What and why
● The onset of both type 2 diabetes and dementia are strongly age-dependent. The global epidemic of type 2 diabetes and an increase in life expectancy means that the co-morbidity of diabetes and dementia is becoming increasingly common.
● See At a glance factsheet: Diabetes and dementia for more information on the associations and implications of co-morbid diabetes and dementia.1
● People with dementia are likely to find managing their diabetes very challenging and, thus, may be at greater risk of diabetes complications.
● An individualised approach to management of diabetes in a person with dementia that is supportive of family and carers is absolutely essential.
● The aim of management is to improve the person’s quality of life. For this, a holistic approach is required.2
Identifying dementia
● A variety of tests of cognitive impairment can be used to help identify dementia.3
- The Mini-Mental State Examination (MMSE) is commonly used and has a high sensitivity and specificity for detecting dementia.
- Other tests that perform well include the Mini-Cog test and Addenbrooke’s Cognitive Examination–Revised (ACE-R).
Screening for dementia in people with diabetes
● Given the increased risk of dementia in people with diabetes, some guidelines have suggested screening for dementia in people with diabetes over the age of 65 years.4
● Consider screening for individuals who are having trouble managing their medications, have lost control of their blood pressure, lipid levels or glycaemia, or have been missing appointments.5
Overall management strategy
● An individualised approach to managing diabetes according to the needs and circumstances of the person concerned is required.6
● People with dementia should have equivalent access to diagnosis, treatment and care services for diabetes as people without dementia.7
● The individual with diabetes and dementia is likely to require a multidisciplinary approach that could involve specialised nurses, dietitians, geriatricians, neurologists, psychiatrists, endocrinologists and GPs.
● Those people with dementia who have diabetes will need regular follow-up for their diabetes, preferably with a healthcare professional who is aware of their social situation.2
● The aim of diabetes management should be to optimise quality of life.
Glycaemic targets
● A holistic assessment focusing on functional status rather than age alone is important in deciding the appropriate level of glycaemic control.8
● Frailty, other comorbidities (e.g. cardiovascular and renal disease), polypharmacy, social setting and reduced life expectancy can all impact on the level of glycaemic control suitable for an individual.9
● A key priority in the individual with dementia is avoidance of hypoglycaemia caused by diabetes medications. This may demand less intensive glycaemic control.
- An HbA1c target of 59–69 mmol/mol (7.5–8.5%) may be appropriate, especially if diabetes treatments that induce hypoglycaemia are being used.
● See How to manage diabetes in later life for a summary of advice.10
Lifestyle
● A healthy diet and exercise should be encouraged in people with dementia who have diabetes, both to improve glycaemic control and to reduce cardiovascular risk.6,11
● A healthy lifestyle and avoidance of overweight/obesity should be advised in those with dementia as a preventative measure against the onset of type 2 diabetes.
Role of carers
● As cognitive impairment and frailty progress, there will be increasing dependence on family and carers to supervise diet, medication administration and glucose monitoring.
● It is of paramount importance to liaise with carers and to provide information and support for them.12
● Carers are frequently female family members who are not in employment.
● Carers need education in diabetes care to empower them to carry out their role and also provision of information on benefit entitlements.13
Diabetes medications in the person with dementia
● In general, the guidelines for type 1 and type 2 diabetes should be followed for people with diabetes and dementia.6,11
● However, there is potential for overtreatment with diabetes medications, and the benefits and harms of each treatment need to be carefully assessed. The benefits from tight glycaemic control can take years to accrue and, thus, may not apply to an individual with limited life expectancy.
● Avoidance of hypoglycaemia from antidiabetes medication is of paramount importance in elderly individuals with dementia; not only are they at increased risk of hypoglycaemia, but also the consequences of this may be more profound. Furthermore, hypoglycaemia itself can accelerate cognitive decline.
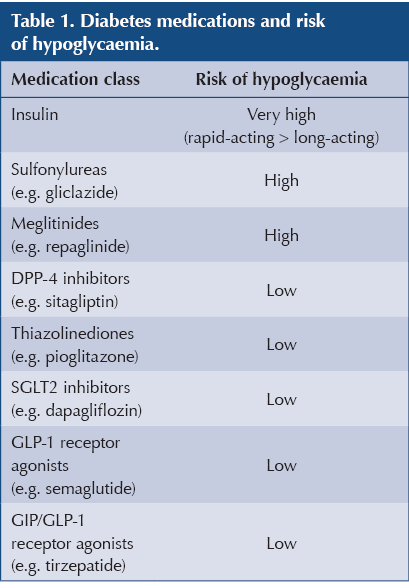
- Medications that induce hypoglycaemia (Table 1) should be used cautiously and, if possible, are better avoided.
- Insulin presents particular problems for the person with dementia, due to its mode of delivery, requirement of blood glucose monitoring and propensity to cause hypoglycaemia.
● Polypharmacy is a concern in the elderly person with dementia, with attendant risks of drug interactions and poor adherence. Where possible, treatment regimens should be simplified and treatment burden reduced.
Are there any cognitive benefits from diabetes medications?
● A Cochrane review in 2017 found no evidence that any specific treatment for type 2 diabetes prevented or delayed cognitive impairment.14
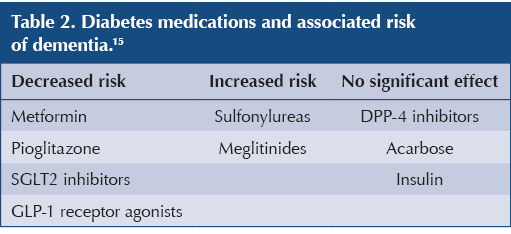
● However, a more recent systematic umbrella review and meta-analysis did find certain treatments for type 2 diabetes were associated with different risks of dementia (Table 2).15
- Several studies have specifically suggested that SGLT2 inhibitors have a beneficial effect on cognitive function, particularly in those with mild cognitive impairment or dementia, and reduce the risk of dementia compared with non-users (hazard ratio 0.68; 95% confidence interval 0.50–0.92).16
- A recent observational study of people with type 2 diabetes aged 49–69 years found that, compared with DPP-4 inhibitors, SGLT2 inhibitors were associated with a 35% relative risk reduction in dementia over a mean of 2 years.17 The risk of both Alzheimer’s disease and vascular dementia were significantly reduced.
● Causality and underlying mechanisms still need to be shown.
Glucose monitoring
● Self-monitoring of blood glucose (SMBG) is useful for those people with dementia who are taking oral medications that induce hypoglycaemia or insulin.
- Undertaking this, interpreting the results and taking appropriate action may require support from family members or carers.6
● Continuous glucose monitoring (CGM) avoids the practical difficulties of SMBG but is still likely to require a supervising person.
- CGM can be the method of choice for monitoring blood glucose in the person with dementia using insulin.
● All adults with type 1 diabetes should be offered a choice of real-time CGM or intermittently scanned CGM (isCGM). It is important that people using CGM retain SMBG as a back-up.11
● CGM offers improved glycaemic control with reduced hypoglycaemic burden compared with SMBG. Alerts can be set for both hypoglycaemia and hyperglycaemia.18
● isCGM is also an option for people with type 2 diabetes and dementia on multiple daily insulin injections if:6
- They suffer from recurrent or severe hypoglycaemia.
- They have impaired hypoglycaemia awareness.
- They have a condition that prevents them using SMBG but in which isCGM is feasible.
- They are using SMBG eight times a day or more.
Useful resources
● How to manage diabetes in later life
● How to prevent, identify and manage hypoglycaemia in adults with diabetes
● At a glance factsheet: Deprescribing in type 2 diabetes
● Diabetes Distilled: The 4S Pathway – realigning management for older people with diabetes





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025