Not so sweet? Low-calorie sweeteners, obesity and metabolic health
Amy Rothberg (Chair), Michelle Pang, Richard Mattes
● Sugar intake is high in the US (around 400 kcal/day for men and 300 kcal/day for women) and leads to chronic diseases. Reduction is recommended, and low-calorie sweeteners (LCS) help achieve this.
● LCS include aspartame, acesulfame-K, saccharin, stevia glycoside and sucralose. Each have different structures and pharmacokinetics, and thus different effects in the body.
● Global LCS consumption is increasing – around 15% of children and 35% of adults regularly consume LCS in drinks and food.
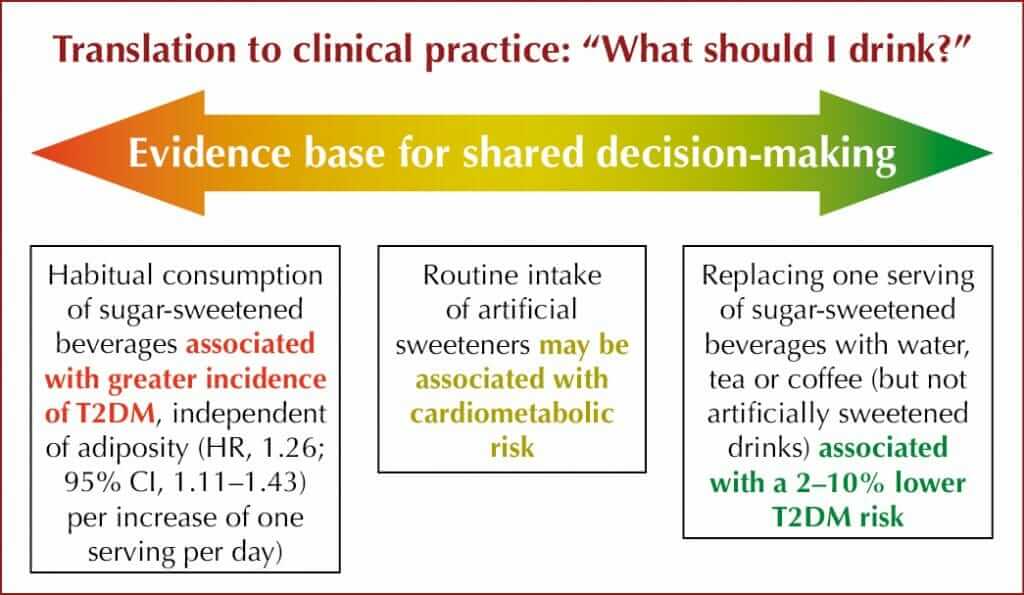
● Controversies include possible changes in taste preferences, increased adipogenesis and weight gain, increased insulin, effects on the gut microbiome, faster glucose absorption, inflammation, glucose intolerance and unhealthy diet patterns leading to potential cardiometabolic disease.
● LCS have been extensively reviewed and safety has been confirmed by international food standards bodies.
● Compared with sugar-sweetened beverages or water, LCS decreased weight in both adults and children (Rogers et al, 2016) but mechanisms may be different for each LCS. When individual sweeteners were examined, a meta-analysis of aspartame and stevia and randomised controlled trials of sucralose and saccharin showed no weight reduction.
● No effects on human glucose absorption; the majority of studies show no effect on insulin levels and no conclusive effects on type 2 diabetes risk in humans.
● LCS are not associated with any differences in hunger, fullness or desire to eat compared with water (Fantino et al, 2018).
● There was no dietary compensation when stevia or aspartame versus sucrose were used as pre-load; daily calorie intake was lower with LCS than sucrose (Anton et al, 2010).
● Gut microbiome response may be individual. LCS may help protect from the effects of lipopolysaccharides and inflammation.
● Long-term clinical studies are needed to confirm effects of individual LCS on body weight and safety. The European SWEET project is exploring the impact of LCS on health, obesity, safety and sustainability, looking at barriers and facilitators for use, and risks and benefits when used to replace sugar.
For more information, see the recent systematic review and meta-analysis by McGlynn et al (2022).
Just how plant-based should people with diabetes go?
Holly Willis (Chair), Lauren Plunkett, Qi Sun, Christopher Gardner, Kim Williams
● Plant-based diets (vegan or vegetarian) or predominantly plant-based diets (flexitarian, pescatarian) are associated with lower risk of developing type 2 diabetes, delay development of the condition in high-risk groups and are beneficial for management in people with established type 2 diabetes.
● Plant-based diets can be healthy or unhealthy, depending on amounts of processed, ultra-processed or whole foods included.
● UK and US nutrition guidelines for prevention and management of type 2 diabetes recommend mainly or wholly plant-based, whole-food eating patterns, including Mediterranean patterns and the DASH (Dietary Approaches to Stop Hypertension) diet (Dyson et al, 2018; Evert et al, 2019).
● The ACC/AHA guideline on the primary prevention of cardiovascular disease (Arnett et al, 2019) recommends a diet that emphasises intake of vegetables, fruit, nuts, whole grains and fish, and reminds clinicians that, for primary prevention of ASCVD, “it is reasonable to minimize the intake of processed meats, refined carbohydrates and sweetened beverages.”
● For adults with type 2 diabetes, the ACC/AHA guideline recommends a tailored nutrition plan focusing on a heart-healthy dietary pattern to improve glycaemic control, achieve weight loss if needed and improve other ASCVD factors.
● Healthy plant-based eating patterns are low-glycaemic-index and high-fibre, contain multiple beneficial phytochemicals, including polyphenols, and have beneficial effects on the gut microbiome.
● Plant-based eating patterns increase microbiome diversity and increase numbers of bacteria that produce short-chain fatty acids, which have beneficial effects on weight and metabolism (Chen et al, 2021; Sharma et al, 2022).
● Plant-based diets contain as much, if not more, quality protein than omnivorous diets. All plant foods contain all amino acids, although some may be in small amounts. Eating a mixed, plant-based diet ensures optimal amounts of all amino acids, and no food combining is needed.
● Most people are eating too much protein, which cannot be stored in the body and so excess is converted to carbohydrates and fat. Most people would benefit from reducing protein intake by 25% and considering swapping 25% of protein intake from animal- to plant-based.
● Plant-based diets (vegan or vegetarian) or predominantly plant-based diets (flexitarian, pescatarian) are associated with lower risk of developing type 2 diabetes, delay development of the condition in high-risk groups and are beneficial for management in people with established type 2 diabetes.
● Plant-based diets can be healthy or unhealthy, depending on amounts of processed, ultra-processed or whole foods included.
● UK and US nutrition guidelines for prevention and management of type 2 diabetes recommend mainly or wholly plant-based, whole-food eating patterns, including Mediterranean patterns and the DASH (Dietary Approaches to Stop Hypertension) diet (Dyson et al, 2018; Evert et al, 2019).
● The ACC/AHA guideline on the primary prevention of cardiovascular disease (Arnett et al, 2019) recommends a diet that emphasises intake of vegetables, fruit, nuts, whole grains and fish, and reminds clinicians that, for primary prevention of ASCVD, “it is reasonable to minimize the intake of processed meats, refined carbohydrates and sweetened beverages.”
● For adults with type 2 diabetes, the ACC/AHA guideline recommends a tailored nutrition plan focusing on a heart-healthy dietary pattern to improve glycaemic control, achieve weight loss if needed and improve other ASCVD factors.
● Healthy plant-based eating patterns are low-glycaemic-index and high-fibre, contain multiple beneficial phytochemicals, including polyphenols, and have beneficial effects on the gut microbiome.
● Plant-based eating patterns increase microbiome diversity and increase numbers of bacteria that produce short-chain fatty acids, which have beneficial effects on weight and metabolism (Chen et al, 2021; Sharma et al, 2022).
● Plant-based diets contain as much, if not more, quality protein than omnivorous diets. All plant foods contain all amino acids, although some may be in small amounts. Eating a mixed, plant-based diet ensures optimal amounts of all amino acids, and no food combining is needed.
● Most people are eating too much protein, which cannot be stored in the body and so excess is converted to carbohydrates and fat. Most people would benefit from reducing protein intake by 25% and considering swapping 25% of protein intake from animal- to plant-based.
● Refined grains and added sugars should be avoided by everyone, whatever eating pattern is followed, but this is particularly important in people living with diabetes.
● “Eat more plants” is a simple message for healthcare professionals to deliver and people with diabetes to understand and implement (see Table 1).
● Whole-food, plant-based diets are good for health, including diabetes, and for the environment.
Take-home message: To optimise health, people with or without diabetes should eat a whole-food, unprocessed, mainly or fully plant-based diet.

Exercise in pregnancy – benefits for mother and offspring
Amy Valent (Chair), Linda May, Sylvia Badon, Samantha Ehrlich, Ana Barbara Alves Wagner
● Maternal obesity and hyperglycaemia during pregnancy increase the risk of early obesity and type 2 diabetes in the offspring through fetal programming. Effects may continue to the next generation (“grandoffspring”).
● Increasing physical activity to recommended levels (150 minutes of moderate-to-vigorous aerobic activity per week) can decrease gestational weight gain, GDM and lipids in obese and overweight women.
● 20 minutes of postprandial interval walking (repeated 3-minute slow and fast intervals), three times daily, may decrease postprandial glucose excursions in women with GDM, but effects are short-lived, so this needs to be continued daily (Andersen et al, 2021).
● 30 minutes of stepping daily (indoors or outdoors; cadence 100 steps/minute; 3000 steps per day) meets recommendations.
● Sedentary time is distinct from inactivity and has negative impact on all-cause mortality even in those who are otherwise meeting physical activity goals, except in the very-high-activity groups. During pregnancy, especially late pregnancy, sedentary time may increase.
● Pre-pregnancy sedentary time is not associated with GDM; however, sedentary time during pregnancy may be associated with GDM, and can increase risk of poor maternal and baby delivery outcomes and maternal metabolic disorders (Li et al, 2022). Decreasing sedentary time and replacing with light or moderate activity may also decrease the transgenerational impact.
● Further investigations are needed to identify differential impacts of various types and durations of exercise and how these differ between populations, as well as longer-term offspring outcomes.
Top 5 nutrition controversies
Gretchen Youssef (Chair), Alison Evert, Maureen Chomko
People with diabetes and healthcare professionals are “adrift in a sea of nutritional information and misinformation” that changes frequently, making it hard to give evidence-based advice. Large, rigorous nutrition trials are rare, and often short-term. Controlling interventions is difficult. Long-term implementation even of proven beneficial outcomes is challenging. Drug trials, by comparison, are much easier. This session set out to answer five of the most-asked questions regarding nutrition.
What is the optimal meal and snack frequency in diabetes?
● No evidence to support previous recommendations for three meals and snacks daily, but this increases caloric intake.
● Eating at breakfast time may improve postprandial glucose later in the day; skipping breakfast and eating large, late dinners may increase risk of CVD and type 2 diabetes.
● More rigorous human studies are needed to assess efficacy, mechanisms and sustainability of time-restricted eating (see Manoogian et al, 2022).
Macronutrients or calories – what is important?
● No optimal macronutrient (carbohydrate, fat, protein) mix for people with diabetes (MacLeod et al, 2017).
● Use CGM/SMBG to identify glucose fluctuations after a meal or specific food: “What could you do differently next time to improve blood glucose?”
● A variety of different eating patterns and calorie intake with varying macronutrient and calorie content can result in weight loss over 1–2 years.
● Shared decision-making and individualisation are useful; refer to a dietitian for guidance.
Food labels – “net carbs” and fibre
● Absorption of fibre and sugar alcohols (e.g. sorbitol) and their impact on blood glucose levels vary between people and over time, so “net carbohydrate” is not a useful concept.
● Eating more fibre is beneficial.
Artificial sweeteners (also see previous session)
● Non-nutritive sweeteners (NNS) vary in their structures, absorption, distribution, metabolism and excretion, so it is inappropriate to study them as a group.
● NNS and BMI: Randomised controlled trials show no difference or no weight loss. Cohort studies show a slight increase in BMI or modest long-term weight gain.
● NNS and metabolic effects: cohort studies only; slight increases in risk of type 2 diabetes and CVD (Azad et al, 2017).
● Many people of colour perceive tap water as risky, so encouraging water-drinking leads to purchase of bottled water and resultant economic burden.
● Instead, explore with open questions: “What do you think you could drink instead of soda?” or “You don’t like the taste of water – what else could you try?”
Note: The differing data on low-calorie sweeteners presented in the two sessions featured here highlight the ongoing controversies.
Are very-low-carbohydrate eating plans safe?
● Very-low-carbohydrate/ketogenic diets are defined as <20–50 g carbs/day, 10–26% of total energy.
● During the first 6 months of this eating pattern, compared with higher-carbohydrate diets, superior weight loss, decreased glycaemia, decreased medication; at 6–12 months, modest HbA1c reductions, significant medication reductions; at ≥12 months, no advantages (may be due to lack of adherence).
● Effects on lipids summarised in National Lipid Association Scientific Statement (Kirkpatrick et al, 2019):
- Over the short term, may improve triglycerides, LDL cholesterol and type 2 diabetes medication requirements (variable effects on LDL).
- By 2 years, no difference.
- Monitor lipids, especially if abnormal or high CVD risk.
● Monitor diabetes to minimise risk of hypoglycaemia and CVD risk factors.
- Decrease insulin dose.
- Ketogenic/very-low-carbohydrate diets are contraindicated if on an SGLT2 inhibitor. Stop the drug or avoid ketogenic diet.
● Refer to dietitian and psychologist or other support for behaviour change, if accessible.
● Monitor salt intake and BP, especially if on BP medication.
● May increase kidney stones; relative contraindication in disordered eating; microbiome shifts identified.





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025