Despite our having many guidelines that allude to the importance of relaxing HbA1c targets for the older or frail person, in practice this has not happened consistently. Both in this journal and in Diabetes & Primary Care, good practice audits have been suggested to identify those who are put at risk by HbA1c levels that are lower than ideal and indicate a high risk of unrecognised hypoglycaemia. Much good work has been achieved to this end; however, what I hear all too often is, firstly, the lack of confidence to de-escalate therapy and, secondly, uncertainty of what to do if the subsequent HbA1c levels start to rise above the ideal target range.
New frailty advice
The recognition of frailty as an important aspect of care in this year’s Quality and Outcomes Framework is a massive step forward in ensuring that this vulnerable group has safer HbA1c targets set. For those with moderate to severe frailty, the target HbA1c level is set at 75 mmol/mol (9.0%). Although this is helpful as a target figure, we still need to be aware of how to achieve it safely, and recognise that this is not an acceptance to withdraw care completely in this vulnerable group.
The recently published position statement from the Association of British Diabetologists, Managing frailty and associated comorbidities in older adults with diabetes, addresses this important and challenging area of diabetes care (Sinclair and Gallagher, 2020). Alan Sinclair himself describes the clinical significance of frailty and describes the statement in greater detail elsewhere in this Journal. However, briefly, the statement divides neatly into three areas:
- Establishing frailty: How we all need to be able recognise and measure frailty status.
- Key areas for medical management: Targets and advice on all medications, including beyond glycaemic management (blood pressure and lipid management). This section also highlights the importance of avoiding hypoglycaemia.
- Audit tools: These are suggestions of how areas or individual services can assess the effectiveness of any interventions for this population.
This statement is a welcome addition to the current advice in this area, and it neatly encapsulates all the current evidence. It offers practical suggestions and advice to all healthcare providers for not only glucose control but also the challenging decisions to be taken regarding when to reduce and/or withdraw blood pressure and lipid management therapies.
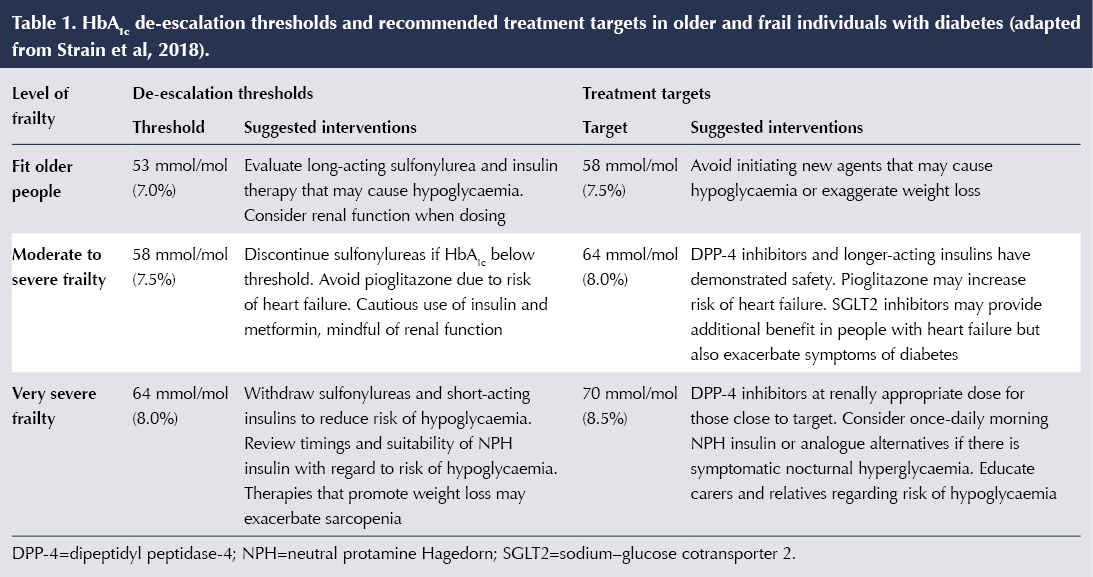
I would like to take this opportunity to also highlight an additional document that focuses on frailty: Type 2 diabetes mellitus in older people: a brief statement of key principles of modern day management including the assessment of frailty. A national collaborative stakeholder initiative (Strain et al, 2018). The purpose of highlighting this is the document’s focus on suggesting HbA1c thresholds at which to start de-escalating medications and advising on which medication groups to consider stopping (Table 1). These two documents are, I believe, an incredible resource for us all.
Updated ADA/EASD guidance
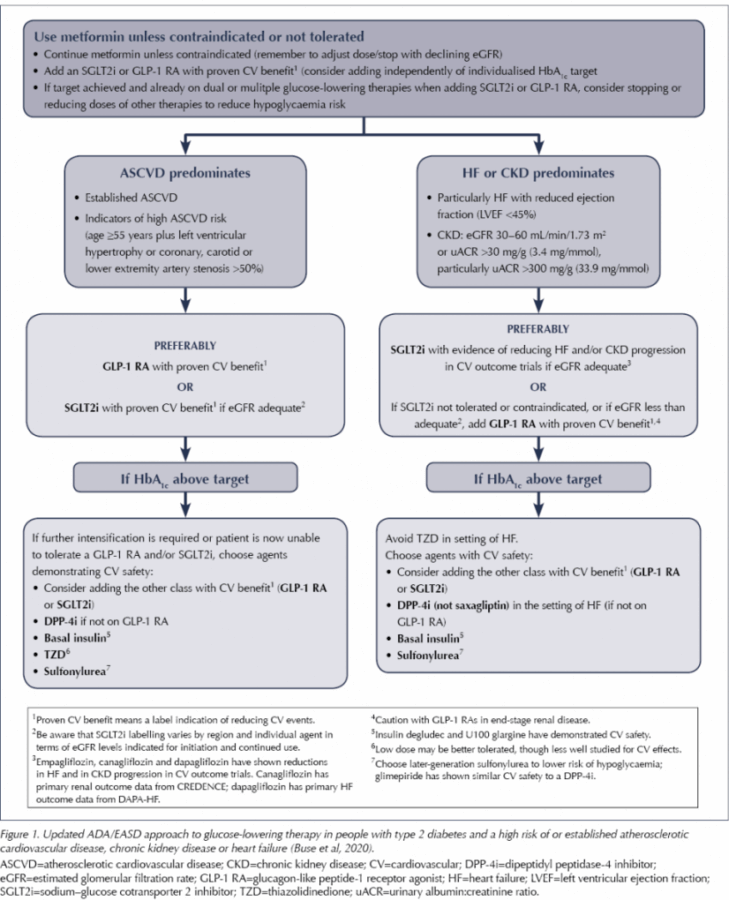
Other important clinical guidance that has just been released is from the American Diabetes Association and European Association for the Study of Diabetes (ADA/EASD), who have updated their consensus report on the management of type 2 diabetes (Buse et al, 2020).
In a previous editorial, I highlighted the significant results seen from cardiovascular outcome trials and the real need for us all to become far more familiar with, and competent in, the recognition of heart failure in our patients with diabetes (Down, 2019). This update to the ADA/EASD consensus statement reinforces the incredible advances seen in two of our therapy classes. In addition to treating people with established atherosclerotic cardiovascular disease, heart failure or chronic kidney disease with either SGLT2 inhibitors or GLP-1 receptor agonists second-line to metformin, the ADA/EASD have taken this advice further, and now recommend these therapies for all patients at high risk of these complications (Figure 1). The most crucial factor in the new advice is that, for this higher-risk population, the use of SGLT2 inhibitors or GLP-1 analogues is irrespective of baseline HbA1c. This signifies the huge benefit of these two classes of medication, over and above their effects on glucose lowering.
This, for me, really signifies an exciting start to 2020!




Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025