and death than those at a similar level of renal disease without diabetes. Therefore, assessment and management of estimated glomerular filtration rate (eGFR) and urinary microalbumin levels are a significant element of the diabetes review. Reducing other risk factors for cardiovascular disease (e.g. lipids, blood pressure and unhealthy lifestyle) in this cohort is vital. Prescribing safely and the importance of conveying sick day guidance to avoid acute kidney injury should be part of the diabetes review. A useful acronym for the medications that may need to be temporarily stopped during illness is SADMANS, as shown in Table 1. Once the person is feeling better and able to eat and drink for 24–48 hours, these medications should be restarted.
In addition to SIGN 116 and NICE CG182 guidance (SIGN, 2010; NICE, 2014b), helpful resources on the diagnosis and management of CKD include the “How to” series published in Diabetes & Primary Care (Gadsby, 2017; Diggle, 2017). In this series there are step-by-step algorithms which can be printed out and laminated to help the busy practitioner in effectively diagnosing and managing CKD in terms of eGFR and microalbuminuria. There are also many patient and healthcare professional resources produced by Kidney Care UK and the Think Kidneys organisation.
All those with CKD stage ≥3 and/or confirmed positive urine microalbumin should be offered a statin without the need for a QRISK2 score, and should be offered an ACE inhibitor such as ramipril or, if this is not tolerated, an angiotensin receptor blocker (ARB).
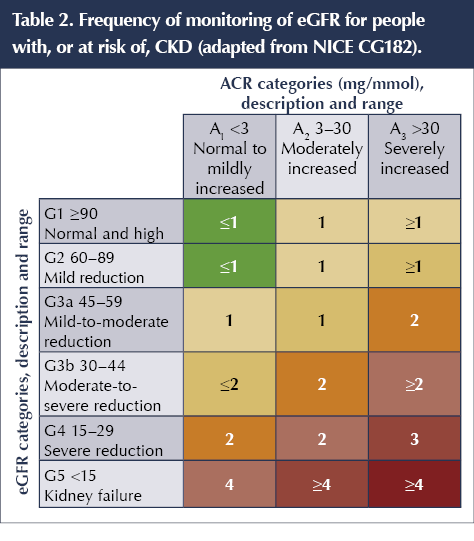
A useful chart outlining the frequency of measuring and reviewing eGFR in those with diabetic kidney disease can be found in Table 2 (NICE, 2014b).
7. Diet and lifestyle advice
As with all long-term conditions, the backbone of the diabetes review needs to be the delivery of appropriate and tailored lifestyle advice. This has gathered momentum recently with the results of the DiRECT study (Lean et al, 2018), which has demonstrated the possibility of halting the progression of type 2 diabetes and even inducing remission, by use of a calorie-restricted diet. NHS England has recently announced funding for pilot sites to offer very-low-calorie diets for people with type 2 diabetes, and findings from these interventions, including their sustainability, will be eagerly awaited. Currently, however, a search on social media sites will lead to an array of conflicting advice about diets and activity schedules advocated for the prevention, remission and treatment of type 2 diabetes. It is important that we give advice to people with diabetes based on evidence, and that we signpost those in our care to trusted sources, such as the recently published Diabetes UK dietary guidelines (Twenefour et al, 2018), so that people can make appropriate and safe lifestyle changes.
Dietary foundation stones are to look at portion sizes and foods advocated in Mediterranean-style diets, such as increased vegetables, fruits, whole grains, fish, nuts and pulses, and to eat less red and processed meat, refined carbohydrates and sugar-sweetened beverages. Reduced salt intake is also important. A Mediterranean meal plan is available from Diabetes UK at: https://bit.ly/2IrY1Tv.
Any increased activity is beneficial, and this needs to be individualised based on a person’s physical ability. It is suggested that 150 minutes of moderate exercise per week, including aerobic and resistance activities, with no more than two days lapsing without exercise, be encouraged (Colberg et al, 2016).
8. Emotional and psychological support
Unlocking the key to behaviour change and evoking lifestyle adjustment is reliant on the engagement of the person with diabetes. Factors such as diabetes distress, anxiety and depression can thwart such engagement and often result in non-attendance at reviews, difficulty in following lifestyle advice and not taking medications as prescribed. The prevalence of depression is approximately twice as high in people with diabetes as in the general population (Kreider et al, 2017). The language we use in talking about diabetes is important, and NHS England (2018) has recently published a document which can help healthcare professionals in achieving effective conversations in diabetes (available at: https://bit.ly/2tpAmt9).
It is important to assess for any emotional and psychological factors, and to signpost to services and other healthcare professionals that can help to manage these effectively. There is growing evidence around the use of “social prescribing” in type 2 diabetes (NHS England, 2014). This encourages people to engage with activities such as walking and cycling clubs and gardening and knitting groups, which aid with social interactions and can be particularly helpful for those experiencing low motivation levels and loneliness.
9. Access to diabetes education
It is estimated that a person with diabetes will spend at most 2–3 hours a year with their healthcare professional; for the remaining 8757 hours of the year, they are on their own. With less than 10% of people attending formal diabetes structured education (Diabetes UK, 2017a), due to a variety of barriers, we need to consistently incorporate education within the diabetes review to ensure that the seriousness of long-term complications is conveyed, alongside the benefits of effective self-care and management. The use of resources such as Diabetes UK’s Information Prescriptions and their recent Be in the Know tools are an excellent way of facilitating this and signposting not just the person with diabetes but also their families and carers to further information and support.
The recently published NHS 10-year plan (NHS England, 2019) has diabetes education high on its priorities, and it includes the pledge to “expand the provision of structured education and digital self-management support tools”. An example of a digital app demonstrating positive outcomes is My Diabetes My Way, which is offered throughout Scotland with an uptake of 10% of the population. NHS England also has a webpage listing approved digital apps that are appropriate for people with type 2 diabetes (available at: https://apps.beta.nhs.uk/category/diabetes).
10. Care from diabetes specialists
The realisation of limitations in knowledge, skills and experience when caring for people with diabetes is paramount. Type 2 diabetes can predominantly be managed in primary care, but there are times when referral to diabetes specialist teams may be indicated. Diabetes care models such as the Portsmouth Super Six (Nicholson et al, 2016) have set out such circumstances, and these are generally inpatient care; antenatal diabetes; poorly controlled type 1 diabetes, including adolescents; low eGFR and people on dialysis; foot complications; and insulin pump services.
11. Influenza and pneumococcal vaccinations
People with diabetes should be offered an influenza vaccination annually and a pneumococcal vaccination as a one-off unless they meet the criteria for more frequent pneumococcal vaccination (Public Health England, 2018). People with diabetes are at increased risk of developing severe complications after influenza virus infection, with three times the likelihood of hospitalisation and four times the risk of intensive care admission once hospitalised (Allard et al, 2010; Hulme et al, 2017).
12. Good care in hospital
One in five inpatients with diabetes will have an episode of hypoglycaemia during their hospital stay. Almost 46% of inpatients will have a medication error related to their diabetes medication and a quarter with type 1 diabetes will develop diabetic ketoacidosis after undertreatment with insulin (Diabetes UK, 2017b). This serves to underline the theme throughout this article of encouraging self-ownership of diabetes so that individuals are empowered to better care for themselves, in the hope that such startling inpatient statistics will see an improvement. Specific advice is available on how to prepare for hospital admission and surgery (Dhatariya, 2018).
13. Support with any sexual problems
Discussion of erectile dysfunction can be difficult to initiate; however, it is estimated that 35–90% of men with diabetes globally are affected by erectile dysfunction, and 27% of women with type 1 diabetes report sexual dysfunction (Enzlin et al, 2003; Malavige and Levy, 2009). Identification of reversible or modifiable risk factors, including lifestyle or drug-related influences in men, is described in a NICE (2017) Clinical Knowledge Summary. The summary also provides guidance on management, to include pharmacological treatment.
It is relevant to advise that erectile dysfunction can respond well to a combination of lifestyle changes and drug treatment, advocating, where appropriate, weight loss, smoking cessation, reduced alcohol consumption, improving HbA1c and increasing physical activity. In women, this area is poorly researched and guidance is welcomed. Psychosexual counselling may also be of benefit.
14. Help to stop smoking
It has been evident throughout this article that smoking cessation is of paramount importance in reducing risk factors relating to the long-term complications of diabetes. Encouragement and support with smoking cessation is significant and highly beneficial. There are a vast array of services to help with smoking cessation available from the NHS.
15. Specialist care for those planning to have a baby
Preconception advice for women of child-bearing age is an important consideration at the diabetes review, as only around 8% of women with diabetes are adequately prepared for pregnancy (Diabetes UK, 2015). Women should be advised to aim for a HbA1c of <48 mmol/mol (6.5%), take folic acid at the prescription-only strength of 5 mg daily and have a medication review to suspend any medications that may be teratogenic. With regard to antidiabetes medications, only metformin and insulin are thought to be safe to use in preconception and pregnancy (NICE, 2015c).
Medication review
Although not specified in the Diabetes UK list of essentials, medication review is clearly a crucial part of the annual review. In reviewing medications, particularly when intensifying treatment, it is always important to look back and assess which medications have been effective, and to be alert to stopping those which are ineffective. Some studies suggest that up to a third of people with type 2 diabetes do not take their prescribed diabetes medications (McGovern et al, 2018), so it is useful to ascertain which ones are actually being taken.
As previously discussed, always be observant for any overtreatment of conditions such as hyperglycaemia and hypertension, especially in the frail and/or elderly, and consider de-escalation of medications in these circumstances. We have already discussed sick day guidance and medications to suspend when unwell/susceptible to dehydration.
Those taking medications that can induce hypoglycaemia (i.e. sulfonylureas, prandial glucose regulators and insulin) will need special consideration, with discussion of hypoglycaemia and its prevention, signs, symptoms and management. A patient information leaflet on hypoglycaemia is available for free from TREND-UK (2018) at: https://bit.ly/2WzlXZ9. It is also essential to discuss DVLA (2018) regulations on driving and hypoglycaemia and to support access to capillary blood glucose monitoring. A how-to guide on assessing fitness to drive is available from Brown and Diggle (2017). Review of glucose self-monitoring, including when it is required, correct technique, timing, interpretation of results and actions to take depending on levels, should be undertaken at least annually (TREND-UK, 2017).
Those taking injectable therapies, such as GLP-1 receptor agonists and insulin, should be reminded about the storage, disposal, preparation and timing of their injections, and observation and palpation of injection sites is relevant in ensuring correct injection technique and site rotation to avoid the formation of areas of lypohypertrophy (Injection Technique Matters, 2018).
Summary
This has been a whistle-stop tour of the diabetes review, with signposts to numerous useful resources looking at specific areas in greater detail. There is much to consider, but hopefully this article has highlighted the need for a multifactorial approach in effective diabetes management, not just the management of blood glucose and HbA1c levels. As we tackle the type 2 diabetes tsunami before us, never forget the very basics of Engagement, Education, Enablement and Empowerment, in order that healthcare professionals and those in our care, including their families and carers, may learn to surf the tidal wave with confidence!





Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024