Hypoglycaemia
Hypoglycaemia occurs when the blood glucose level falls below 3.9 mmol/L. A level below 3.0 mmol/L is defined as clinically important hypoglycaemia.1
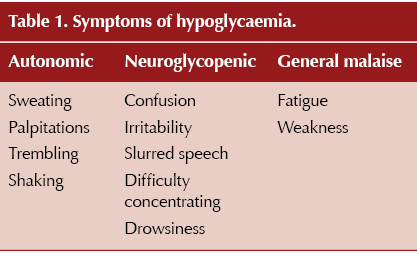
Hypoglycaemia symptoms can be categorised into three different types (Table 1). Autonomic symptoms should occur first to warn and prompt appropriate action to restore normoglycaemia. However, if autonomic symptoms are absent or not recognised, neuroglycopenic symptoms develop due to the brain being deprived of glucose, leading to cognitive impairment. In addition, some older people experience more generalised symptoms of hypoglycaemia.
For more information on hypoglycaemia, see How to prevent, identify and manage hypoglycaemia in adults with diabetes.
What is impaired hypoglycaemia awareness?
Impaired hypoglycaemia awareness (IHA) is defined as reduced ability to recognise or perceive the onset of hypoglycaemia, meaning that hypoglycaemia symptoms are not triggered until glucose levels are very low, often after cognitive function is impaired.1 IAH affects 20–25% of people living with type 1 diabetes and 10% of people with type 2 diabetes treated with insulin therapy.2,3
Owing to the reduced ability to recognise hypoglycaemia and take corrective action, IHA is a major risk factor for severe hypoglycaemia. This occurs when blood glucose falls so low that the person is unable to self-treat the hypoglycaemia and/or experiences loss of consciousness or seizure, requiring third-party intervention.
Risk factors for IHA
The mechanisms that lead to IHA are not fully understood; however, repeated exposure to hypoglycaemia over time can lead to a reduced counter-regulatory response to falling glucose levels. IHA is more common in people with a longer duration of diabetes and can also affect older adults.
In older people, autonomic symptoms of hypoglycaemia occur at a lower blood glucose level and neuroglycopenic symptoms occur at a higher level than in younger individuals. Therefore, autonomic symptoms and neuroglycopenic symptoms can happen almost simultaneously in older individuals. This means there is often little warning that blood glucose is falling, due to the lack of autonomic warning signs at the appropriate level.4
How to assess hypoglycaemia awareness
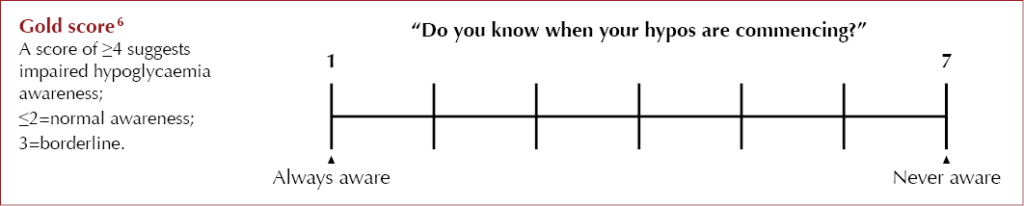
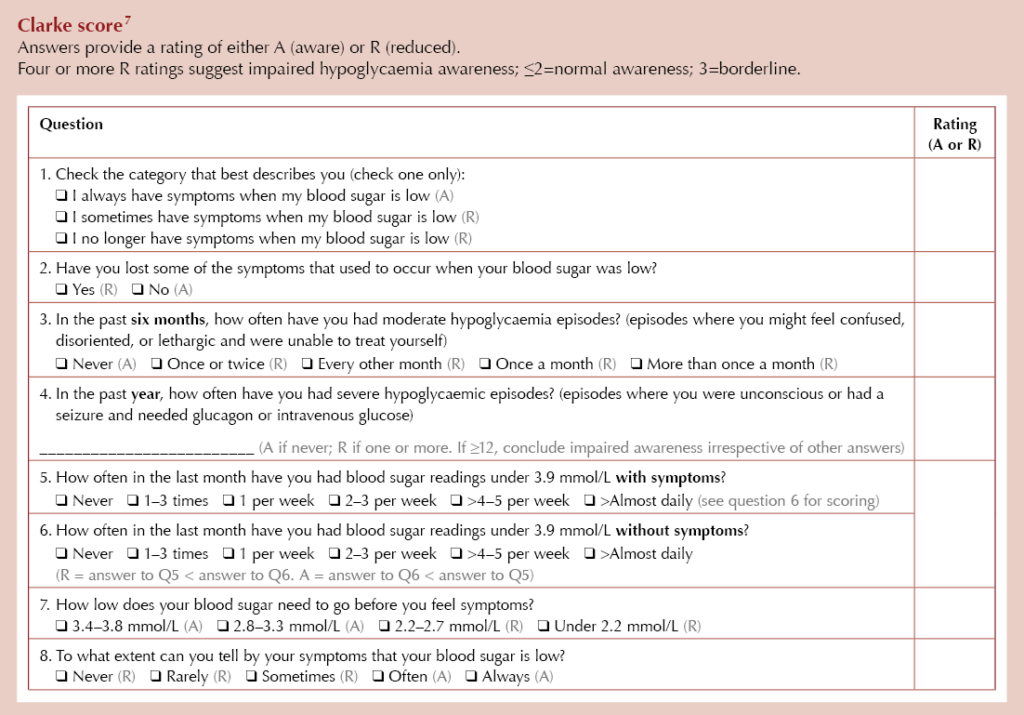
There is currently no single gold-standard test to assess IHA; however, the Gold score and Clarke score are two validated tools which NICE currently recommends as methods to assess awareness of hypoglycaemia in people with type 1 diabetes.5
Although these tools have not been validated in people living with type 2 diabetes, they do offer a clinically meaningful way to assess hypoglycaemia awareness. They can be particularly helpful in identifying people with type 2 diabetes on multiple daily injections with IHA who may benefit from continuous glucose monitoring (CGM) technology.
Psychosocial implications of IHA
High levels of fear or concern about hypoglycaemia can lead to anxiety, emotional stress and insecurity. It can also lead the person to maintain higher glucose levels to prevent hypoglycaemia, resulting in suboptimal glucose management and increased risk of diabetes-related complications.
Conversely, some people with IAH show low levels of fear or concern about the consequences of their hypoglycaemia, and this can cause barriers to hypoglycaemia avoidance, resulting in continued subsequent hypoglycaemia.
The impact of IHA can affect a person’s day-to-day quality of life, including their sleep quality. It can also impact the lives of their parents, caregivers, and partners, due to increased reliance on others.
IHA can also have occupational implications, particularly for those who rely on driving for their occupation or who drive buses, lorries, private hire or emergency vehicles. In some cases, loss of employment my occur due to disability.1
Driving
The DVLA defines IHA as “an inability to detect the onset of hypoglycaemia because of total absence of warning symptoms”.8 People with IHA must stop driving and inform the DVLA.
Group 1 licence (Cars and Motorbikes):
Driving may resume after a clinical report by a GP or consultant diabetes specialist confirms that adequate hypoglycaemia awareness has been regained.
Group 2 licence (Bus and Lorry):
The licence will be refused or revoked.
The DVLA also states that CGM alarms are not accepted as a substitute for adequate symptomatic or physiological awareness of hypoglycaemia. Should a driver become reliant on these alarms to alert them that they are hypoglycaemic, they must stop driving and notify the DVLA.
For full DVLA regulations, see here.
Management of IHA
Education
Structured education in flexible insulin dose adjustment (e.g. DAFNE) is recommended to improve hypoglycaemia awareness and reduce risk of severe hypoglycaemia. Bolus calculators are also available to help precisely calculate the insulin dose required in any given situation, considering the current glucose level, carbohydrate eaten and current active insulin.
Continuous glucose monitoring
Continuous glucose monitoring (CGM) is recommended for all people living with type 1 diabetes by NICE NG17.5 This technology has proven benefit in people with IAH and severe hypoglycaemia. Some CGM devices have predictive low alarms, helping to mitigate hypoglycaemia before it occurs. Such systems may offer greater benefit in hypoglycaemia avoidance in people with IHA. Devices with predictive alarms are not currently available to prescribe in primary care and are initiated within specialist diabetes teams.
NICE NG28 recommends offering intermittently scanned CGM or real-time CGM (if available at the same or lower cost) for people living with type 2 diabetes on multiple daily insulin injections who have IAH or recurrent severe hypoglycaemia.9 There are several systems available to prescribe in primary care. For more information on the different systems available, see the DSN Forum UK CGM comparison chart.
Using trend arrows to aid hypoglycaemia avoidance
CGM can give greater insight to aid hypoglycaemia prevention by using the trend arrows. Generally, if the glucose level is less than 6 mmol/L and there is a downward trend arrow, the person should consider consuming 5–10 g of fast-acting carbohydrate (1–2 jelly babies) and re-check their glucose in 10–15 minutes.
Trend arrows and their meanings will vary based on the CGM system used. For more detailed advice, see the Diabetes Technology Network UK video Using CGM to reduce hypoglycaemia.
Insulin regimens
Types of insulin that reduce the risk of hypoglycaemia are preferable. Optimal insulin therapy when part of a multi-dose regimen should usually involve the use of rapid-acting insulin analogues and basal or ultra-long-acting basal analogues.10
Insulin pumps
Insulin pumps and hybrid closed-loop therapy have also been shown to reduce severe hypoglycaemia in people with type 1 diabetes. The assessment and management of such technology is undertaken by specialist diabetes teams. NICE NG17 suggests that, if impaired awareness of hypoglycaemia or recurrent severe hypoglycaemia is present, CGM with alarms or sensor-augmented pump therapy may be more suitable than standalone pump and CGM devices.5
For more information on the different systems available, see the DSN Forum UK HCL comparison chart.
A NICE Technology Appraisal on hybrid closed-loop systems is expected to be published imminently.
Further resources
How to prevent, identify and manage hypoglycaemia in adults with diabetes
Diabetes & Primary Care 24: 69–70
Click here to access
How to initiate and support continuous glucose monitoring
Diabetes & Primary Care 25: 117–9
Click here to access






Jane Diggle examines the draft update to the NICE NG28 clinical guideline, plus new advice regarding the discontinuation of Levemir.
10 Sep 2025