Poorly controlled type 2 diabetes can have a significant impact on foot health, with complications such as foot ulcers and amputation (Kerr et al, 2014; Lazzarini et al, 2018). The incidence of type 2 diabetes is steadily increasing, with significant implications for NHS sustainability (Public Health England, 2016).
Glycaemia can increase the risk of complications such as loss of protective sensation (LOPS; Mishra et al, 2017) and peripheral arterial disease (PAD; Stratton et al, 2000). These are key risk factors in the development of diabetic foot ulcers and amputation (Stratton et al, 2000). Furthermore, there is potential for those at low risk to become at increased risk over time (Mcinnes et al, 2011; Hill, 2019); therefore, prevention strategies are a public health priority (Bus et al, 2020).
Several studies have demonstrated that people at low risk are less likely to practice good foot self-care than high-risk individuals (Pollock et al, 2014; Matricciani and Jones, 2015), and are more likely to engage in damaging behaviours (Hill, 2019). Therefore, there is a need to further understand why feet matter (or do not matter) in the eyes of those at lower risk who have type 2 diabetes, in order to inform preventative initiatives.
Study methods
Ethical approval
Ethical approval for this qualitative study was granted as an amendment to an existing research initiative (HSR1819-030) from the University of Salford.
Participants
All participants had been diagnosed with type 2 diabetes, were currently at lower risk of developing foot health problems and were routine footcare patients of the University of Salford podiatry clinic. Seventeen potential participants (nine male, eight female) due to attend clinic were invited to participate in semi-structured, face-to-face interviews. Nine participants (five female and four male) agreed and provided written, informed consent. The interviews were conducted by a student podiatrist (EB) supervised by the first author (SS).
Data collection
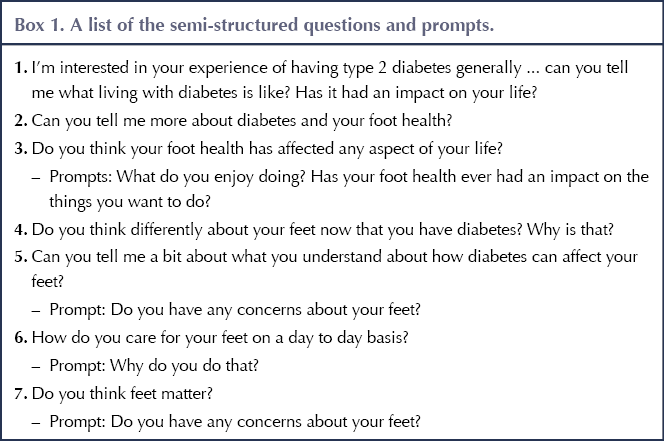
Semi-structured questions were used to elicit the beliefs, experience and understanding of type 2 diabetes-related perspectives about foot health. The semi-structured interviews included open-ended questions, partially driven by responses from the participant, but were guided by the questions in Box 1.
Data analysis
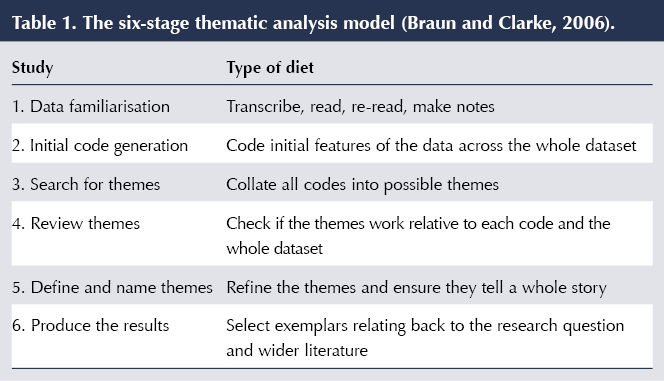
Themes were identified using thematic analysis (Table 1), which helps to ensure the production of high-quality, rich datasets, and is deemed suitable for a novice researcher (Clarke and Braun, 2017). The data were scrutinised by two experienced researchers (AW and SS). Field notes were taken after each interview. Interviews were externally transcribed and compared with the audio files for accuracy before analysis.
Results
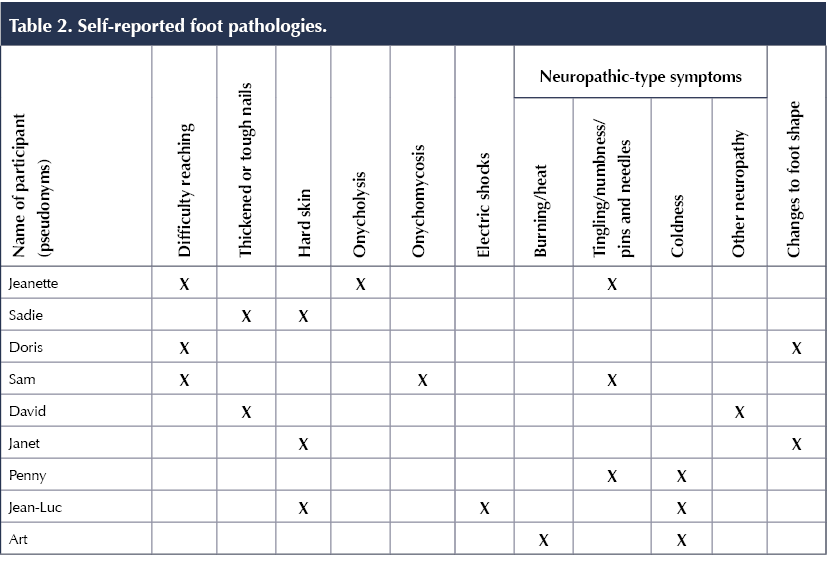
Nine participants (five female, four male) aged between 43 and 80 years were interviewed. Six participants had experience of non-diabetes-related comorbidities, including cancer, COPD and depression. The results aligned with the biopsychosocial model of health (Engel, 1977), whereby the pathophysiological presentation of each participant gave the biological context, and two overarching themes were identified; theme 1: psychological impact and theme 2: social impact. There was variation in the experiences and beliefs of the participants within each theme.
All participants described a range of foot health pathologies that may or may not be directly related to their diabetes status (Table 2). This provides context and is an important feature of the research, given that participants did not always perceive a link between diabetes and related foot health problems. Even symptoms related to neuropathy that are clearly understood to be sequelae of type 2 diabetes disease progression were not always confidently or accurately related to diabetes.
Theme 1: Psychological impact
Several participants indicated confusion and a lack of understanding about how diabetes can affect feet, resulting in a fear for the future.
Subtheme 1: Uncertainty about “why feet matter” in the context of type 2 diabetes
Several participants were uncertain how diabetes can affect foot health, and any awareness tended to be superficial. While some participants were aware of neuropathy, there was some confusion about any connection between neurological and vascular consequences of diabetes:
“Nerve damage can cause the numbness. I suppose it can affect circulation as well. I don’t know whether the nerve damage and circulation are all kind of linked.” (Jeanette*)
*For the purposes of this article, all names used are pseudonyms.
Only one participant demonstrated knowledge of a link between gangrene and ulceration, but he questioned his understanding, stating:
“There’s less circulation in the feet … as you get older as well, you need to be careful because of the risk of ulcers. The ulcers then turn to gangrene. Is that right?” (Art)
Most participants were aware of amputation risk but lacked clarity about how this occurs:
“When I see people and they’ve got ulcers, I tend to think that’s probably hygiene, but it’s not is it, because it’s something that happens to your body, like deterioration, isn’t it?” (Doris)
While participants were also aware of common foot pathologies, there was little connection made between type 2 diabetes and foot health. Some participants attributed their symptoms to other causes, such as old age, pronated feet or footwear. Conversely, one participant blamed type 2 diabetes for his nails growing “funny” and for fungal nail infections, but he did not demonstrate any understanding of wider complications. This problem was exemplified in participants with comorbidities. One participant had received a cancer and diabetes diagnosis concomitantly, and while she believed her physical symptoms could be linked to diabetes, she was not confident, saying:
“I know it’s sort of linked with diabetes, but it seemed to come on with the cancer treatment. So I don’t know whether it may be the steroids messing with my blood sugar.” (Jeanette)
There was also a sense of not “being at that stage” where proactive foot care is warranted. Jeanette talked about keeping a check on her “little bit of numbness” and stated:
“I forget I have diabetes until something crops up that reminds me. [Feet are] something that you don’t really think about, you take for granted until suddenly you can’t use them.” (Jeanette)
For other participants, however, having diabetes has led to an increased consciousness:
“I think with being diabetic makes you more conscious of [changes to the body].” (Sadie)
Subtheme 2: Impact of foot symptoms and concerns
The impact on mobility and how problems were overcome were described by some participants. Jean-Luc shared how he manages pain when walking:
“I have to stop and scrunch up my feet. If no one’s around, [I] take my shoe off to massage my foot.” (Jean-Luc)
Knowing what to look for and how to care for feet empowered some participants:
“It doesn’t worry me because I think I’ve got it under control. I’ve got better sensation in my feet now. I’m not as worried as I could be.” (Art)
One described fear associated with possible amputation:
“Scared! I don’t want to lose a toe.” (Sam)
Some participants described the psychological impact of physical restrictions:
“It breaks my heart. I used to go swimming, dancing, walking, cycling. I could still do a bit of it, but I’d suffer with the feet afterwards.” (Penny)
“I used to walk four and a half miles. I mean it’s not a marathon, but I enjoyed that. I couldn’t do it now.” (David)
Foot problems and limited footwear choices also had an emotional impact:
“I can only wear one pair. I was really getting to the end of my tether.” (Doris)
“I don’t feel I fit in with them (friends). I want to wear heels. It’s stopped me from going out and dancing. I started crying. I felt so depressed.” (Penny)
There can also be an emotional impact associated with a lack of understanding:
“[I’m] an idiot. It was burning my skin. Why was it not hurting me? If you’re burning flesh, it’s going to stink and I had none of that. And yet when they cut my nails, if they touch me in the wrong way, I can feel it. I just can’t work it out.” (Sam)
Subtheme 3: adjusted behaviours and self-management
Participants employed several problem-solving strategies, with David describing how he stays active:
“I park as far away as I can and try and walk around the car park three times. It’s not an easy feat, but I do it. I’d be absolutely lost if I couldn’t walk at all.” (David)
Jeanette described how she wears different heel heights around the house to increase tolerance:
“I probably need to change my footwear instead of just wearing trainers all the time so that my feet are constantly used to different heel heights and fastenings.” (Jeanette)
Sam also revealed damaging behaviour to resolve his cold feet:
“I had this dressing gown [which] had slots for your feet and it still wasn’t working. I had these medicine bottle things and I put warm water in. I didn’t know they were burning my feet … I couldn’t feel it.” (Sam)
Understanding the importance of basic regular hygiene was also lacking, although Sadie could provide a rationale: “…because [my feet] can crack so I’m careful.”
Some participants related the importance of self-care in relation to neuropathy:
“At night, I’ll soak them in warm water; not hot, warm. I don’t want to burn my feet again, plus I don’t feel it anyway.” (Sam)
Sam also talked about the fact that he would not walk around barefoot, “because if I trod on something, I probably wouldn’t feel it.”
Subtheme 4: Why feet DO matter
There was universal agreement that feet matter. However, this was not always implicit in the wider data. When asked why feet matter, most participants indicated maintaining mobility, but the reasons for wanting to stay mobile differed widely.
For Jeanette, walking is a way of staying active after cancer treatment. Doris also relates the importance of walking:
“I just want to keep walking and that’s what keeps me going.” (Doris)
Independence and capacity to care for others were also considerations:
“There’s so much you can do if you look after your feet. I want to be able to rely on myself; without feet, you struggle.” (Sadie)
Theme 2: Social issues
All participants chose to attend a student podiatry clinic, perceiving that NHS appointments were not frequent or long enough to meet their needs, or they found it hard to reach their own feet to cut toenails, etc. The nature of the service also presented an issue for some participants.
Subtheme 1: Lack of information
Several participants expressed a knowledge gap in relation to type 2 diabetes:
“I don’t think I’ve ever sat down and talked about my diabetes. I’ve been to my GP – they never said there’s such thing as a diabetic doctor or nurse. I’m trying to do it myself.” (Sam)
“It feels like you’re just a number. You’re just done, gone, you’re out the door. They don’t want to listen to you. If you ask them, you’ll have to make a longer appointment. You think, it’s not right, this.” (Penny)
Some participants expressed the importance of information to decision-making and self-care. Sam described how he wants to understand his condition:
“I want to know the ins and outs, and try and deal with it. The more info you get, the better, then you can work it out yourself can’t you? You’ll find ways of doing things that suit you.” (Sam)
He continues to link how knowledge can impact on self-care:
“I was told never to cut your own nails in case it bleeds. It’s serious because you’ve got no feeling. Now I understand.” (Sam)
Subtheme 2: Disconnected therapeutic alliance with healthcare professionals
Some participants described a disconnect between advice and experience. For example, although wearing socks may be recommended for cold feet, some participants felt this made their feet feel worse because “it holds the cold in.”
David described how he had been “told off”, adding: “I only occasionally dry between my toes. I get told off about that at the clinic.”
Meanwhile, Doris explained that: “when I was first diagnosed, where this toe was rubbing, I’d washed it and put a plaster on. She went mad and said no, you mustn’t do that, you must come to the outpatients.” The effect of this did not create positive behaviour change.
Penny talked about her struggles with neuropathic symptoms, describing the discord between her experience and a nurse’s perception:
“She said ‘oh it’s not too bad’ but it is, I feel it.” (Penny)
In contrast, Art described the impact of a positive therapeutic alliance:
“Since I had diabetes, I attend a doctors surgery where the doctor is a trainee. He’s been very, very good – he’s rung me up [and said] ‘can you do a quick test now for me, just tell me what the figures are’ and we’ve worked together to bring my diabetes under control. So now it’s practically normal.” (Art)
Subtheme 3: Patient beliefs trump advice
Several participants talked about complying with advice, yet gave several examples where they had not, sometimes because of a conflict with belief systems. This demonstrates the complex interplay between beliefs, actions and advice. It also highlights why understanding beliefs is key, echoing findings by Gale et al (2008) and Johnson et al (2005). Doris stated:
“I do do what I’m told … my feet are always dry … they’ve suggested all sorts to me about putting cream in a plastic bag. And I’m thinking, ‘If that works, I will do that.’” (Doris)
However, on probing, she revealed she had not, “because I was trying to work it out and I thought, ‘Now, do you go to bed with that on … then I’m thinking about what happens in the morning, or are you sliding?’” Similarly, Art weighed the perceived risks to benefits: “Going for a slide … that’s more of a danger than having dry feet.” He also revealed expense as another barrier: “The specialist cream with the urea in is quite expensive for normal people.”
Subtheme 4: Family and social support
Sam and Penny both talked about their relationships with family. Penny described feeling alone:
“It’s the shock of having it. My parents didn’t have it and I can’t think of anybody else in the family that has had it. I never talk about it to my children; it does get to me.” (Penny)
Sam attributed being overweight as the cause of his brother’s diabetes, but was confused at his own diagnosis:
“They reckon it’s all fat guys that get it. I’m not fat. I was eight and a half stone when I got diagnosed – how do you work that out?” (Sam)
He also described how their self-management differs and observed that he does not feel his brother “cares much”. When asked if he talks to his brother about diabetes, Sam replied: “I don’t think he likes talking about it.”
Discussion
This study has revealed how people with type 2 diabetes express behaviours and beliefs about if and why feet matter. Some of the symptoms described are related to common foot pathologies associated with diabetes, such as dry skin and callus (De Macedo et al, 2016; Schaper et al, 2020) and some nail disorders (Cervantes et al, 2017). There were also diabetes-related changes to foot shape (Cheuy et al, 2015; Tang et al, 2015) and peripheral neuropathy (Tesfaye and Selvarajah, 2012; Pop-Busui et al, 2016). However, these results highlight that, while participants are aware of their foot pathologies, they do not always link them to type 2 diabetes or relate them to the importance of foot self-care.
The biopsychosocial model recognises ways in which people experience and respond to physical, psychological and social aspects of their condition (Engel, 1977; Borrell-Carrio, 2004; Smith et al, 2013), and this was borne out by the present results, in which participants demonstrated how beliefs can influence behaviour. This reinforces the need for person-centred foot healthcare, and timely information that is responsive to knowledge levels, capacity and motivation.
Engel (1977) recognised that psychological and social factors can influence when individuals (and those around them) identify as being ill. In this study, participants who had minimal complications demonstrated a lack of concern about foot health. This suggests that prevention of foot pathology is not a key consideration and the potential sequelae are not apparent. The presence of comorbidities or confounding factors, such as ageing, were also prevalent, where some participants blamed old age or other comorbidities for foot health problems and did not relate them to type 2 diabetes. This indicates the lack of knowledge and understanding about the wider implications of type 2 diabetes on foot health.
The study also provides insight into experiences of living with non-painful neuropathy, a phenomenon that is predominantly absent from the literature. For example, Brod et al (2015) describe a range of peripheral neuropathy symptoms, but “cold” is not listed. This suggests value in conducting further research into the effect of diabetic peripheral neuropathy on the lives of people who experience debilitating symptoms without pain. Furthermore, there was a real difference in participants’ social, emotional and physical experience of the same symptoms related to peripheral neuropathy. This supports taking a biopsychosocial, person-centred care approach (Borrell-Carrio, 2004).
The therapeutic alliance was important in relation to foot health information; while some participants would follow foot health advice even if they did not perceive a direct benefit, others would prioritise their own beliefs where there was incongruity. This exemplifies the importance of aligning management strategies with personal beliefs, needs and capacity.
Several female participants reported the impact of limited footwear choices on their social life and psychological wellbeing. Some participants revealed strategic concordance, whereby health advice was negotiated in specific instances so that a person could continue to wear a desired pair of shoes. This reinforces the link identified by Farndon et al (2016) between footwear and identity. It also supports the proposal made by Nicholls et al (2018) that there could be a benefit to linking a sociological approach to podiatry consultations in order to further relate to patients and their needs.
Consistent with other studies of people with type 2 diabetes at lower risk of foot health problems (Burnside et al, 2007; Gale et al, 2008; Searle et al, 2008), several participants could not provide examples of how type 2 diabetes can affect feet, and this demonstrated a lack of understanding of the potential disease sequelae that can lead to ulceration (Searle et al, 2008). This was also the case for lower-level foot pathologies such as callus, fungal nail infection, nail thickening and changes to their foot shape. This has direct implications for motivation to prioritise preventative foot self-care management.
The insidiousness of type 2 diabetes onset is noted in the literature (Mcinnes et al, 2011). Minimal symptoms can lead to complacency toward potential complications such as diabetic foot ulceration (Burnside et al, 2007). This reactivity to foot health in relation to type 2 diabetes was demonstrated throughout the results, and the effect materialised when symptoms began to have a tangible impact.
If knowledge is considered an enabler of foot self-care (Matricciani and Jones, 2015), it follows that a lack of understanding can lead to an absence of efficacious foot health behaviour. This is borne out in the findings by Gale et al (2008) and echoed in this study, with several participants providing similar examples of behaviour that put foot health at risk. This suggests a lack of appropriate and timely patient education, particularly in the early stages.
Healthcare systems and professionals are a key component of the “social” aspect of the biopsychosocial model (Bolton, 2019). Engel (1977) proposes that “rational” therapy alone is not enough, and that the physician–patient relationship could directly affect outcomes. Some participants experienced confrontational clinical encounters, none of which had a successful outcome, reinforcing the need for person-centred care founded on a positive, empathic therapeutic alliance.
The power of language to educate and build confidence is highlighted in the Language Matters guide produced by NHS England (2018). Conversely, negative communication can lead to feelings of shame or blame, and undermine self-care activities (Borrell-Carrio, 2004; NHS England, 2018). This suggests clear implications for developing communication skills and empathy in practice.
Participants sometimes described themselves as passive agents, suggesting a traditional paternalistic professional–patient relationship (Flocke et al, 2002). These findings demonstrate how influencing behaviour is complex and that advice is not always impactful when personal belief systems are not congruent with it. This reinforces research by Johnson et al (2005) and Gale et al (2008), who found that behaviour is linked to beliefs and understanding.
Finally, there was a sense of frustration from several participants about the level of information provided. Yet guidance is clear about the benefits of this to empowerment and quality of care, especially since providing healthcare information encourages proactive health behaviour (Health and Care Professions Council, 2013; NICE, 2015), where the importance of providing information to facilitate shared decision-making is recognised (Coulter and Collins, 2011).
All participants chose to attend a university podiatry clinic. This suggests some motivation to care for foot health. However, in spite of this, participants described limited self-directed foot behaviour, which reflects findings from other studies into foot self-care behaviours in lower-risk individuals (Pollock et al, 2004; Gale et al, 2008). This may be because of physical limitations (Matricciani and Jones, 2015), as well as the perceived importance, attitudes and beliefs that influence self-care. Several participants revealed that where they saw a benefit they were more likely to act, but a lack of perceived benefit can hinder engagement. This lends credence to research findings by Matricciani and Jones (2015), who state the role of individual beliefs and attitudes in relation to barriers and facilitators of self-care. These findings also support the findings of Gale et al (2008), who recommended that healthcare professionals explore beliefs, motivations and understanding to address any misconceptions or gaps in knowledge.
In relation to the question “Do feet matter?”, most individuals referred to perceptions about their future foot health, rather than current foot problems. There was also a disconnect between beliefs and actions, whereby although feet were declared to matter, they were also forgettable in the absence of poor foot health. Yet the reasons for the importance of good foot health were evident in relation to independence, mobility, function and ability to care for others. This potentially highlights the benefit of engaging with the motivation to keep feet healthy, and is consistent with adopting a motivational interviewing technique (Rollnick et al, 2010).
Study limitations and recommendations for future research
This was an exploratory study and several themes emerged that were not initially anticipated, such as the therapeutic alliance and its significance; therefore, this is a recommendation for future work. The researcher carrying out the interviews was inexperienced in qualitative research; however, the process was guided by mentorship from experienced co-authors. As previously discussed, the participants all chose to attend a university podiatry clinic and, therefore, the findings will reflect this.
Conclusion
This study reveals the experiences of individuals with type 2 diabetes at low risk of foot health problems, the impact on quality of life and attitudes toward foot health self-care. The findings demonstrate the variety of ways in which people consider the psychological and social impact of diminished foot health, and yet, through a lack of knowledge or incongruity with personal belief systems, there was little motivation to proactively manage foot health to improve current health or prevent future problems. The results exemplify the need to gain insight into an individual’s biopsychosocial world to provide patient-centred care and improve outcomes.
Acknowledgements
The authors would like to thank all participants who willingly took part in the study, as well as staff at the University of Salford podiatry clinic for facilitating the recruitment and interviewing process.
Publisher’s note
This article was originally published in The Diabetic Foot Journal and has been adapted for the Journal of Diabetes Nursing. To read the original article, click here.





Empowering nurses to tackle inequities in access to technology.
22 Jul 2025