Rory is a 63-year-old lecturer in bio-chemistry at a Scottish university. Two weeks ago, he was admitted to a hospital with an ST-elevation myocardial infarction, which was complicated by an episode of heart failure. He has had coronary angiography carried out, which confirmed triple vessel coronary artery disease, and he had two coronary artery stents inserted.
During his admission, type 2 diabetes was diagnosed, although he has no symptoms. He has comes to see his GP with a hospital discharge letter.
His weight is 97 kg, with a BMI of 30.6 kg/m2. His HbA1c was 76 mmol/mmol (9.1%) in hospital and his average blood pressure over three readings was 157/91 mmHg. He is a non-smoker, having given up a 20-per-day habit in his mid 40s, and he has 1–2 glasses of wine each evening.
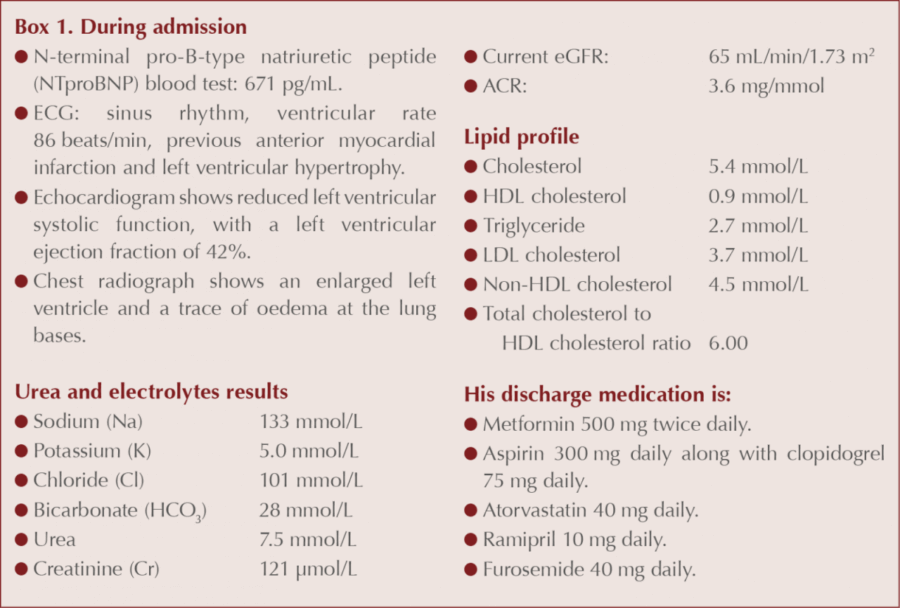
You note also the information provided in the hospital’s discharge letter (see Box 1).
During the consultation, Rory asks:
- Do I really have type 2 diabetes?
- Do I need all this medication?
- They want me to do an exercise programme. Is that wise?
- What are the best evidence-based interventions for me?
How would you respond? Take a few moments to reflect on the information provided, then read on to find out how three healthcare professionals would approach the different aspects of this complex case.
The clinicians’ perspectives
Lifestyle and physical activity (Gwen Hall)
I seem to meet this fellow regularly in clinic, or many like him. Without the person in front of me, it is difficult to comment without making generalisations. However, first and foremost, the aim must be to find out what the individual feels about his health and to work with him on improving it.
The question that is relevant to my comment on lifestyle and physical activity is around the wisdom of an exercise programme. So, is it wise in his case?
Following a myocardial infarction, the British Heart Foundation (https://bit.ly/2L4aSg2) suggests:
I love their table of activity! Take weeks 1–4 and see how much of it might apply to our individual:
Then:
Aim to be exercising for 15–20 minutes at a time by weeks four to six. By this time you should also have started attending cardiac rehabilitation sessions.
But we don’t know what he was doing before. His BMI may suggest “not a lot”, but it is a crude measure and doesn’t account for muscle mass. In my area, we have not only cardiac rehabilitation but also a very well run activity programme. Note I say physical activity, not exercise. It is not necessary to attend a gym for “exercise”. Any physical activity, gently introduced, will be beneficial. Find out what he likes. What motivates him?
While discussing this, I would like to address some other lifestyle issues. Whilst it is not appropriate to use cardiovascular risk assessment tools like QRISK®3 calculator (https://qrisk.org), because he has already had a heart attack, you can use them to show the benefit of other changes he can effect. By effective use of antihypertensive medication, which answers part of another of his questions, he could reduce his blood pressure to acceptable levels, thereby improving his risk. Weight loss would further reduce his risk.
Perhaps in discussion I would try to establish the following: Does he know the number of calories in those wine glasses? Realistically, what size are they? What is their alcoholic strength? There is a useful calculator on drinkaware.co.uk. Two 175-mL glasses of 13% ABV wine=318 calories per day. There are savings to be made even before discussing the rest of his diet.
In practice, I would cover the basics of a healthy diet, with his family if possible, with finer detail covered by the dietitian in the cardiac rehab programme. Hopefully, in no more than 3 months, the HbA1c result will confirm he has reached his target level. Again, I would try to seek to include the family, if possible. The important thing is to work closely with the individual, who will be feeling quite stressed, and to support him in whatever way he chooses.
Diabetes diagnosis and cardiovascular care (Nigel Campbell)
We like to think that we don’t see a presentation like Rory’s now, given all the health screening and health checks that we do in primary care. Rory reminds us that, for all the worried well who come, there are people out there who pay little heed to their health until crisis hits. Sadly, we still have many patients who present post crisis.
There are many things to discuss, but it seems Rory is stuck at the point where he doubts he has diabetes. In the absence of symptoms, many patients do find the diagnosis difficult to accept and the whole consultation may be taken up just trying to get Rory to come to terms with this one issue, never mind the rest. At the other end of the spectrum are the people who want to cover all issues in the one consultation. Communication will be the key in getting Rory on board.
Rory’s diagnosis of diabetes seems certain given the HbA1c level recorded. However, since he is asymptomatic, the laboratory venous HbA1c test should be repeated to exclude the possibility of error. Remember to tell the laboratory that the repeat is to confirm or refute the diagnosis; otherwise they may decline to retest. Explaining the natural history of diabetes may enable him to grasp the nature of the condition and its implications. The association with coronary artery disease does not surprise us, as this is the chief enemy of our patients with type 2 diabetes, but no doubt Rory has been shocked.
From having no medication to being told you need to take seven pills per day may stretch Rory beyond what he’s comfortable with. All are necessary, however, and it reminds us that in type 2 diabetes our patients can end up on multiple medications. Adherence will need to be checked and compromise reached if Rory seems unwilling to take so many tablets.
Rory’s fear of exercise is common in those who have had a cardiac event. The importance of cardiac rehabilitation should be emphasised and he should be referred for this, if it isn’t already arranged. Likewise, he should be attending a heart failure clinic for adjustment to his medication. I do wonder why he isn’t taking a beta blocker. Added to this is the need for weight loss, alteration to his diet and moderation in his alcohol intake.
Rory will need ongoing support from his primary healthcare team and careful management of his comorbidities.
Evidence base for therapy (Patrick Holmes)
Does Rory really have diabetes?
It looks as though the diagnosis was based on a single elevated HbA1c, taken in hospital whilst being treated for an acute coronary syndrome. Rory does not have symptoms of diabetes, according to the World Health Organization (http://bit.ly/2vGR5Kx). In an asymptomatic person, two tests need to be undertaken prior to diagnosis, both of 48 mmol/mol (6.5%) or above. There is no indication of an alternative explanation for the elevated HbA1c and it seems highly likely that Rory does have diabetes. If he really is asymptomatic, a second sample should be taken at the earliest opportunity to confirm the diagnosis.
Does he need all this medication?
Rory has had an ST-elevated acute myocardial infarction (STEMI), with evidence (raised pro-BNP and ECHO findings) of left ventricular systolic dysfunction (LVSD). Based on NICE guidance (NICE, 2013; 2014), he should be offered dual antiplatelet therapy, a statin, an ACE inhibitor, eplerenone and a beta-blocker.
The same guidance would recommend the choice of antiplatelet drug as low-dose aspirin indefinitely (e.g. 75 mg) in combination with ticagrelor (or prasugrel) for at least 12 months in view of the insertion of two coronary stents, rather than his current regimen.
The statin recommended in the guidelines is atorvastatin 80 mg per day. It is unclear why Rory was prescribed only 40 mg. Lower doses should be considered if there are potential drug interactions, if the patient is at high risk of adverse effects or because of patient preference.
The dose of the ACE inhibitor (ramipril) prescribed appears appropriate.
He is not on either eplerenone or a beta-blocker.
Furosemide, as a loop diuretic, should be titrated up or down to treat symptoms of heart failure (NICE, 2010). Assuming there are currently no signs or symptoms of heart failure, this could be reduced or even stopped.
Rory’s current dose of metformin is a reasonable addition, based on NICE guidance (NICE, 2017). He is at an increased risk of lactic acidosis in view of the LVSD. Further dose escalation should be considered over the coming weeks.
Is an exercise programme wise?
Absolutely. There is evidence to show that cardiac rehabilitation with an exercise programme reduces mortality by 25% compared with a 13% reduction when cardiac rehabilitation is not accompanied by an exercise component (Lawler et al, 2011). The inclusion of an exercise programme also results in an improved quality of life (Heran et al, 2011).
What are the best evidence-based interventions for Rory?
Given the fact that Rory has recently had a STEMI with evidence of LVSD, probably has diabetes, has an elevated BP and may be developing early evidence of renal disease (reduced eGFR and elevated ACR), he is at a high risk of a subsequent further cardiovascular (CV) event and CV death. He would benefit from optimal treatment of his CV disease and risk factors for a further event.
Cardiac rehabilitation that includes an exercise component demonstrates good evidence of benefit. Optimally, treating Rory’s post-myocardial LVSD with beta-blockers, eplerenone and ramipril will reduce his mortality risk with the addition of each therapy.
In terms of antiplatelet therapy, low-dose aspirin plus ticagrelor or prasugrel reduces mortality compared with aspirin plus a clopidogrel regimen (Wiviott et al, 2007; Wallentin et al, 2009).
Statin therapy following MI reduces mortality, with atorvastatin 80 mg remaining the gold standard dose for higher risk patients.
Rory appears to have three risk factors that are not optimally managed: his BP, dysglycaemia and possibly impaired renal function. With regard to his BP, the introduction of beta-blockers and eplerenone are likely to help reduce it. The optimal target remains controversial. The consensus is to reduce systolic BP to 140 mmHg. Although reducing this further may further reduce CV events, it introduces harms such as falls and adverse renal outcomes without reducing overall mortality (de Boer et al, 2018).
For the dysglycaemia, it is likely that he will need treatment in addition to the metformin. CV outcome trials using glucose-lowering agents have demonstrated a clear benefit with SGLT2 inhibitors and certain GLP-1 receptor agonists (most notably liraglutide and semaglutide), when added to metformin. In those with established CV disease, mortality appears to be reduced the most with SGLT2 inhibitors (Zheng et al, 2018). However, in view of the use of furosemide, some caution needs to be employed before adding an SGLT2 inhibitor (Wilding et al, 2018) to avoid over-diuresis. Metformin monotherapy was shown in the UK Prospective Diabetes Study (UKPDS) to reduce mortality and MI when used in overweight people as initial therapy (UKPDS, 1998).
With the possibility of impaired renal function being present, ACR and eGFR tests need to be repeated (see http://bit.ly/2zRqtZU and http://bit.ly/2OC3lGZ). If the ACR confirms persistent albuminuria, then there is evidence that an SGLT2 inhibitor may slow the rate of decline in eGFR (Warren et al, 2018).
We are grateful to the three contributors who analysed and responded to this patient’s queries from their own perspectives. All felt disappointed that the patient had evolved to this stage without previous input from the primary care team on diagnosis of his diabetes and other risk factors. All would encourage him to accept the diagnosis of diabetes when confirmed.
Key learning points from Rory’s presentation
- Cardiac rehabilitation that includes an exercise component is an important evidence-based intervention to reduce future risk.
- Diet and alcohol intake as well as other lifestyle issues need to discussed realistically, but sensitively, both during practice visits and in the cardiac rehabilitation programme.
- Rory may be developing early diabetic renal disease and, if confirmed, will further increase his cardiovascular risk, so follow up albumin–creatinine ratio (ACR) and eGFR tests are important. How to… guides on using ACR and how to diagnose CKD are available at http://bit.ly/2zRqtZU and http://bit.ly/2OC3lGZ).
- All recognised the patient’s concern at this sudden pill burden, and additional medication, such as beta-blocker and increased statin, is likely. Adherence should be addressed at each consultation.
- The use of SGLT2 inhibitors and GLP-1 receptor agonists with evidence for benefit in those with established cardiovascular disease (CVD) should be considered as second-line glucose-lowering medication in people such as Rory. This has been formalised in the new ADA/EASD guideline which can be accessed at https://doi.org/10.2337/dci18-0033.
Follow-up monitoring of all aspects of Rory’s care will be vital in keeping him motivated to reduce his future CVD risk.






The mortality benefits of smoking cessation may be greater and accrue more rapidly than previously understood.
2 Apr 2024