Chronic kidney disease (CKD) confers increased risk of end-stage renal disease, cardiovascular disease and death, and this risk increases as urinary albumin levels rise and estimated glomerular filtration rate (eGFR) falls.
The majority of people with moderate-to-severe CKD are managed in primary care. In addition to the management considerations listed in Box 1 (Diggle, 2017), optimising blood glucose levels is of crucial importance as hyperglycaemia drives the initiation and progression of CKD (Alicic et al, 2017), and intensive glucose control has consistently been shown to reduce the risk of albuminuria (Coca et al, 2012).

In addition, emerging evidence suggests that the sodium–glucose cotransporter 2 (SGLT2) inhibitors in particular may have renoprotective effects independent of their effects on blood glucose, such that the American Diabetes Association and European Association for the Study of Diabetes now prioritise their use after metformin in people with type 2 diabetes and CKD (Davies et al, 2018; Buse et al, 2020). Although SGLT2 inhibitors are not currently licensed for initiation in people with an eGFR <60 mL/min/1.73 m2, they can be used in those with albuminuria and an eGFR ≥60. This is an important group who may make up 10% of the population with type 2 diabetes, and at this early stage it may be possible to reverse albuminuria.
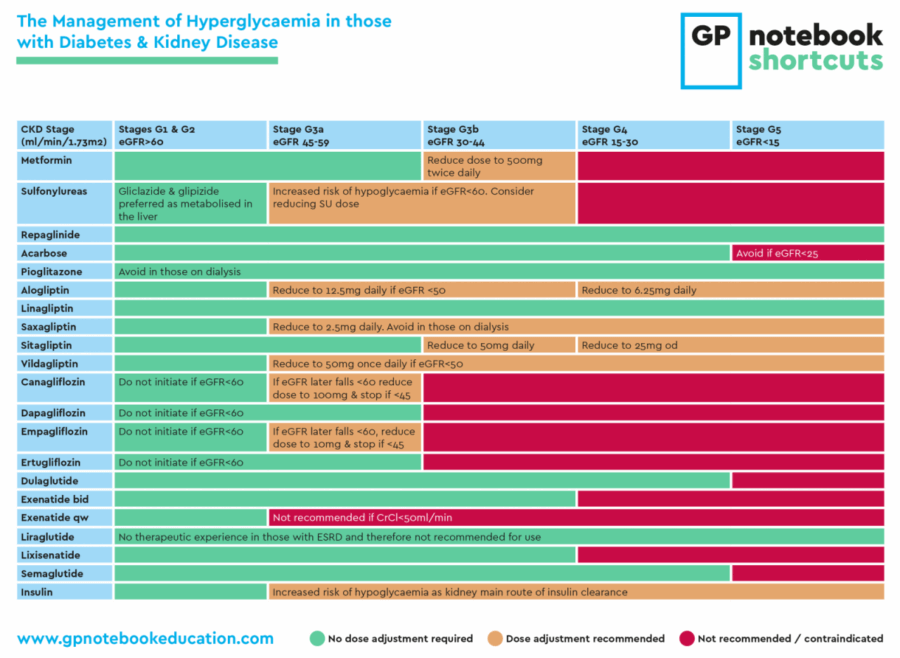
However, optimising glycaemic control in people with CKD is complicated by the alterations in glucose homeostasis and drug pharmacokinetics that result from reduced kidney function (Neumiller et al, 2017), such that the majority of antidiabetes drugs will require dose adjustment or discontinuation as eGFR decreases.
This GPnotebook Shortcut provides a concise summary of the indications and dosing recommendations of antidiabetes drugs in people with diabetes and CKD.
GPnotebook Shortcuts
GPnotebook Shortcuts are a series of easily digestible, bite-sized resources to help clinicians manage their patients in primary care. A full list of Shortcuts can be found here.
GPnotebook Education
GPnotebook Education is an independent educational resource which has been created with primary care professionals in mind and mirrors the daily work in primary care, using multiple patient case studies to cover latest clinical guidance, research and hot topics.
All GPnotebook Education courses provide unbiased, independent content, prepared and presented by fellow healthcare professionals. Visit gpnotebookeducation.com to learn more.





Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025