The fundamentals of type 1 diabetes management have remained unchanged since the discovery of insulin in the 1920s – principally the measurement of blood glucose levels and replacement insulin therapy. New technologies have been developed throughout the 20th and into the 21st century. Pivotal to these developments has been the invention of continuous subcutaneous insulin infusion (CSII) therapy, more commonly known as the insulin pump.
Insulin pumps were developed for research in the early 1970s; however, they were very large in size and not suitable for use outside of the hospital setting. In 1976, the first insulin pump suitable for outpatient use was developed by Dean Kamen (who, interestingly, would also go on to invent the Segway, the electric self-balancing scooter). However, it was not until the start of the 21st century that access to insulin pump therapy, especially in children and young people, started to significantly increase. Despite this uptake in use, the evidence base to support such a therapy change was yet to be established.
Developing the evidence base
Use of insulin pumps in children and young people with type 1 diabetes did not significantly occur until the turn of the new millennium. Alongside this increased use saw the undertaking of more studies to acquire a rigorous evidence base for this developing therapy. Much of the data support the use of insulin pumps in this population (Sherr et al, 2018). Improvements in glycaemic control, often the primary outcome measure, ranged from a miserly 2 mmol/mol (0.2%) through to a clinically significant 11 mmol/mol (1.0%). Much of these data, however, were generated in studies that were not randomised, had very small numbers of participants or had short durations (Blair et al, 2019). Whilst good-quality evidence proved difficult to generate in the paediatric population, high-quality randomised controlled trials in adult populations have long shown positive glycaemic effects, with one meta-analysis showing improvements in HbA1c of over 4 mmol/mol (0.4%) versus control groups on multiple daily injections (MDI; Jeitler et al, 2008).
Since the DCCT (Diabetes Control and Complications Trial Research Group, 1993) showed that intensive diabetes management reduces the incidence of complications, the balancing act of intensively managing one’s diabetes and maintaining quality of life has been ongoing. As a side note, there was a large number of participants using insulin pumps as a part of the intensively managed cohort in the DCCT, and they achieved mean HbA1c levels 2–5 mmol/mol lower than their peers on MDI (Pickup, 2009).
Of course, whilst glycaemia is a vital outcome in the successful management of type 1 diabetes, it is important to acknowledge that there are other measures. More intensive diabetes management, as described in the DCCT, significantly increases the risk of severe hypoglycaemia (DCCT Research Group, 1997). A consistent observation noted in the literature following the uptake of insulin pump therapy was a reduction in both the frequency and severity of hypoglycaemia (Sherr et al, 2018). Hypoglycaemia is regularly described as one of the biggest worries for families supporting children with type 1 diabetes, and insulin pumps can be used to alleviate this (NICE, 2008). Like glycaemia, quality of life measures have had mixed results in studies. However, a consistent theme has been that the quality of life for the families supporting the child with diabetes improves significantly with insulin pump therapy. This is particularly pertinent to those with younger children; therefore, insulin pump therapy is often offered to all children under around 7 years of age (Sundberg et al, 2017).
NICE guidance
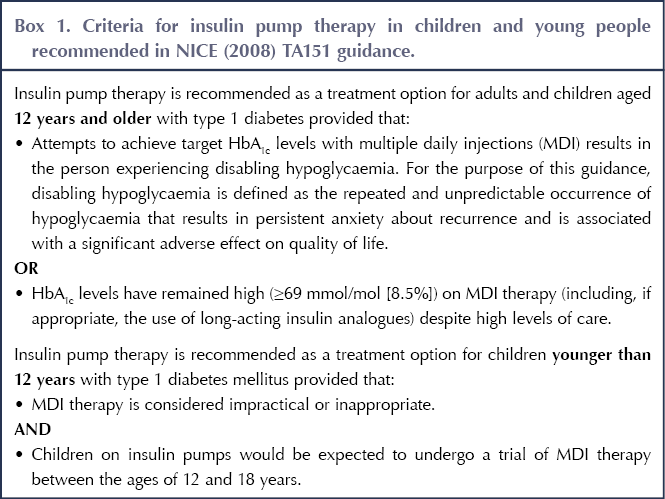
NICE is particularly clear about when insulin pump therapy can be beneficial in children and young people. The NICE (2008) TA151 guideline suggests the criteria outlined in Box 1. However, this advice is over a decade old and, while it is almost certainly still useful as a conversation starter, it could be questioned whether these criteria are still useful for patient selection. Twelve years seems an arbitrary age at which to “change the rules”, especially given the profound differences in access to pump therapy suggested: children under 12 years have very open access, whilst those over 12 are more limited. Anecdotally, many families find it particularly galling that good glycaemic control is used against them, as a reason to take away their insulin pump, during adolescence.
It should be noted that large improvements in glycaemic control have been observed in patients with suboptimal HbA1c at the start of insulin pump therapy (Sherr et al, 2018). There is an important discussion to be had regarding the ethics of stopping a treatment that may be working very successfully in order to trial a different therapy. How many clinicians would be comfortable advocating a change in therapy modality in a patient who has achieved an HbA1c of 50 mmol/mol (6.7%), minimal episodes of hypoglycaemia and positive quality of life? As shared decision-making becomes increasingly important in modern healthcare, this didactic guideline seems painfully out of date.
Pumps at diagnosis?
The recently published SCIPI (SubCutaneous Insulin: Pumps or Injections) trial has offered much to think about regarding the use of insulin pumps in the paediatric age group (Blair et al, 2019). This is one of the first UK-based, multicentre, randomised controlled trials to evaluate insulin pump therapy from diagnosis in children and young people with type 1 diabetes. Alongside glycaemic outcomes, a cost-effectiveness evaluation was also completed. At first glance, the results showed no clinically significant differences in glycaemic outcomes between CSII and MDI. In fact, mean HbA1c was marginally better in the MDI group. The study authors conclude that initiating insulin pump therapy in the first year of diagnosis of diabetes is not a cost-effective choice.
The SCIPI trial raises some interesting questions around when and how insulin pump therapy should be used in the therapeutic journey for a paediatric patient. The results are perhaps not as surprising as they seem. Diagnosis of diabetes is a troubling time for families; there are often misplaced feelings of guilt. A strong, persistent grief, with symptoms akin to post-traumatic stress disorder, has been observed in some families (Landolt et al, 2002). Educating families on diabetes fundamentals with this level of psychological trauma is difficult, and is often made more so by lack of sleep and with the education taking place in a hospital setting. As per the SCIPI study design, participants randomised to insulin pump therapy were instructed in the use of the device, including advanced features, within 2 weeks of diagnosis. This is a tremendous ask for families who have already experienced, and are continuing to deal with, feelings of grief and possibly trauma. The SCIPI report rightly recognises this as one of the limitations in the applicability of its findings to practice.
In addition, the education component of the study was not standardised; curricula were reviewed to ensure that they met appropriate criteria but, due to limits in cost and time, a standardised education pathway for insulin pump use was not used. Again, the report acknowledges this potential weakness in the design, but does attempt to counter that by suggesting that all pump trainers in the study were experienced members of the diabetes teams. SCIPI clearly describes itself as a pragmatic randomised controlled trial; it acknowledges that education may have been an issue.
The SCIPI authors should be congratulated on completing such a well-powered, “gold-standard” trial in this area, one that was much needed. However, one could question whether this an area in which the randomised controlled trial should be considered the gold standard.
Patient registry data
Throughout the world, patient registries for children and young people with type 1 diabetes are increasingly being used. The National Paediatric Diabetes Audit (NPDA) acts as a form of registry for England and Wales, and there is the DPV in Germany and Austria, and the Type 1 Diabetes Exchange in the US. In addition, the SWEET initiative is a multinational registry. These registries serve, amongst other functions, as a record of patients’ glycaemic control and treatment modality, as well as ensuring individual clinic conformity to standards. Proponents of both the randomised controlled trial and the population study could argue that the one counters the other’s deficiencies.
Reviews of registry-wide data have shown that children and young people using insulin pumps have better glycaemic control than their peers using intensive injection regimens (Sherr et al, 2016). Registry data do highlight some startling differences between our practice in England and Wales and that in our German/Austrian and US peers. In 2016, Germany and the US had 41% and 47% of paediatric patients, respectively, using insulin pumps, whilst England and Wales had a rate of only 14% (Sherr et al, 2016). Differences in mean HbA1c across the registries was also striking, with both European and American registries showing averages 5–10 mmol/mol lower than the NPDA, regardless of treatment modality. There is much to be encouraged about, however. The proportion of patients on insulin pump therapy in the most recent NPDA has shown a large increase, to over 30% (Royal College of Paediatrics and Child Health, 2019), perhaps signalling a shift in professional experience and attitudes towards insulin pump therapy. This increase in the number of children and young people using insulin pumps has mirrored the proportion of those achieving glycaemic control closer to targets. Whether this relationship is causal is a matter for debate, however, as it has also coincided with the increase in investment since the introduction of Paediatric Diabetes Best Practice Tariff.
The future: Closed-loop systems
A review of the evidence pertaining to the use of insulin pumps in children and young people will provide a mixed picture. However, should the use of insulin pumps be considered as a necessary step? Closed-loop systems, often known as the artificial pancreas, have finally come to fruition. The closed-loop system is modular; it requires an insulin pump, a continuous glucose monitoring sensor and a control algorithm. These components, working together, create a biofeedback mechanism, similar to that of a functioning pancreatic beta-cell. The safety and efficacy of such systems have been investigated by the APCam consortium, in a study conducted in both adults and children (although only overnight in the paediatric population), and in a real-world, home setting (Thabit et al, 2015). The results were impressive, with an 11–24% increase in time spent in the target glycaemic range compared with controls using sensor-augmented pump therapy. This has been replicated with other closed-loop systems using different control algorithms, with a meta-analysis showing a mean increase in time in range of >11% across all reviewed studies (Bekiari et al, 2018). This study included both research-only devices and those which are now commercially available.
Closed-loop systems have been proven to be both safe and effective. Does this render insulin pumps, and as such this clinical review, moot? In the current state of the art, the insulin pump forms a hugely significant part of the closed-loop “trifecta”. It could be argued that pump therapy would form a very important step in the transition to closed-loop systems for users. This should be explored further in future research.
Lessons should also be learned from how insulin pump therapy has been introduced, and how this may have been a factor in the lack of significant clinical impact observed. Research needs to be undertaken about how healthcare professionals train patients and their families, and about what level of support these patients need during the transition to pump therapy, as well as which patients would benefit most from this technology, and when in their journey with diabetes. Careful, coordinated planning of this translational research will ensure that this developing technology is used effectively in real-world settings.
Conclusion
In conclusion, the evidence for the use of insulin pumps in children and young people has been mixed, especially when using improvements in glycaemic control as the primary outcome measure. Improvements in quality of life, especially in the important context of the family, have been more consistent. That said, if this was a pharmacological therapy, would we be happy using it based on the available evidence? If insulin pump therapy alone was the pinnacle of diabetes technology, it would present a challenge to defend its routine use. However, as a significant part of closed-loop systems, insulin pumps will continue to factor in diabetes therapy for the foreseeable future. More research needs to be undertaken to discover what part, if any, conventional insulin pump therapy has in this exciting era of closed-loop systems.




Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025