Over the last few decades, key stakeholders have worked tirelessly to raise awareness of the need for diabetes inpatient services, given that hospital bed occupancy by people with diabetes remains stable at around 20% (Diabetes UK, 2017; NHS Digital, 2020). However, almost one fifth (18%) of hospital sites in the UK still have no dedicated diabetes inpatient specialist nurse (DISN), according to the 2019 National Inpatient Diabetes Audit (NHS Digital, 2020).
In 2020, with the surge in COVID-19 infections, healthcare systems experienced increased demand for inpatient care (McCabe et al, 2020). As a result, many healthcare workers, including DISNs, were redeployed to work on general wards, as part of the NHS plan to address staffing issues and the unprecedented wave of hospitalised patients with COVID-19 (Rayman et al, 2020). This further stifled the delivery of care for inpatients with diabetes, who were also disproportionately affected by COVID-19 (Holman et al, 2020).
An online survey of 1829 diabetes nurses undertaken by the Foundation of European Nurses in Diabetes revealed substantial interruption in clinical diabetes services (Forde et al, 2021). Anecdotal evidence suggested that, in the UK, most diabetes nurses were redeployed, leaving only a few diabetes nurses to care for inpatients.
Several studies have reported the physical and mental health effects of the COVID-19 pandemic on healthcare professionals. This includes the worry about dealing with a highly infectious virus (Wu et al, 2020), wearing of personal protective equipment (Vindrola-Padros et al, 2020), anxiety about working in unfamiliar settings (Sykes and Pandit, 2021), rapidly changing clinical protocols and guidelines (Maben and Bridges, 2020), and redeployment due to staff shortages (Vindrola-Padros et al, 2020). In addition to these, the limited number of DISNs working in diabetes were at an increased risk of stress due to growth in demand secondary to the glycaemic complications of COVID-19 (Rubino et al, 2020).
The impact of the COVID-19 pandemic on DISNs in the UK is not well documented. For example, it is not known what proportion of DISNs in the UK were redeployed during the pandemic, and the possible implications of this on inpatient diabetes care are not well understood. It is also not clear whether, or the extent to which, DISN wellbeing was supported during the COVID-19 pandemic. This is important in identifying gaps in staffing and staff wellbeing, in order to develop appropriate resources and services. Our study aim, therefore, was to explore the impact of COVID-19, and associated redeployment, on diabetes inpatient specialist nurse services in the UK.
Methodology
The DISN UK Group, in collaboration with Diabetes UK, developed two set of questionnaires to understand the impact of the pandemic on diabetes inpatient services and specialist nurses during both the first and the second COVID-19 waves.
In the first survey by the DISN UK Group, a Freedom of Information (FOI) request was emailed to 229 NHS Trusts across the UK in April 2021. As this was an FOI request, we did not require an ethical review board regulation. FOI requests have existing structures in place that satisfy ethical values and considerations (Walby and Luscombe, 2018). The following information was asked:
- The number of dedicated DISNs (including whole time equivalents [WTE; a division of the number of required hours for a role by the fullt-time equivalent of 37.5 hours per week]).
- Whether COVID-19 risk assessments were available.
- Redeployment during the first and second waves of the pandemic.
- The referral and support available for the mental health and wellbeing of DISNs.
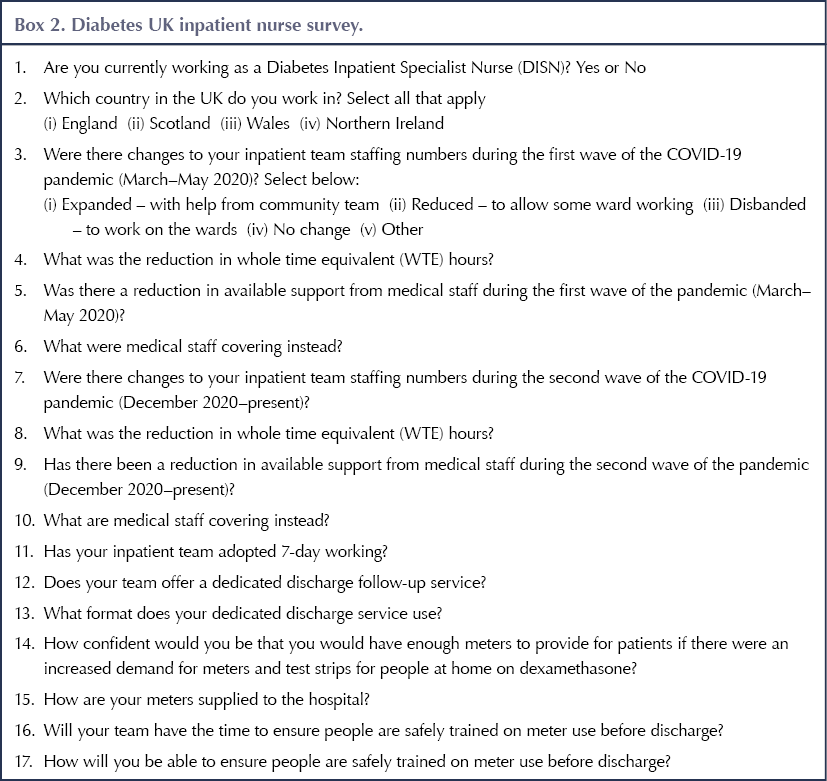
Concurrently, Diabetes UK conducted a short, online, open-access survey for DISNs in the UK via social media to gain insight into the following:
- The impact of the pandemic on DISN staffing numbers.
- Available medical team support during the first and second COVID-19 waves.
- Available dedicated discharge services for patients.
- The provision of blood glucose meters for patients, especially those managed on steroid therapy.
These two questionnaires are detailed in Box 1 and Box 2.
Participants’ responses were exported into Microsoft Excel and analysed using descriptive statistics, and grouped into the following categories: dedicated DISN workforce and risk assessment; redeployment of DISNs; and access to mental health and wellbeing support.
Results
FOI survey report
Of the 229 FOI requests sent, only 41 respondents provided answers to the information requested. The others that responded were commissioning groups, which did not hold the relevant information required.
Dedicated DISN workforce and risk assessment
Thirty-six of 41 Trusts had dedicated DISN(s), and all of these staff were assessed to minimise potential risk to themselves and patients. One Trust had a new staff member who was yet to be risk-assessed.
The total DISN WTE provided by these Trusts was 147.6, but the range was vast: between 1.0 and 11.8 WTE. Of the Trusts which did not have a dedicated DISN, diabetes inpatient services were shared among the diabetes specialist nurse (DSN) rota (n=3) or provided by DISNs from another Trust (n=1). Only one Trust declined to respond to this question due to confidentiality reasons.
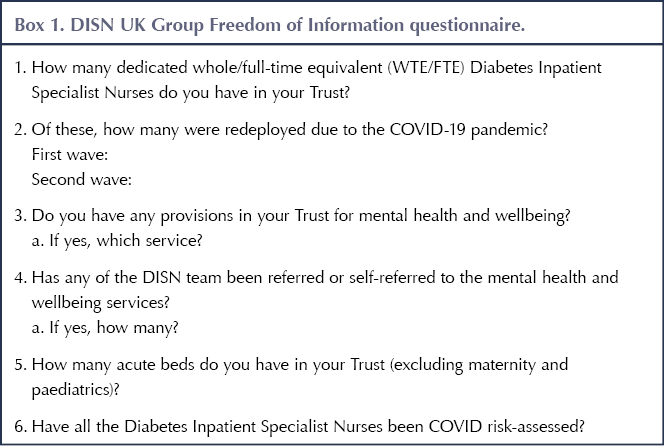
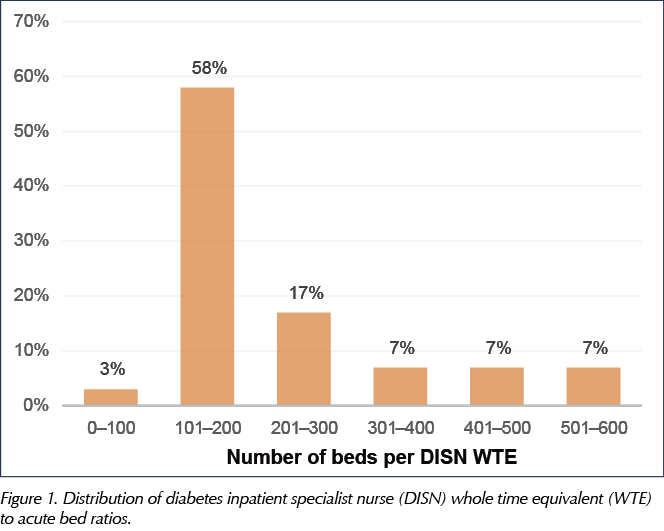
Within those Trusts with a dedicated DISN, the DISN-to-bed ratio (i.e. the number of acute beds attended by one DISN WTE) ranged from 1:82 to 1:600, demonstrating significant differences in potential workload. Six Trusts had one DISN for more than 300 beds and two of these had one DISN for more than 500 beds. The distribution of DISN-to-bed ratios is shown in Figure 1.
Redeployment during COVID-19
Eighteen Trusts (50%) redeployed DISN staff (0.2–5.0 WTE) during the first wave of the pandemic (March to May 2020), while the remaining 18 did not redeploy any DISN. Of those that redeployed DISNs, this was equivalent to a total of 33.7 WTE, with one Trust redeploying all its staff.
During the second COVID-19 wave (December 2020 to May 2021), 11 Trusts redeployed a total of 19.9 DISN WTE (including two Trusts that redeployed all their DISNs), but the majority (n=26; 70%) did not redeploy any staff. Eight Trusts redeployed DISNs during both waves; nine redeployed during the first wave only; four redeployed during the second wave only; and 14 did not redeploy any DISNs during either wave.
Mental health and wellbeing services available for DISNs during COVID-19
All of the 41 Trusts except one, which did not share its information, reported having provisions for staff to access mental health and wellbeing services. Identified services included Employee Assistance Programmes (EAPs); Mental Health First Aid; Trust counselling and psychology services; wellbeing webinars; Vivup (an employee benefits provider specialising in health and wellbeing), Health Assured, Care First; and access to mindfulness and meditation, such as yoga, Reiki, etc.
We enquired whether DISNs were signposted to mental and wellbeing services at their workplaces during the pandemic. Only seven Trusts responded that their DISNs were referred to access available mental health and wellbeing services; the majority did not disclose this information on the grounds of confidentiality.
Diabetes UK questionnaire results
There were 26 respondents to the Diabetes UK questionnaire, of whom 24 were DISNs and two were excluded as they appeared to be duplicates from the same Trust. The majority (88%, n=21) were from England, 8% (n=2) were from Scotland and 4% (n=1) were from Wales and none from Northern Ireland.
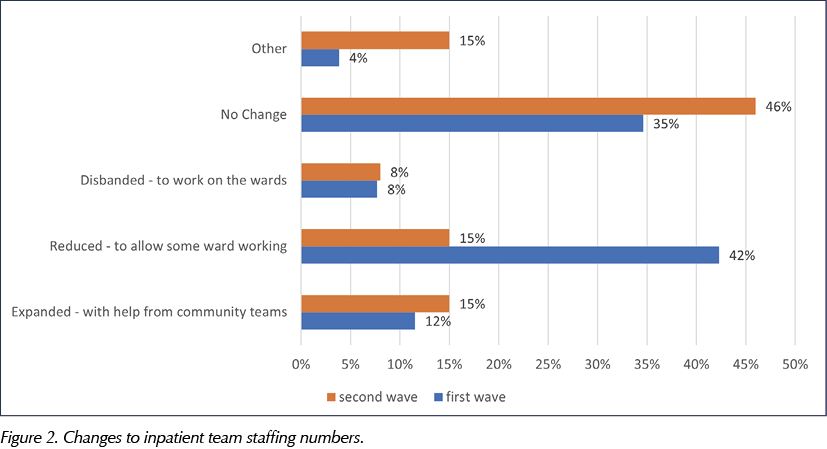
Changes to inpatient staffing levels, reduction in WTE and adoption of seven-day working schedule
The survey responses concerning changes to inpatient staffing numbers are summarised in Figure 2. It shows twice as many inpatient team members (50%; n=13) were reduced and disbanded to work on the wards during the first wave of COVID-19 than in the second wave (23%; n=6). Nearly half of the respondents (46%; n=12) reported no changes to their staffing numbers during the second COVID-19 surge as compared to the first surge. The inpatient teams were expanded with support from community teams during both waves, which may have impacted on community diabetes service provision.
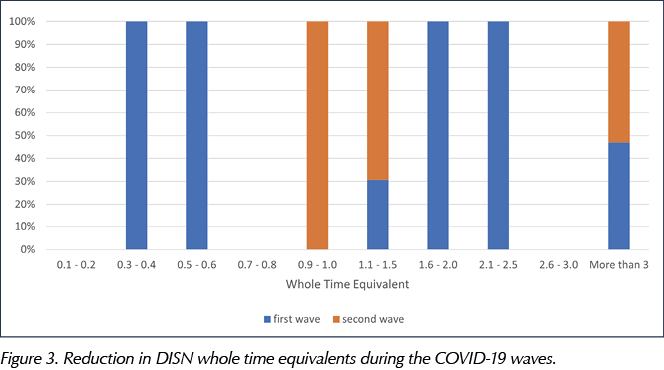
The reduction in WTE (range from 0.1 to more than 3.0 WTE) occurred more frequently during the first wave than the second wave, as reported in Figure 3.
Additionally, the survey asked how many of the inpatient teams operated a seven-day working schedule during the pandemic. Prior to the start of the COVID-19 outbreak, before March 2020, seven (27%) of the 26 responding inpatient teams operated a seven-day plan. During the first COVID-19 wave, only five respondents (19%) adopted a 7-day working schedule, and this number increased to eight (31%) during the second wave.
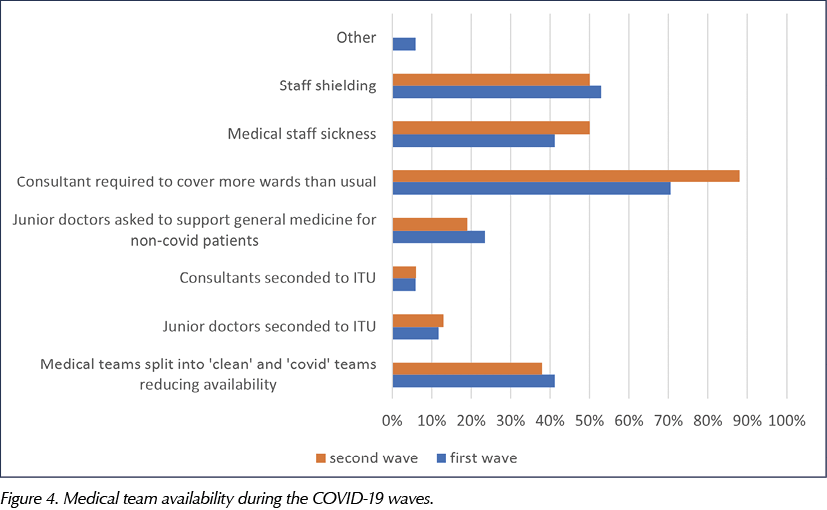
Reduction in medical support
The inpatient team reported a roughly 60% reduction in available medical support during both COVID-19 waves. Half of the medics were not available due to sickness or staff shielding. Most of the consultants (80% on average) were sent to cover general medical wards, and just under 20% of both junior doctors and consultants were seconded to intensive care units. A few of the junior doctors were also asked to support general wards. Figure 4 compares medical staff coverage in both the first and the second COVID-19 waves.
Dedicated discharge services
Approximately 60% (n=16) of the inpatient teams reported having a dedicated discharge follow-up service, while the remaining 40% (n=10) had none. All of the inpatient teams who responded (n=16) offer telephone follow-up appointments, and almost half (44%; n=7) provide face-to-face follow-up as well. Generally, 25% of the participants (n=4) deliver follow-up via remote formats.
The Diabetes UK survey also looked at the availability and supplies of blood glucose meters to hospital and to people on dexamethasone at home, and whether staff were confident they could train patients safely before discharge. Details of the responses are in Table 1.
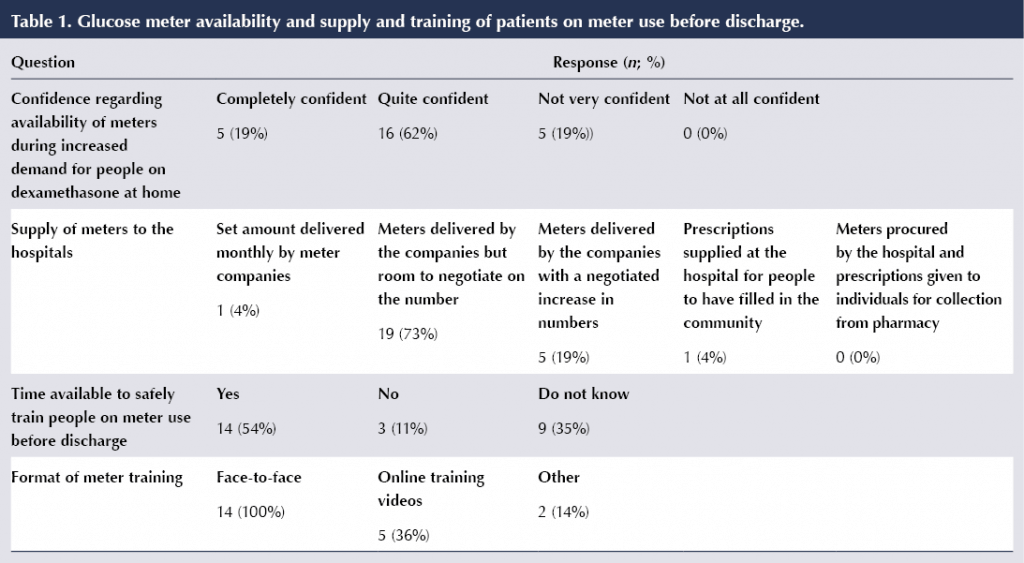
Most hospitals receive and negotiate the number of meters needed directly from the companies that produce them, and none are procured by the hospitals themselves. In times of increasing demand, especially for people on dexamethasone at home, over 80% of the inpatient teams felt confident that enough meters would be available; however, only 50% felt they would have time to safely train patients before discharge. The training was mostly conducted face-to-face, but around a third of respondents (35%) reported using online training videos for their patients.
Discussion
These surveys have provided insight into the impact of the COVID-19 pandemic on diabetes inpatient specialist services in the UK. Although the number of participants is relatively small, the study results have highlighted the changes to diabetes inpatient specialist teams’ staffing numbers and a reduction of dedicated DISN hours during both COVID-19 waves in the UK. Some Trusts in the UK do not have a dedicated DISN team but they usually share the work among their DSN rota. The Joint British Diabetes Societies for Inpatient Care (2019) have stressed the worrying shortage of DISNs in the UK, which accounts for why about 30% of inpatients with diabetes are not reviewed by a dedicated DISN team.
Our findings are in line with the National Diabetes Inpatient Audit in 2019, which reported that a sixth of hospitals still have no DISNs, though the number of DISN hours per patient had gradually improved since the years 2015 and 2017 (NHS Digital, 2020). There is a need for more dedicated inpatient specialist teams to match up the number of beds occupied by people with diabetes in the hospital to promote good inpatient outcomes. This has been further highlighted by the NHS Long Term Plan, which states that hospitals should offer expanded access to diabetes inpatient specialist nursing teams to reduce inpatients’ length of stay, enhance recovery and prevent potential readmissions (NHS, 2019).
During the COVID-19 waves, redeployment of healthcare professionals was used as an approach to address shortages and capacity concerns (Vindrola-Padros et al, 2020). Our study showed that many Trusts both redeployed their DISNs and had severely reduced medical support during the pandemic, especially during the first wave. The National Diabetes Inpatient COVID-19 Response Group, created in the last week of March 2020, reported similar findings in one of its Diabetes UK position statements (Rayman et al, 2020). It remarked that most diabetes teams, including inpatient specialist nurses, were redeployed to support general ward care.
Redeployment and disruption in clinical diabetes services further impacted on the care that inpatients with diabetes required during the pandemic, which relates to the findings of the pan-European survey of diabetes specialist nurses undertaken by the Foundation of European Nurses in Diabetes COVID-19 consortium (Forde et al, 2021).
COVID-19 infection has been associated with increased risk of new-onset diabetes (Rubino et al, 2020) and increased hyperglycaemic episodes from severe infection (Li et al, 2020). In addition, most studies have reported that people with diabetes are at increased risk of severe COVID-related infection and mortality (Bornstein et al, 2020; Holman et al, 2020). In people admitted with COVID-19, the use of dexamethasone has been accepted as a possible treatment for the coronavirus infection. The RECOVERY trial demonstrated that once-daily dexamethasone 6 mg reduces mortality in patients with COVID-19 who are on respiratory support (RECOVERY Collaborative Group, 2021). However, this treatment has the potential to further trigger steroid-induced hyperglycaemia, which can be difficult to manage, coupled with COVID-induced insulin resistance and impaired insulin production (Rayman et al, 2020). As a result of all these factors, more patients treated for coronavirus infection are requiring blood glucose monitoring and close follow-up, even at discharge, for hyperglycaemia management.
Some hospitals do not have dedicated discharge services for patients to influence timely and safe discharge. The NHS England launching of COVID-19 virtual ward models in 2021, as part of the response to safely discharge patients with coronavirus, can be useful to support diabetes discharge services (NHS England and NHS Improvement, 2021). Diabetes specialist teams can adapt the COVID-19 virtual wards guidance to agree on local pathways to provide follow-up diabetes care for people with diabetes to prevent further rehospitalisation (National Inpatient Diabetes COVID-19 Response Group, 2021).
The effects of the COVID-19 era on the mental health and wellbeing of all healthcare professionals have been well researched (Sykes and Pandit, 2021; Phiri et al, 2021). In our results, most Trusts had provisions for mental health and wellbeing services for their staff, but it is unclear whether people were accessing these services. It is noteworthy that individuals may require a degree of self-awareness and motivational energy to engage with these wellbeing services, if available. Diabetes inpatient teams should be encouraged to access services to support their mental health and emotional wellbeing, to cope with the stress from managing challenging cases of COVID-related diabetes pathology. The British Psychological Society (2020) also provided guidance for healthcare managers to practise visible leadership and demonstrate an effective communication strategy to support staff wellbeing during the pandemic. This guideline can be a useful resource for managers.
This study is limited by a small sample size and low response rate, as few of the NHS Trusts and DISNs responded. There is also a possibility that some people who responded to the Diabetes UK survey may have been from the same Trusts that answered the FOI request, resulting in some redundancy of data within the results.
Conclusion
The services of DISNs have become pertinent in managing the convoluted pathology of COVID-19-related diabetes. There should be provisions for staff including access to and uptake of mental health and wellbeing services to deal with work-related stress. Careful planning is needed to preserve diabetes inpatient services during future waves of COVID-19, and consideration should be given to the potential increase in diabetes service provision once COVID-19 is no longer a pandemic but remains endemic among the general population, in order to promote good care outcomes for people with diabetes and their safe discharge.
DISN UK Group committee members
Erwin Castro (Chair), Diabetes Nurse Consultant, East Sussex NHS Trust; Esther Walden, Lead Diabetes Inpatient Specialist Nurse, Norfolk and Norwich University Hospitals NHS Foundation Trust; Anne Claydon, Diabetes Nurse Consultant, Barts Health NHS Trust; Caroline Brooks, Diabetes Specialist Nurse and Diabetes Nurse Educator, Maidstone; Jo Reed, Renal Diabetes Specialist Nurse, Imperial College Healthcare NHS Trust; Debbie Stanisstreet, Diabetes Specialist Nurse, Hertfordshire Community NHS Trust.






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024