The Language Matters (NHS England, 2018) document highlights how important effective, understanding and emphatic language is when caring for people living with diabetes. The new model, called the Ormskirk Model, takes guidance from Language Matters and was collaboratively developed with healthcare professionals (HCPs) and those living with diabetes.
For too long, people living with diabetes have endured stigmatising messages and images about diabetes from the media, the public and – whether intended or not – HCPs. The Ormskirk Model helps both HCPs and people living with diabetes to identify resources, strengths and what is important to them. It enables the person living with diabetes to be seen and heard, rather than simply looking at the numbers.
A change in conversation
One conversational method that can be utilised in diabetes management uses assumptions and questions from solution-focused approaches (Guyers et al, 2019). Within the approach, the HCP is not seen as the ‘expert’ and more of a helpful visitor in the other person’s life. In a sense, the HCP’s greatest expertise is in asking exactly the right question at exactly the right time, rather than acting as a director using instructions based on an assumed knowledge of what’s good for the patient and what they should want.
Solution-focused approaches are potentially a good fit to discuss HbA1c or time-in-range (TiR). For example, Presseau et al (2010) found that people are more motivated to follow goals set by themselves – known as intrinsic motivation – as opposed to goals set for them by others. Sutton (1994) found that a good predictor of future behaviour is past behaviour. Within solution-focused approaches, revisiting how somebody did something well in the past is worthwhile. The approach encourages a focus on resilience, coping and personal resources to overcome past adversities (Guyers et al, 2019).
Why is a change needed?
Use of HbA1c scales by diabetes teams is widespread, yet the evaluation of how useful such scales are is nonexistent. Research has shown that the use of ‘scary’ images and words, ie ‘serious complications’, ‘very poor’ or ‘high risk’, is not beneficial and has the potential to be harmful (Dickinson et al, 2017). The majority of current scales and models are based on a medical model using a pathological approach that makes an attempt to scare people with diabetes about the risks of complications.
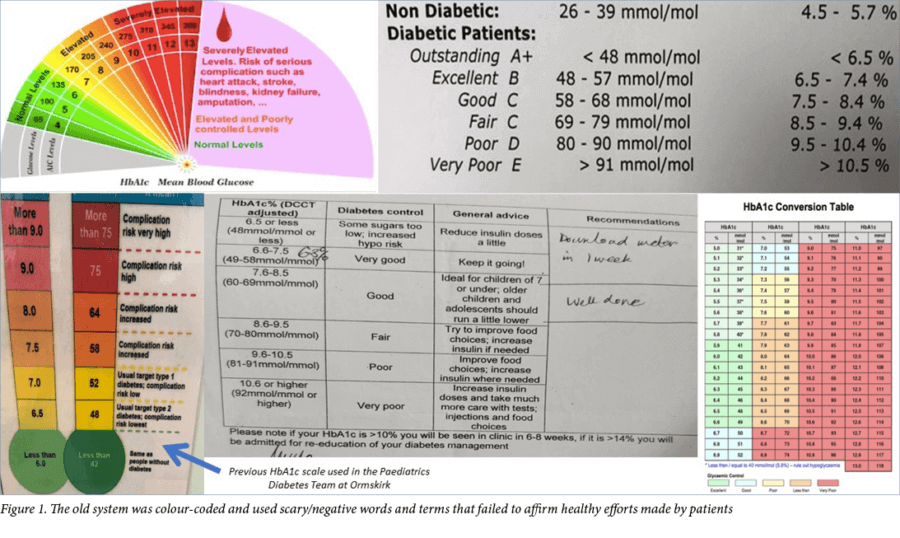
Within the Paediatric Diabetes Team at Ormskirk, HbA1c results were previously visually represented as a thermometer going from green to red, see Figure 1. These colours corresponded to high and low HbA1c. The results made reference to those ‘living without diabetes’ and had information relating to the potential risks listed next to them. A HbA1c >75 mmol/mol (>9%), for example, was aligned with the text ‘Complication risk very high’, see bottom left of Figure 1. The colour-coded thermometer did little to amplify and focus on what patients may have been doing well in their management, and did little to acknowledge that those who have been living with diabetes for many years were already well aware of complications.
HCPs can be tempted to become caught up in the numbers rather than the person in front of them. Similarly, we found that children and young people negatively referred to themselves after appointments, making comments such as ‘I’m still in the red zone’. Despite considerable effort being made and a reduction occurring within that colour zone, the old model failed to affirm healthy efforts.
A new approach: The Ormskirk Model
The Ormskirk Model approaches HbA1c and TiR in an emphatic and compassionate way, utilising concepts from solution-focused therapy. The ability to empathise is the foundation for any HCP’s training and subsequent interactions with patients and their families. The concept is discussed in policy, codes of practice and national clinical guidance (Derksen et al, 2013). The presence of empathy has been found to be particularly important in diabetes care outcomes (Hojat et al, 2011; Dambha-Miller et al, 2019). Dickinson and colleagues (2017) interviewed people living with diabetes and found that they had experienced judgement and blame through the language used by HCPs, friends, family and the general public. To be empathetic while considering the long-term complications and working with the patient and their family requires a whole-person approach. Polonsky et al (2017) found that inspiring people living with diabetes through the use of appropriate language can play an important role in engagement, management, treatment outcomes and the psychological wellbeing of the individual. For people living with diabetes, they found that language has a significant impact in increasing motivation, management behaviours and health outcomes.
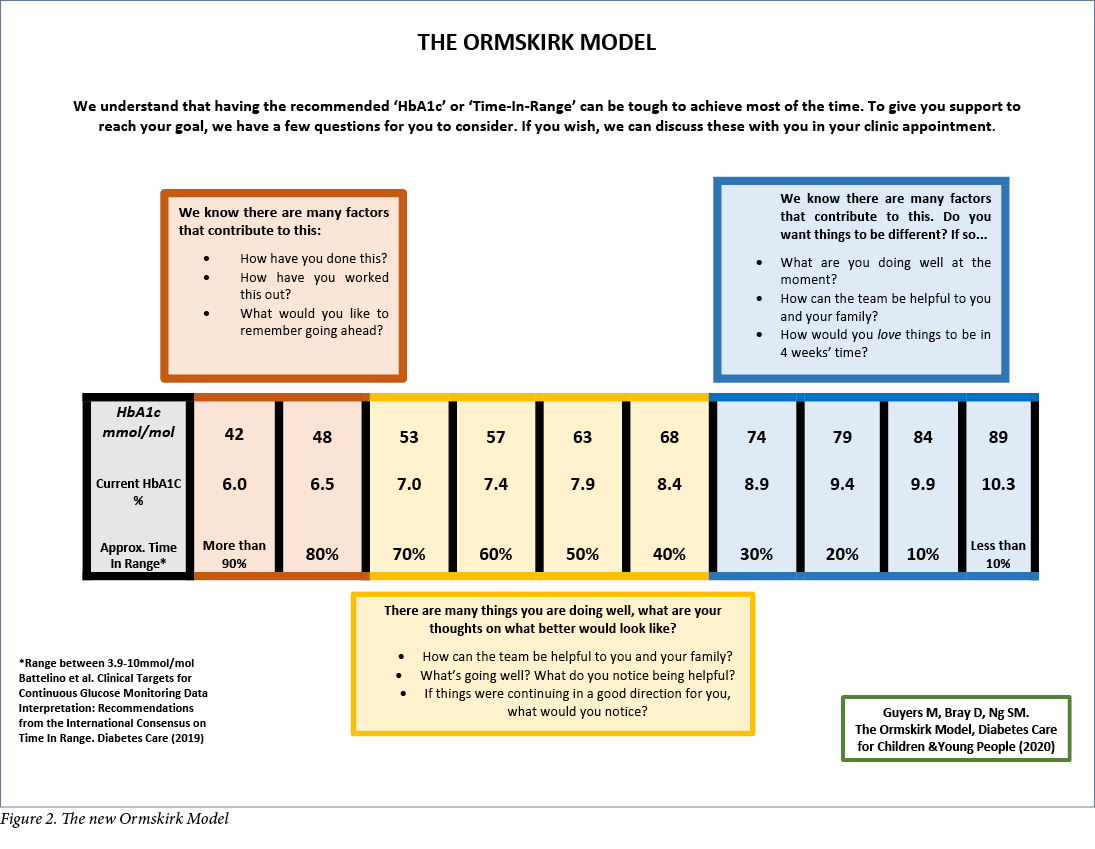
The Ormskirk Model promotes a conversation about any movements in HbA1c or TiR. The colour-neutral scale, see Figure 2, takes a timely step away from the previous traffic light image that categorised HbA1c into ‘good’ and ‘bad’ colours. With the use of neutral colour, there is a lack of immediate judgement of the child or young person living with diabetes. Instead there is a focus on affirming efforts made by patients and their families to manage their diabetes.
The ‘complications’ component has been removed from this new model. It avoids language such as ‘complications’, ‘risks’ and ‘good/poor/very poor’.
For people living with diabetes and their families, the meaning and understanding of what ‘good for them’ might look like is potentially very different to others. The model attempts to enquire how diabetes (no matter what the HbA1c or TiR reading) is managed by that individual and their family. There is a renewed assumption that people living with diabetes are doing what they can at this moment in time, until proven otherwise, and the HCP can enquire what that is.
The model asserts that it is time to move away from the word ‘control’, which originated from the Diabetes Control and Complications Trial (Nathan et al, 1993). Attribution of the ‘ability to have control’ or ‘a lack of control’ is a consequence of this. According to Broom and Whittaker (2004), this type of messaging positions people with diabetes as ‘defiant children’ or as ‘dreadful or reckless adults’, which is contradictory and confusing for people with diabetes.
The American Psychological Association (2010) has long endorsed the person-first perspective in an effort to reduce stigma, stereotyping and prejudice toward people with disabilities; this applies to those working in clinical practice, research, and education. Utilising person-first language respects the whole individual rather than their diagnosis, which is only one part of their life experience (Dunn et al, 2015). The Ormskirk Model utilises language that facilitates people in their identification of and work towards what matters to them through the use of rhetorical questions. Connecting with the children and young people’s families, we provide support through words, images and symbols grounded in values that help make new ways of thinking and behaving accessible and relevant to their busy lives.
Use in clinical practice: less judging, more valuing
The Ormskirk Model is present in each Ormskirk Diabetes Team clinic room and is displayed in the waiting room in a bigger A3 format. It can be used as a visual prompt for patients and HCPs. The model can encourage reflection from the person living with diabetes and the HCP, gently focusing their attention on strengths, rather than deficits. The Ormskirk Paediatric Diabetes Team members find that they are now continually ‘in step’ with children and young people and their families, and are more aware of what works for them.
To download a pdf of the Ormskirk Model, click here
Correspondence to: Dr May Ng [email protected] or @mayng888
Acknowledgements
Thank you to Dr Rebecca Simm, Southport & Ormskirk Paediatric Diabetes Team (Lynne Finnigan, Helen Day, Michelle Quinn, Alison Hannah, Linda Connellan, Dona Pintus), Ashley Ng, Rosie Walker and all the children, young people and their families at Southport & Ormskirk Hospital NHS Trust. To the diabetes community on Twitter – thank you for your time in reading and making suggestions to improve the Ormskirk Model. It would not be what it is without your input. Your passion for ‘what good in diabetes care should look like’ is an inspiration to everyone.
The Ormskirk Model is free for all diabetes teams to use with the source acknowledged whenever used. It has been translated into over 20 languages including Welsh, Telegu, Mandarin, Arabic, Portuguese, Bulgarian, Dutch, Greek, German, Malay, Romanian, Latvian, Italian, Hindi, Urdu, Tagalog, Russian, Spanish, French and Polish. Translations are available for download if you click here.




NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022