One of the major causes of type 2 diabetes is obesity (Ndisang et al, 2017). The American Diabetes Association (2021) recommends maintaining a healthy diet and regular exercise to reduce body weight and, therefore, reduce the risk of developing type 2 diabetes and complications associated with the condition. The Global Burden of Disease 2015 Obesity Collaborators (2017) have investigated the impact of obesity and found that 604 million adults are obese worldwide.
A complication associated with obesity is considerable joint compression and inflammation, leading to musculoskeletal disorders causing joint pain and decreased movement within lower limb joints and the lower back (Onyemaechi et al, 2016). In these circumstances, performing exercise to reduce weight can exacerbate joint pain, impacting on quality of life and physical function (Shultz and Ambrose, 2017). To overcome these difficulties, water-based exercise interventions have been proposed, and a meta-analysis by Barker et al (2014) concluded that low-weight-bearing exercise such as water-based exercise reduced pain and increased range of joint motion, improving physical function and quality of life.
Williams et al (2016) performed a systematic review confirming the link between type 2 diabetes and musculoskeletal disorders. Within that review, the authors highlighted that people with type 2 diabetes are advised to carry out physical exercises regularly but that their pain and physical limitations are not being taken into consideration, impacting on their treatment and leading to further progression of both their diabetes and musculoskeletal disorders.
Water-based environments provide a safe and protective means to exercise due to water’s buoyancy, and thus they reduce the risk of joint injury. This allows individuals who are overweight or obese with musculoskeletal complications to exercise at a high intensity that can generate weight loss and improve fitness levels which may not be achievable on land due to heavy joint loading (Becker, 2009).
Systematic reviews have assessed how water-based exercise programmes affect glycaemic control, vascular function and quality of life in people living with type 2 diabetes (Rees et al, 2017). However, no systematic review has yet been completed on the impact of water-based exercise on body weight in people with type 2 diabetes. Thus, this systematic review aims to address a gap in the research and our knowledge.
Methods
Aim
The aim of this systematic review was to examine the effect of water-based exercise programmes on body weight in people with type 2 diabetes.
Inclusion criteria
Studies had to include participants over the age of 18 years with a diagnoses of type 2 diabetes. The intervention must have included a structured, water-based exercise programme with reported pre- and post-intervention body weight measurements. Only English-language articles were considered. Studies that did not report the primary or secondary outcomes were excluded.
Search strategy
Using the search strategy guidelines of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al, 2022a), a systematic search was performed to ensure all relevant literature was included. Through use of the EBSCO host search engine, the MEDLINE, CINAHL Plus with Full Text, Health Business Elite, Information Science & Technology Abstracts and APA PsycInfo databases were searched, in addition to the individual PubMed, Google Scholar and Cochrane Library databases.
Key search terms as below were used in each of the databases, along with the Boolean operators “OR” and “AND”:
- Diabetes mellitus type 2.
- Diabetes.
- Water-based exercise.
- Aquatic based exercise.
- Weight.
- Body mass.
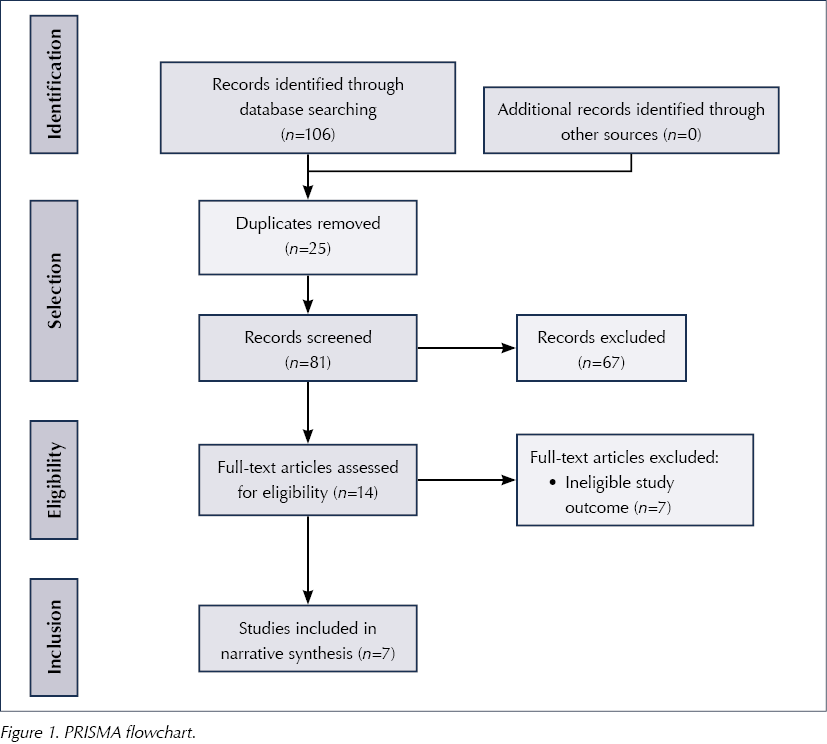
Figure 1 summarises the overall process of the comprehensive search that was undertaken.
Data extraction and quality appraisal
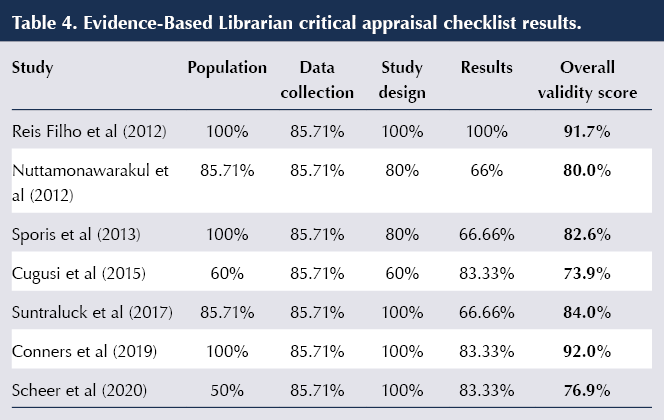
Accurate, relevant and standardised data were collated and presented using a bespoke data extraction table. The Evidence-Based Librarian critical appraisal checklist tool (Glynn, 2006) was used to assess the quality and validity of each selected study.
Data analysis
It was initially attempted to run a meta-analysis using RevMan; however, this was not possible as the statistical heterogeneity of the combined studies, tested using the I² value, was 95%, indicating considerable heterogeneity. Therefore, a narrative analysis methodology was used.
Results
Description of included studies
Of the seven studies that met the inclusion criteria, two were based in Thailand and the other five were based in Italy, USA, Brazil, Croatia and Australia, respectively. The timeframe of the studies ranged from 2012 to 2020, and they were set predominantly in a community setting, with one study conducted in a hospital setting. One study did not state the setting.
Study participants
All seven studies involved adults over the age of 18 years with a medical diagnosis of type 2 diabetes. No participants were on insulin and no change was made to any participant’s medication or treatment during the course of any of the studies.
Four studies focused on adults over the age of 60 years (Reis Filho et al, 2012; Nuttamonwarakul et al, 2012; Suntraluck et al, 2017; Scheer et al, 2020). Cugusi et al (2015) enrolled participants aged 40–65 years, while the participants in Conners et al (2019) had a mean age of 58 years. In Sporis et al (2013), participants were aged between 39 and 73 years, with a mean age of 56 years. The study by Cugusi et al (2015) had male participants only; all other studies involved male and female participants. The smallest sample size was 18 (Cugusi et al, 2015) and the largest was 40 (Nuttamonwarakul et al, 2012).
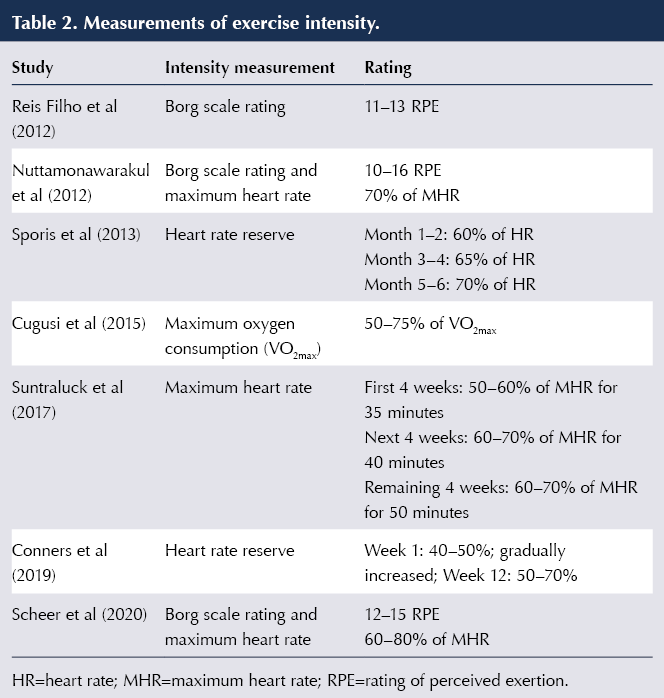
Description of water-based exercises
Table 1 details the different types of water-based exercise and the elements that were involved in each study. Intensity levels of the exercises were measured differently throughout the studies, as seen in Table 2. The Borg scale: Rating of Perceived Exertion (Borg, 1982) was used in three studies to measure exercise intensity (Reis Filho et al, 2012; Nuttamonwarakul et al, 2012; Scheer et al, 2020). The Borg scale measures an individual’s perception of the difficulty of an activity, with six being no exertion, and 20 meaning maximum exertion (Ritchie, 2012). Exercise intensity levels as a percentage of maximum heart rate (MHR) was recorded within three studies (Nuttamonwarakul et al, 2012; Suntraluck et al, 2017; Scheer et al, 2020). MRH is used in physical activity studies as an indicator of a participant’s level of effort (Boer, 2017). It is determined and formulated by subtracting a participant’s age from 220; for example, 220 (years) – 60 = 160 bpm MHR. Two studies measured intensity by monitoring heart rate reserve (Sporis et al, 2013; Conners et al, 2019). Heart rate reserve is found by subtracting a resting heart rate from a maximum heart rate. One study measured exercise intensity by monitoring maximum oxygen consumption (VO2max; Cugusi et al, 2015). This measurement is widely used to measure cardiorespiratory fitness (Chavarrias et al, 2020) and measures the maximum amount of oxygen consumed during exercise.

Data collection methods
The participants’ weight was measured at the beginning of all seven studies. Different brands of scales were used to take measurements throughout the studies. One study obtained measurements on the first, sixth and final twelfth week of the study (Reis Filho et al, 2012). Sporis et al (2013) carried out measurements one week before the trial, at 3 months and at 6 months. All other studies obtained measurements on the first and last week of the trial.
Outcomes measured
The seven studies measured the effect of water-based exercise on a range of outcomes, including body weight, HbA1c levels, blood pressure measurements and maximum oxygen uptake. The data and information extracted from each study are represented in Table 3.
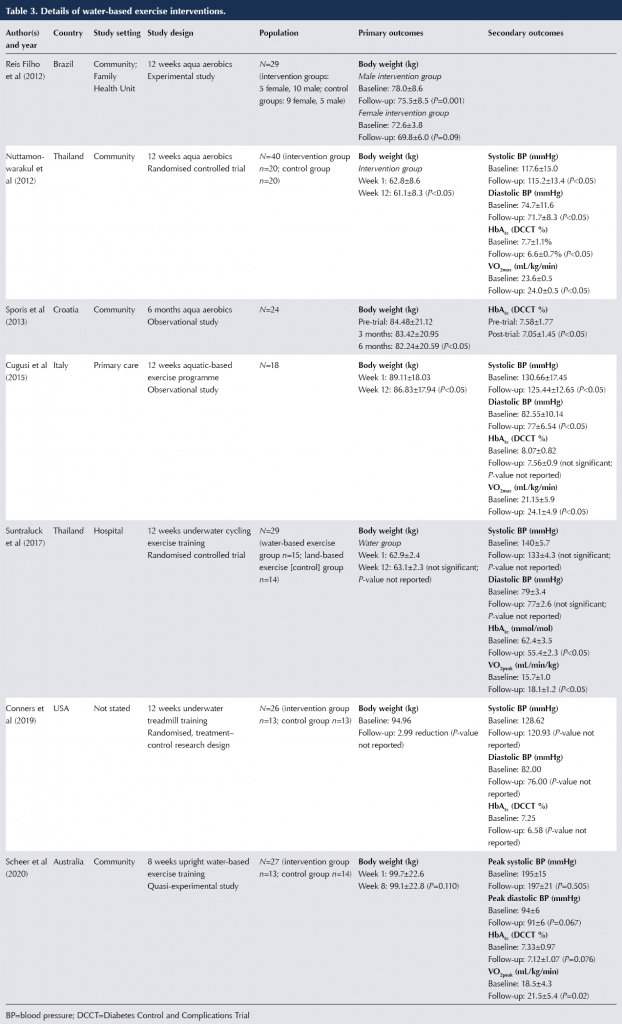
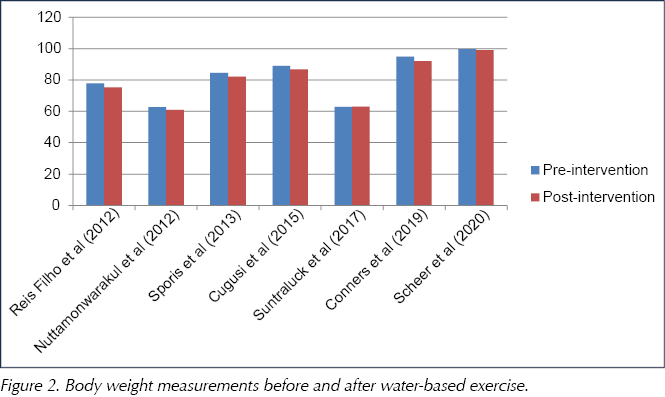
Primary outcome results: Body weight
The form of water-based exercise and the measurement of intervention intensity varied throughout the seven studies. Because of the heterogeneous nature of the studies, a narrative analysis of the primary outcomes was carried out. In Reis Filho et al (2012), 12 weeks of water aerobics resulted in a significant body weight reduction within males (2.5 kg reduction; P=0.01), but not females (2.8 kg reduction; P=0.09).
Nuttamonwarakul et al (2012) reported a significant reduction (1.7 kg reduction; P<0.05) in the participants’ body weight after 12 weeks of aqua aerobic exercise. Sporis et al (2013) reported a significant reduction of 2.64% after six months of aquatic aerobics. Cugusi et al (2015) reported a significant reduction (2.3 kg; P<0.05) in body weight after 12 weeks of water circuit training. Conners et al (2019) reported a mean body weight reduction of 2.99 kg (no P-value reported) after 12 weeks of underwater treadmill training sessions.
However, Scheer et al (2020) found no significant reduction (0.6 kg; P=0.110) in body weight measurements after 8 weeks of water circuit training, and Suntraluck et al (2012) observed an increase in body weight after 12 weeks of a water cycling training programme (0.2 kg; no P-value reported).
Table 3 presents the mean body weight measurements reported in the studies, and Figure 2 is a visual representation of the primary outcome findings.
Secondary outcome results
Blood pressure
Four of the seven studies measured the effect of water-based exercise on resting systolic and diastolic blood pressure (BP) readings (see Table 3). Nuttamonwarakul et al (2012) reported a significant reduction (P<0.05) in resting blood pressure, both systolic (2.4 mmHg) and diastolic (3.0 mmHg), amongst the participants after 12 weeks of aqua aerobics. Cugusi et al (2015) observed significant (P<0.05) reductions in systolic (5.22 mmHg) and diastolic BP (5.55 mmHg) after 12 week of aqua aerobics. Suntraluck et al (2017) reported a reduction in BP after 12 weeks of underwater cycling; however, this was not a significant difference and no P-value was reported. Resting systolic and diastolic BP readings were also reported by Conners et al (2019). Systolic BP dropped by 7.69 mmHg and diastolic BP by 6.00 mmHg after 6 months of underwater treadmill training. It was not indicated whether this was a significant reduction.
HbA1c levels
Six of the seven studies reported the effect of water-based exercise on HbA1c levels (see Table 3). After 12 weeks of aquatic aerobics, Nuttamonwarakul et al (2012) reported a significant reduction in HbA1c (1.1%; P<0.05). Sporis et al (2013) also reported a significant reduction (0.53%; P<0.05) after 6 months of aqua aerobics. Suntraluck et al (2017) reported a significant reduction (7 mmol/mol; P<0.05) following 12 weeks of water cycling. Conners et al (2019) reported a reduction of 0.67% following a 12-week underwater treadmill exercise programme; however, a P-value was not reported. Both Cugusi et al (2015) and Scheer et al (2020) reported no significant change to HbA1c levels post-intervention.
Maximum oxygen uptake (VO2max)
The effects of water-based exercise on maximum oxygen uptake (VO2max) was measured in four of the seven studies (see Table 3). VO2max is widely used to measure cardiorespiratory fitness, and is the rate at which oxygen is used during intense exercise (Grant et al, 1995. Nuttamonwarakul et al (2012) reported a significant increase in participants’ VO2max levels (0.4 mL/kg/min; P<0.05) after 12 weeks of aqua aerobics. A significant improvement (2.95 mL/kg/min; P<0.05) was also reported by Cugusi et al (2015) after 12 weeks of aquatic exercise. Scheer et al (2020) reported a significant improvement (3.0 mL/kg/min; P=0.02) following eight weeks of water circuit training. Suntraluck et al (2017) reported a significant improvement (2.4 mL/kg/min; P<0.05) following 12 weeks of underwater cycling exercise training.
Quality appraisal
The Evidence-Based Librarian critical appraisal checklist was completed on each of the seven studies. Table 4 gives an overview of the validity score of each study. Six studies had a validity score over 75%. One study, by Cugusi et al (2015), scored 73.91%. It was unclear in this study whether the researcher was also involved in delivering a service to the target population. Three studies reported small sample sizes (Cugusi et al, 2015; Suntraluck et al, 2017; Scheer et al, 2020). Confounding variables were only identified in one study (Reis Filho et al, 2012) and were not reported in the other six studies. The study by Cugusi et al (2015) only involved male participants and so this created a risk of population bias. In addition, the study did not report approval from an ethics committee; however, the researchers did report obtaining informed consent from participants. Lastly, three studies did not make any recommendations on further research (Nuttamonwarakul et al, 2012; Sporis et al, 2013; Suntraluck et al, 2017).
Discussion
The primary aim of this systematic review was to review the evidence on the effect of water-based exercise on body weight in people with type 2 diabetes. The secondary outcomes that were focused on were blood pressure, HbA1c levels and maximum oxygen uptake.
In relation to the primary outcome, it was found that water-based exercise was effective in four of the seven studies in reducing body weight in participants with type 2 diabetes. Six of the seven studies reported the BMI of the participants, with all being either overweight or obese. The fact that all studies involved participants who were either overweight or obese adds strength to this systematic review as it is capturing the demographic profile of those who are most at risk of developing both cardiovascular and musculoskeletal complications associated with obesity and type 2 diabetes. In a one-year observational study, Wing et al (2011) recommended a weight loss of 5–10% to reduce the risk of cardiovascular complications; however, they stated that as little as 2–5% weight loss can have a positive effect on cardiovascular risk factors by stabilising glycaemic control. Although a significant difference was not found in three of the studies, it can be considered that even a minimum amount of weight loss can reduce the risk of complications in an individual with type 2 diabetes.
Only two of five studies reported a significant reduction in BP following water-based exercise. Lowering BP levels in people with type 2 diabetes reduces cardiovascular risk, including stroke, and retinopathy (Emdin et al, 2015). However, it must be noted that the literature reports inconsistent BP targets for individuals with type 2 diabetes, making it difficult to set an optimum goal (Grossman and Grossman, 2017; Shen et al, 2019).
The effect of water-based exercise on maximum oxygen uptake showed a significant overall positive result, with four studies reporting a significant improvement in cardiopulmonary fitness in the participants. There is a link associated between VO2max and insulin sensitivity; if VO2max is improved then it can have a positive effect on insulin sensitivity, reducing insulin resistance and therefore lowering blood glucose levels (Leite et al, 2009).
Water-based exercise was reported to significantly decrease HbA1c levels in three studies. Reducing HbA1c levels by 11 mmol/mol (1.0%) is associated with a 14% reduction in myocardial infarction risk and a 21% reduction in diabetes-related mortality (Najafipour et al, 2017). Any improvement in BP, VO2max and HbA1c levels may have substantial effects on an individual basis.
Water-based exercise performed in warm water environments can increase leg muscle strength and endurance, reduce muscle pain and spasms, and is perceived to be more enjoyable, improving quality of life for people with musculoskeletal disorders (Foley et al, 2003; Cadmus et al, 2010; Kargarfard et al, 2012; Rees et al, 2017). Silva et al (2008) highlighted that water-based exercise was effective in reducing pain in people with osteoarthritis compared to land-based exercise.
Nam et al (2011) have reported pain to be one of the barriers in diabetes management. Due to these findings and limited studies in this topic, research into water-based exercise and pain management in people with type 2 diabetes could be considered for future research and could have beneficial findings on how to treat individuals with type 2 diabetes who are obese and have musculoskeletal pain.
Finally, as diabetes is a long-standing, progressive disorder and the studies involved were conducted over a short period of time, ranging from 8 weeks to 6 months, it is recommended that more research be carried out involving long-term water-based exercise programmes and their long-term effects on people living with type 2 diabetes.
Study strength and limitations
The sample sizes were relatively small in all studies. In three studies the authors recognised this as a limitation. Dropout rates were discussed by Reis Filho et al (2012), with a 17.5% dropout rate; Suntraluck et al (2017), with a 19.5% dropout rate; and Scheer et al (2020), with 30% of participants not completing the 8-week exercise programme. Both the small sample sizes and high dropout rates could have had an impact on the power of the studies’ results and increase the risk of bias due to missing outcome data (Higgins et al, 2022b).
Three studies declared a limitation in that they had no control group to minimise the effect of variables. However, Suntraluck et al (2017) argued that it was deemed unethical to have a control group providing no intervention to the participants, so the authors compared water-based to land-based exercise.
To enhance the strength of this systematic review, it was noted that all seven studies performed water-based exercises that were structured and according to a programme. Intensity levels were reported and monitored closely in each study. These programmes can be easily replicated for use in future treatment interventions; however, strength also lies in the precision and accuracy of the intervention execution reported by each study, which ensures uniform data collection for each session. Contributing to the strength of this review, six of the seven studies scored over 75% when critically appraised.
Conclusion
The primary aim of this systematic review was to investigate how water-based exercise affects body weight in people with type 2 diabetes. Overall findings suggested that water-based exercise significantly decreases body weight. Secondary outcome results showed that two articles reported a significant reduction in BP, three reported a reduction in HbA1c levels and four reported improved VO2max levels. However, due to small sample sizes and high dropout rates, the overall results should be considered with caution. The global population of people living with type 2 diabetes is growing rapidly and, therefore, the need to research different treatments and interventions is much needed to ensure there are different and effective interventions available to fit all medical needs.






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024