People with diabetes have a life-time risk of vascular events that is two to three times as high as the risk among those without diabetes (Emerging Risk Factors Collaboration et al, 2010). People living with diabetes often die prematurely from atherosclerotic cardiovascular disease (ASCVD), and risk factors associated with this should to be addressed, with blood pressure, lipids and blood glucose levels all treated actively (Juutilainen et al, 2005).
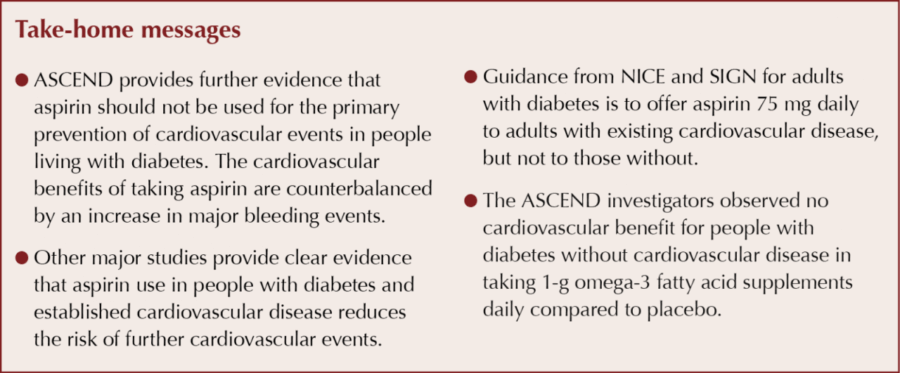
In people living with diabetes, aspirin use has clear benefits for secondary prevention of further events in those with established cardiovascular disease (CVD; Smith et al, 2011), with NICE guidance suggesting a variety of antiplatelet treatment strategies depending on which part of the vascular tree is affected (https://cks.nice.org.uk/antiplatelet-treatment).
There had been an orthodoxy that the presence of diabetes from middle life onwards was a coronary heart disease (CHD) “risk equivalent”. Investigators who analysed the concept of risk equivalence, by comparing the risk of subsequent CHD events among individuals with or without history of diabetes or CHD in a large real-world cohort over a period of 10 years (2002 to 2011), found that not all individuals with diabetes should be unconditionally assumed to be a risk equivalent of those with prior CHD (Rana et al, 2016). A recent paper has noted that individuals with type 2 diabetes who maintain five risk-factor variables within the target ranges appeared to have little or no excess risk of death, myocardial infarction or stroke, compared with the general population (Rawshani et al, 2018).
The ASCEND study
The ASCEND (A Study of Cardiovascular Events iN Diabetes) trial was initiated in 2005, when this CVD “risk equivalence” was accepted, and has examined the primary prevention of cardiovascular events with aspirin in people living with diabetes. It has been recently published and helps to clarify this use of aspirin further (ASCEND Study Collaborative Group, 2018a).
Aspirin
ASCEND examined whether aspirin reduced the risk of a first cardiovascular event in people living with diabetes. Between 2005 and 2011, 15480 people with diabetes, living in the UK, but who had no evident or manifest history of CVD, were randomly assigned to aspirin (100 mg daily) or matching placebo and followed for an average of 7.4 years. Investigators carefully matched the placebo group for length of diabetes, smoking status, treatment of hypertension and statin use. The 100-mg dose of aspirin is not the NICE or SIGN recommended dose but, in the light of a study suggesting a larger dose of aspirin in individuals >70 kg, is justifiable (Theken and Grosser, 2018), especially in the context of American diabetes guidance suggesting a higher dose (75–162 mg/day; American Diabetes Association [ADA], 2018).
Serious health outcomes that occurred to participants during follow up were recorded. These included first serious vascular events (the primary efficacy endpoint), which included non-fatal heart attacks, non-fatal strokes or death from a cardiovascular cause. During the recruitment phase, it was decided to add transient ischaemic attacks, which may have improved the statistical power of the study. Also included were first major bleeds (the primary safety endpoint), which included bleeding in the head or brain, from the gut or from elsewhere in the body that was serious enough to result in hospitalisation or be fatal.
Participants were then followed up for an average of 7.4 years. A first serious vascular event occurred in 685 (8.5%) participants allocated aspirin and 743 (9.6%) allocated placebo. Eleven of every 1000 participants avoided a serious vascular event during the trial as a result of allocation to aspirin, which represented a 12% proportional reduction in the risk of serious vascular events. However, a first major bleed occurred in 314 (4.1%) participants allocated aspirin and 245 (3.2%) allocated placebo, which meant that 9 of every 1000 participants suffered a first major bleed during the trial as a result of allocation to aspirin. This represented a 29% proportional increase in the risk of major bleeding. The numbers needed to treat (NNT) with aspirin was 91 over 7.4 years to avoid one serious vascular event.
The investigators concluded that the numbers of participants who avoided a serious vascular event were counterbalanced by the numbers who suffered a major bleed, feeling that it was not possible to identify a group of participants in the trial in whom the benefits of taking aspirin clearly outweighed the risks, with a number needed to harm (NNH) of 115. It is of note that approximately 25% of trial participants were receiving proton-pump inhibitors (PPIs).
Previous studies had suggested that aspirin might produce a reduction in cancers in the gut (especially in the bowel), with the effects increasing over time (Rothwell et al, 2018). During the ASCEND study, 897 (11.6%) cancers were noted in the aspirin group, and 887 (11.5%) in the control during the average 7.4 years of follow-up. No effect of aspirin on incident gastrointestinal cancer was observed, nor was there any apparent effect of aspirin on the overall risk of cancer. There is an intention to follow up the cancer effect.
Omega-3 fatty acids
As well as aspirin, omega-3 fatty acids (also known as n-3 fatty acids) have been associated with a reduced risk of CVD in observational studies. As part of the ASCEND study among individuals with diabetes without evidence of CVD, there was no significant difference in the risk of serious vascular events between those who were assigned to receive omega-3 fatty acid supplementation and those who were assigned to receive placebo (ASCEND Study Collaborative Group, 2018b). This finding in a controlled trial confirms observational data from a Cochrane collaboration which showed that increasing these omega-3 fatty acids has little or no effect on all-cause deaths and cardiovascular events (Abdelhamid et al, 2018).
Other aspirin studies
The 2009 Antithrombotic Trialists’ (ATT) Collaboration meta-analysis, involving 95000 participants in six primary prevention trials, showed that assignment to aspirin use led to a 12% lower risk of serious vascular events than control, and was published four years after the ASCEND study started (Antithrombotic Trialists’ [ATT] Collaboration, 2009). On average, however, the approximate 50% higher risk of bleeding with aspirin use than with control counterbalanced much of the benefit in these low-risk individuals. Only approximately 4% of participants in those trials had diabetes. Investigators concluded then that, considering the beneficial effect of aspirin in primary prevention, it is much less clear that there is an overall advantage in people who have not yet had a cardiovascular event.
In the recently published ARRIVE study, about 12000 people without diabetes were randomised to 100 mg of aspirin or placebo daily. The men who were enrolled were ≥55 years of age and had at least two cardiovascular risk factors; enrolled women were ≥60 years and had three of more cardiovascular risk factors. During an average follow-up of 5 years, aspirin conferred no cardiovascular benefit. The incidence of a composite endpoint that included myocardial infarction and stroke was about 4% in both groups. Gastrointestinal bleeding was slightly, but statistically significantly, more common with aspirin (Graziano et al, 2018).
The ASCEND study investigators acknowledged previous trials that specifically examined the use of aspirin to prevent ASCVD (ASCEND, 2018a). The JPAD (Japanese Primary Prevention of Atherosclerosis with Aspirin in Diabetes) study (Ogawa et al, 2008) involved participants with type 2 diabetes, while the JPPP (Japanese Primary Prevention Project) study (Ikeda et al, 2014) looked at a broader, elderly population. Both studies showed small, non-significant reductions in cardiovascular risk with aspirin.
The POPADAD (Prevention Of Progression of Arterial Disease And Diabetes) trial did not provide evidence to support the use of aspirin or antioxidants in primary prevention of cardiovascular events and mortality in the population with diabetes studied (Belch et al, 2008). In another trial involving people without diabetes but with a low ankle–brachial index (ABI), aspirin compared with placebo did not result in a significant reduction in vascular events (Fowkes et al, 2010).
It is also worth bearing in mind the potential for harm with aspirin. The recent ASCEND study shows a number needed to harm (NNH) of 112 over 7.4 years for a major gastrointestinal bleed. In another study of people with diabetes, the use of low-dose aspirin showed an increased risk of hospitalisation for ischemic stroke (Kim et al, 2015). A Swedish study revealed that daily low-dose aspirin treatment did not prevent cardiovascular events or death in people with type 2 diabetes and no previous CVD, and suggested an increase in the risk of CHD in females (Ekström et al, 2013). Aspirin-exacerbated respiratory disease in people living with asthma has also been reported (White and Stephenson, 2018).
Resistance to aspirin
Is there something about having diabetes that makes people not respond to aspirin? People living with diabetes may exhibit platelet hyper-reactivity, which renders them resistant to antithrombotic treatments, but clear evidence of true diabetes-related aspirin resistance is limited. In one study, investigators concluded that the prevalence of aspirin resistance is comparable in those with and those without diabetes, with hypercholesterolaemia the only independent predictor of aspirin resistance in participants with diabetes (Tasdemir et al, 2014). This is supported by another study which found that resistance to aspirin in people with diabetes is associated with lipid disorders and a history of current smoking (Łabuz-Roszak et al, 2014).
Guidance
In December 2015, NICE issued a clinical guideline update recommending that GPs did not offer antiplatelet therapy (aspirin or clopidogrel) for adults with type 2 diabetes without CVD (NICE, 2015). A similar recommendation was made in the SIGN (2017) type 2 diabetes guidance. It is of note, though, that in the 2018 ADA guidance, aspirin therapy (75–162 mg/day) may be considered as a primary prevention strategy in those with type 1 or type 2 diabetes who are at increased cardiovascular risk (ADA, 2018). This includes most men and women with diabetes aged ≥50 years who have at least one additional major risk factor (family history of premature atherosclerotic CVD, hypertension, dyslipidaemia, smoking or albuminuria) and are not at increased risk of bleeding.
Aspirin use in primary care diabetes
Does this new publication warrant any change in practice? As always, it is important to empower patients by having a discussion with them, informed by recent publications. As previously stated in this Journal, healthcare professionals will want to adhere to NICE or SIGN guidance and use aspirin 75 mg in secondary prevention of CVD in people living with diabetes, but not offer aspirin for primary prevention of cardiovascular events in people living with diabetes (Kenny, 2016).




Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025