To qualify as a nurse prescriber, nurses must undertake a recognised Nursing and Midwifery Council (NMC)-accredited prescribing course through a UK university. Upon successful completion, the qualification must be registered with the NMC and individuals must obtain authorisation to prescribe from their employer (usually the Hospital or Community Trust).
There are three types of non-medical prescribing:
- Independent prescribing. Independent prescribers are responsible and accountable for the assessment of people with undiagnosed and diagnosed conditions, and for decisions about the clinical management required, including prescribing. Independent nurse and pharmacist prescribers are able to prescribe any medicine, including certain controlled drugs, for any medical condition within their competence. Optometrist independent prescribers can prescribe any licensed medicine for ocular conditions, but cannot prescribe any controlled drugs. Physiotherapist and podiatrist independent prescribers can prescribe any licensed medicine that falls within their individual area of competence, but cannot prescribe any controlled drugs.
- Supplementary prescribing. Supplementary prescribers may prescribe any medicine, including controlled drugs, within the framework of a patient-specific clinical management plan that has been agreed with a doctor. Nurses, pharmacists, physiotherapists, chiropodists or podiatrists, radiographers and optometrists may train and register as a supplementary prescriber.
- Prescribing by community practitioners from the Nurse Prescribers’ Formulary for Community Practitioners. Community practitioners (including district nurses, health visitors and school nurses) are able to prescribe independently from a limited formulary, the Nurse Prescribers’ Formulary for Community Practitioners (British Medical Association, 2015). This comprises a limited range of medicines, dressings and appliances suitable for use in community settings.
Since the introduction of nurse prescribing, many legislative changes have taken place to implement the Government’s policy of extending prescribing responsibilities to non-medical professions (Department of Health [DH], 2000; 2006). Non-medical prescribing is an integral part of the larger agenda to modernise the NHS, to work in different ways and to change traditional professional roles and responsibilities. The DH (1999) re-affirmed the Government’s intention to “…extend the role of nurses, midwives and health visitors to make better use of their knowledge and skills – including making it easier for them to prescribe”. The primary aim was to improve patients’ access to treatment and advice, to make more effective use of the skills and expertise of groups of professionals, to improve patient choice and convenience, and to allow for more flexible team working across the NHS.
According to the RCN (2012), prescribing has the potential to increase nurses’ autonomy, job satisfaction and independence. There is also evidence that nurse prescribing can improve patient care by ensuring timely access to medicines and treatment, and by increasing flexibility for patients who would otherwise need to wait to see a doctor (Carey and Stenner, 2011). Patient satisfaction with nurse prescribing is high (Courtenay et al, 2015), and the RCN (2012) has highlighted how nurse-led diabetes services in which nurses are authorised to prescribe allow for more streamlined and patient-focused care. There is, however, a shortage of empirical evidence that supports the clinical and economic outcomes for nurse prescribing. What is clear, however, is that nurse prescribers are taking on a higher level of clinical responsibility.
Proficiencies and continuing professional development
The NMC (2006) published the Standards of proficiency for nurse and midwife prescribers. In relation to accountability (Practice Standard 2), it specifies that nurse prescribers are professionally accountable for their prescribing decisions, including actions and omissions, and cannot delegate this accountability to any other person, and that they must only ever prescribe within their level of expertise and competence.
Practice Standard 15 relates to continuing professional development (CPD), and states the following:
15.1 It is your responsibility to remain up-to-date with knowledge and skills to enable you to prescribe competently and safely.
15.2 You must act in accordance with Clause 6 of The NMC code of professional conduct: standards for conduct, performance and ethics.
15.3 As a nurse or midwife who is recorded on the register as being a prescriber, you should ensure that your continuing professional development is in line with your role as a prescriber.
There is an acknowledgement that employers have a responsibility to ensure that prescribers have access to undertake the relevant CPD, as identified through their staff appraisal, but ultimately the responsibility to ensure these standards are upheld appears to lie with the prescribers themselves.
The NMC (2008) produced CPD guidance for nurse and midwife prescribers, the principles of which are listed in Box 1.
The Code and revalidation
In January 2015, the NMC published its revised code of professional standards that nurses and midwives must uphold in order to be registered to practise in the UK (NMC, 2015). Effective from 31 March 2015, the new Code was structured around four themes – prioritise people, practise effectively, preserve safety and promote professionalism and trust.
The NMC exists primarily to protect the public. Partly prompted by the Francis Report (Mid Staffordshire NHS Foundation Trust Public Inquiry, 2013), in December 2015, the NMC introduced a mandatory system of revalidation, similar to that of the General Medical Council, as a means of reinforcing the status and competencies of registered nurses and providing additional protection to the public.
Revalidation replaces Post Registration Education and Practice and is the process by which registered nurses and midwives are required to regularly demonstrate to the NMC that they remain fit to practise and adhere to the revised Code.
Every nurse and midwife is required to confirm that they:
- Continue to remain fit to practise.
- Have met the requirements for practice and CPD.
- Have sought and received third-party feedback, which has informed their reflection on their practice. This feedback could be from patients, carers, students (for educators) or peers.
- Have sought and received third-party confirmation that they are fit to practise. A third party (likely to be a manager, another registrant or a supervisor) will need to confirm that the nurse or midwife is adhering to the Code and standards, and is fit to practise.
Within the revised Code, nurses will be required to undertake 35 hours of CPD every 3 years, 20 hours of which have to be committed to “participatory” learning (e.g. learning workshops or shadowing colleagues). Nurse prescribers will need to collect evidence that will validate their competence in relation to their prescribing role, with an emphasis on reflection on practice and feedback as a means of highlighting good performance and identifying areas that might need improvement.
Nurse prescribers must take responsibility for their own CPD. A portfolio structured according to the four sections of the revised NMC Code is recommended for compiling evidence to support revalidation. Nurse prescribers should ensure that there is evidence within their portfolio to validate their prescribing competency. There should be clear evidence of ongoing CPD demonstrating reflective practice, with evidence of educational courses, patient testimonials and reflective learning. It is recommended that the portfolio be structured according to the four sections of the NMC Code (prioritise people, practise effectively, preserve safety and promote professionalism).
The portfolio provides useful information upon which to base the annual appraisal and discussion around personal development. A professional development discussion with another NMC registrant, which includes a review of reflections on the Code, CPD and practice-related feedback, is required for revalidation. There is also a requirement to record a minimum of five written reflections on the code of conduct, feedback and CPD, and these should encompass the prescribing role.
Support for revalidation
The NMC is clear that employers have a responsibility to support their staff to meet CPD requirements (NMC, 2016). In relation to prescribing, the Standards of proficiency for nurse and midwife prescribers state that employers have a responsibility to ensure that prescribers have access to undertake the relevant CPD as identified through their staff appraisal (NMC, 2006). However, there is no legal requirement for employers to provide time for CPD-related learning.
A fact sheet published by the RCN (2016) suggests that best practice in the UK is for employers to negotiate with their nursing staff on how much CPD time they need for the coming year, usually agreed during a nurse’s annual appraisal. It is, however, up to the employer and the nurse to negotiate funding and agree time.
Launched in December 2012, Compassion in Practice (DH, 2012) was the new 3-year vision and strategy for nursing, midwifery and care staff, drawn up the Chief Nursing Officer for England and the Director of Nursing at the Department of Health. Six fundamental values were identified as underpinning effective nursing practice: care, compassion, competence, communication, courage and commitment (the “6Cs”). The strategy recognises that, to make this vision a reality, nurses need to be in supportive organisational cultures. Hopefully, Government commitments specific to nursing covering staffing levels, support for nurses, leadership within the profession and ways to measure and monitor quality care will provide nurses with some leverage with which to ensure their employers provide the appropriate level of support for CPD.
Competency frameworks
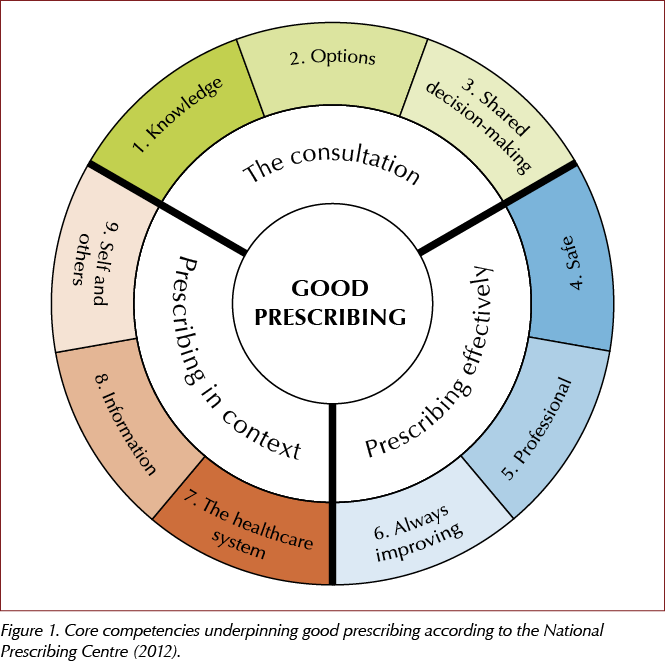
In 2012, the National Prescribing Centre (NPC) published A single competency framework for all prescribers, describing the core competencies that underpin good prescribing, regardless of professional background (NPC, 2012).
The framework comprises three domains, each containing three dimensions of competency, as illustrated in Figure 1. Within each of the nine competency dimensions in total, there are statements describing the activity or outcomes prescribers should be able to demonstrate. It provides an outline of common prescribing competencies that, if acquired and maintained, could help prescribers to become and remain effective prescribers in their area of practice.
The NPC website was subsequently decommissioned, although it is still possible to access an archived version of the competency. It is, however, important to know that this has not been updated and some of the content may be out of date. Some of the principles within the document have been incorporated into the medicines optimisation guideline (NG5) published by NICE (2015).
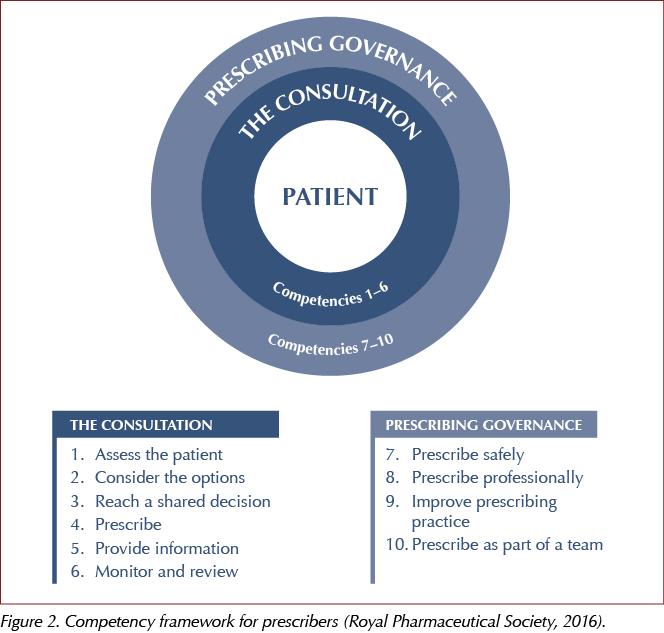
Frameworks do provide a useful template upon which to highlight good prescribing practice and identify areas for improvement. The Royal Pharmaceutical Society (2016) has published its own competency framework. Within this framework (Figure 2), there are ten competencies, split into two domains. Within each of the ten competency dimensions, there are statements that describe the activity or outcomes prescribers should be able to demonstrate.
Concluding remarks
Of course, all non-medical prescribing is underpinned by legislation and regulatory standards. All nurse prescribers are required to record their prescribing qualification with the NMC. They also have a responsibility to remain up to date with the knowledge and skills that enable them to prescribe competently and safely.
Diabetes is a complex and challenging condition to manage effectively. With new therapies being launched on a regular basis, there has never been a greater need for nurse prescribers to demonstrate prescribing proficiency.





Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025