State of the Nation
Clare Hambling, Chair of PCDS and National Clinical Director for Diabetes and Obesity, NHS England
Key NHS England initiatives on type 2 diabetes and obesity
● Healthier You Diabetes Prevention Programme – 1.7 million referrals.
- Self-referral possible for women who have had gestational diabetes.
- 20% reduction in risk of developing type 2 diabetes in those referred.
● Type 2 Diabetes Path to Remission – 26 000 referrals, 13 000 starts to date.
- Referral early after diagnosis improves outcomes.
● NHS Digital weight management programme – 12-week, web-based behaviour change programme.
- For those with BMI ≥30 kg/m2 (≥27.5 kg/m2 for high-risk ethnic groups) and hypertension, diabetes or both.
- Includes triage to three different levels of support according to needs: digital only, or digital with 50 or 100 minutes’ personal coaching.
- Also available, without referral, for NHS staff (same BMI requirements; valid NHS email address needed).
● NHS Healthy Living structured education:
- Digital programme available across England and accepting self-referrals.
- Core audit.
- Pregnancy in diabetes audit.
- Foot care audit.
- Inpatient safety audit.
- Gestational diabetes audit.
● Coming soon:
- New NHS England 10-year plan.
- NICE guideline: Type 2 diabetes (medicines).
- NICE guideline: Overweight and obesity.
- NICE technology appraisals: Teplizumab, Tirzepatide for obesity.
Multiple long-term conditions: The major transition in diabetes
Kamlesh Khunti, Professor of Primary Care Diabetes and Vascular Medicine, University of Leicester
● Use the term “multiple long-term conditions” (MLTCs) in preference to multimorbidity; this is defined as two or more conditions.1
● Historically, diseases were managed individually. Increasing numbers of people with multiple conditions has prompted NICE guidelines on how to manage MLTCs,2 emphasising a person-centred, holistic approach.
● MLTCs occur more commonly in those with diabetes, are associated with higher age and social deprivation, and result in poorer health-related quality of life, greater psychological and physical health needs, poorer physical function and higher mortality rates. People with MLTCs have complex health needs.
● Mechanisms linking the long-term conditions include inflammation and insulin resistance, and obesity has been highlighted as a potential target to reduce subsequent MLTCs.
● In a whole-population study of more than 60 million people across England in 2020, 29.3% overall had at least one long-term condition, 14.8% had two or more, 8.6% three or more, 5.2% four or more and 3.2% five or more.3
- Prevalence increased with age, (two conditions from age 20 years; four or more from age 40 years) and was two-times higher in the most versus the least deprived. No significant sex differences.
● People are living longer but in poorer health. Important to consider how many years people will live with a condition as well as how many years less they will live due to the condition.
- By age 50, one third of people with diabetes have three or more conditions, spend 20 years living with them and will die 11 years earlier than the general population.
- Each extra condition reduces life expectancy by 4 years.
- Hypertension, depression, cancer and coronary heart disease create the greatest burden of years spent and lost.4
- People with diabetes lose around 6 years due to the disease, whereas people with diabetes and cardiovascular disease lose an average of 12 years.
● Obesity is a driver for MLTCs. People living with BMI >35 kg/m2 have a 15-times higher risk of MLTCs.
● Medication non-adherence is significant. Solutions include coordinated care programmes, self-management education programmes, increasing encouragement to make lifestyle changes and system redesign.
- Medication adherence can be improved by multifaceted interventions, with those involving regular patient contact or education most effective.
● There is strong evidence for the legacy benefits of management options – 44 years for glycaemia, 10 years for blood pressure, 18 years for lipids and 21 years for managing multiple risk factors. Weight loss carries multiple benefits.
● It is important to avoid therapeutic inertia at all ages, particularly in those with MLTCs. Meanwhile, deintensification is important in older, frail people with diabetes and MLTCs.
Bookends of pregnancy
Professor Helen Murphy, Professor of Medicine, University of East Anglia
● What does a successful pregnancy outcome for a women with diabetes look like?
- No congenital malformations.
- Live birth and no stillbirth or neonatal death.
- No need for neonatal intensive care.
- No neonatal hypoglycaemia.
- Baby normal size (<90th centile).
- No birth injuries or delivery problems.
● Early-onset type 2 diabetes (age <40 years) has changed the demographics of diabetes in pregnancy:
- In 2002–2003, 27% had type 2 and 73% had type 1 diabetes.
- In 2022–2023, 57% had type 2 and 43% had type 1 diabetes.
● Single most important predictor of successful pregnancy is maternal glucose:
- Aim to keep HbA1c <50 mmol/mol in women with diabetes aged 15–50 years, in case of unplanned pregnancy.
- Goal is HbA1c <43 mmol/mol for women planning and preparing for pregnancy.
● HbA1c of 86 mmol/mol carries 10% risk of congenital malformations – avoid pregnancy if HbA1c is this high.
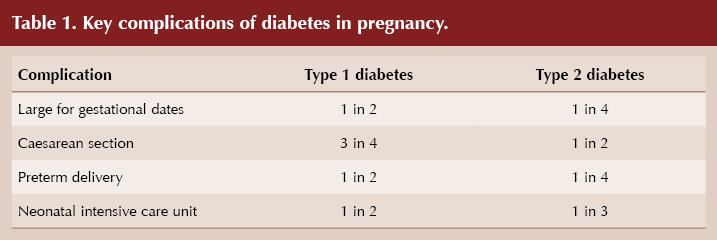
● Key complications of diabetes in pregnancy: see Table 1.
● Encourage all women under 50 with diabetes to use contraception until “pregnancy-ready”:
- Currently only one in 10 women with type 2 diabetes who get pregnant are well prepared, and this is unchanged in 10 years.
- Being “pregnancy-ready” reduces risk of a serious complication (stillbirth or serious heart or birth defect) from 10% to 2%.
● Type 1 diabetes: Use of CGM during pregnancy now up to 98%, with significant reductions in large-for-gestational-age babies, preterm deliveries and NICU need.
- Specific hybrid closed-loop systems which can operate at the low glycaemic settings needed in pregnancy rapidly improve time in range and gestational weight gain, and provide increased peace of mind for mum so she can enjoy her pregnancy.5
What can we do in primary care?
● Actively encourage contraception for all those with diabetes and HbA1c >48 mmol/mol.
● Remind about importance of avoiding unplanned pregnancy, and to discuss with us before discontinuing contraception.
● Encourage those with recently diagnosed type 2 diabetes to work towards remission.
● When glucose level controlled and “pregnancy-ready”:
- Ensure on 5 mg folic acid.
- Switch harmful medications (ACEi, ARB, glucose-lowering medications apart from insulin).
- Stop statins.
- Book with specialist team before 8 weeks’ gestation.
● Code all those with gestational diabetes. Ensure testing post-pregnancy to rule out type 2 diabetes, ensure annual HbA1c and weight check – see How to follow up gestational diabetes.
● Work with women to help them lose weight between pregnancies.






Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025