On 10th October 2019, the pregnancy outcomes in diabetes for the year 2018 were published (NHS Digital, 2019). Whilst overall the situation in terms of outcomes did not worsen in 2018, sadly there has not been any improvement over the 5 years that the report has been published, either. This means that there remains a higher rate of stillbirth and neonatal death, along with congenital abnormalities, in women with pre-existing diabetes compared with the general population.
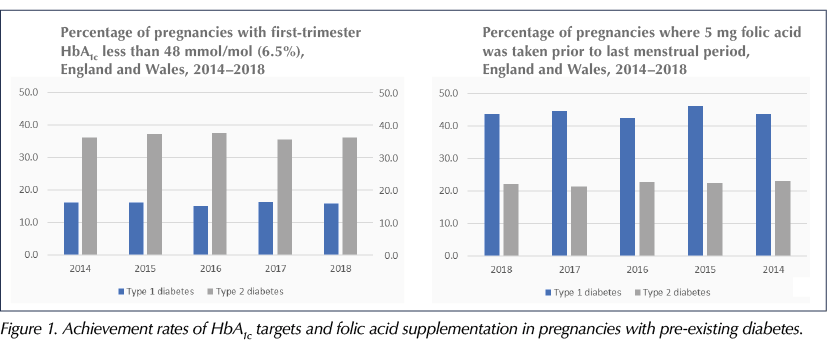
For the first time in the report’s history, women with type 2 diabetes outnumbered those with type 1, and although fewer women with type 2 diabetes were taking statins, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers and antidiabetes agents other than insulin and metformin than in previous years, suggesting some improvement over time, rates of folic acid supplementation and achievement of glucose targets remain suboptimal.
The rise in the number of women with pre-existing type 2 diabetes has important implications for us all. The reason for, and importance of, this rise is multifactorial. It clearly demonstrates that ever more people are being diagnosed with type 2 diabetes at a younger age and that women are choosing to have children at a later age. These women most often receive their diabetes care in general practice. They are more likely to be hypertensive, have a higher BMI and often to have other long-term conditions. These factors pose additional challenges to an already medicalised pregnancy.
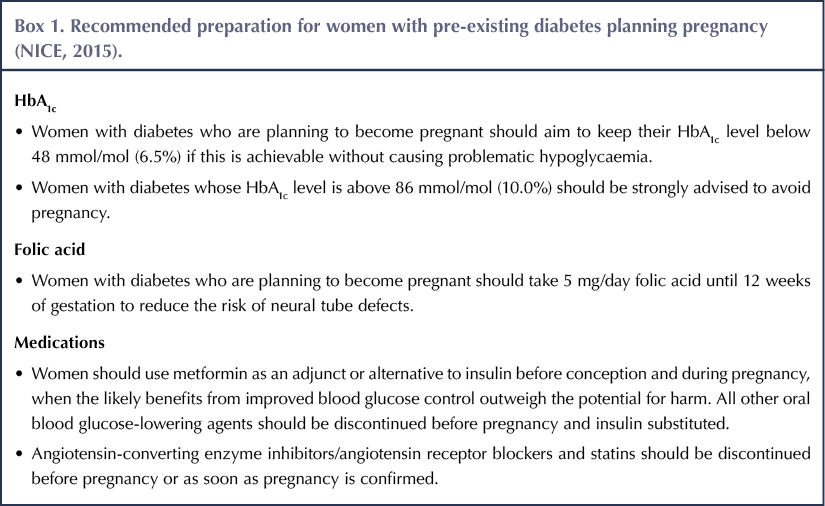
Neither women with type 1 nor type 2 diabetes receive adequate preparation for pregnancy, as listed in Box 1. These figures are not improving at all. In fact, staggeringly, seven in every eight women did not receive the NICE-recommended pregnancy preparation to reduce their risk. Other factors that remain astonishingly poor are the numbers of women who achieve the recommended HbA1c target of 48 mmol/mol (6.5%) prior to conception (see Figure 1). Again, the higher the HbA1c at conception, the higher the risk of fetal abnormality. Not only is there an increased risk to the fetus from poor glycaemic control, but also the mother is at increased risk of pre-eclampsia or worsening of any previous diabetes complications, such as retinopathy and nephropathy, if glucose control is optimised quickly in the early weeks of pregnancy.
So what needs to be done?
What can we take from this report? Given that it demonstrated that this issue is uniform across England and Wales, calls have been made for a whole-system approach to tackle this issue. Once pregnant, it is too late to achieve the maximum benefit of folic acid supplementation or glucose optimisation.
There has to be a system-wide approach to identify women of childbearing age with either type 1 or type 2 diabetes, and ensure they are aware of the risks of an unplanned pregnancy. This should then be recorded in their medical records (much as we record discussions regarding hypoglycaemia and driving).
As healthcare professionals, we have to be extremely mindful of prescribing or recommending medications not licensed for use in pregnancy to women of childbearing age unless we are aware of their contraceptive status. We need to ensure that women are aware of the risks and we need to record that these discussions have taken place.
So we have lots to aim for in 2020, and I feel that a real focus on the management of women of childbearing age and an increased awareness of the risks of an unplanned pregnancy, across primary care, should be our New Year’s resolution!
On that note, I wish you all a very Merry Christmas and prosperous New Year, and I look forward to more reviews and challenges in my editorials throughout 2020.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025