Registered nurses play a vital role in health promotion, the prevention of ill health and healthcare delivery in the current healthcare climate (Craig and Senior, 2018). They work alongside other healthcare professionals and must be accountable for their own actions, often working with uncertainly in challenging environments, as demonstrated during the current COVID-19 pandemic (Nelson et al, 2021). At the point of registration, nurses must achieve proficiencies across seven key platforms defined by the Nursing & Midwifery Council (NMC; 2018). These platforms include preventing ill health and improving safety. Elements of all platforms are related to long-term conditions, such as diabetes, which is specifically highlighted in the proficiencies document. A crucial message from the new standards is the requirement for higher educational institutes to work in partnership with practice learning partners to ensure that theory is transferred into practice, thus ensuring a rich learning experience (Leigh and Roberts, 2018). It may be argued that this has become more challenging during the pandemic. However, a disproportionate number of deaths due to COVID-19 have been reported in individuals with diabetes, particularly those with poor glycaemic control (Katulanda et al, 2020).
Diabetes is a common long-term condition affecting over 4 million people in the UK, with additionally an estimated 850000 people who are currently undiagnosed (Diabetes UK, 2022). Approximately 1 in 6 hospital beds are occupied by a person with diabetes and, worryingly, almost one third of inpatients with diabetes experience at least one medication or management error during their hospital stay (NHS Digital, 2020). The National Diabetes Inpatient Audit (NHS Digital, 2020) acknowledges the importance of education of healthcare professionals in preventing both diabetes medication and management errors, particularly considering the perceived variable level of diabetes knowledge amongst hospital staff reported by patients. These findings, along with the additional challenges of COVID-19 on diabetes management, have an impact on the provision of clinical services, both in primary and secondary care settings. Hence, ensuring that new NMC registrants have the knowledge and skills required to deliver evidence-based diabetes care is of paramount importance.
Several studies have investigated diabetes knowledge in various healthcare professions, including registered nurses and healthcare assistants, and have identified knowledge gaps in, for example, the management of hypoglycaemia and medicines management (Cardwell et al 2016; Hayes and Cardwell, 2017; Lange and Pearce, 2017). A study of 116 qualified nurses, working across a variety of specialities, reported that diabetes knowledge was significantly higher (P < 0.01) in nurses working in medical areas compared to those working in surgery, with nurses working in dermatology scoring the lowest (Abduelkarem and El-Shareif, 2013). This was particularly evident for scores relating to acute complications, such as hypoglycaemia and diabetic ketoacidosis (DKA), both of which are potentially life-threatening. This is an important finding as most hospital admissions in adults with diabetes are not directly diabetes-related, so patients will occupy beds across hospital specialties (NHS Digital, 2020). In addition, hyperglycaemia in hospital inpatients is associated with adverse clinical outcomes and increased length of stay, with a recent national audit reporting that 3.6% of hospital inpatients with type 1 diabetes developed DKA, which is preventable by careful and educated monitoring, during their admission (NHS Digital, 2020).
Deficits in diabetes knowledge do not appear to be limited to the UK. A systematic review of 25 studies across a variety of healthcare settings from developed and developing countries reported serious knowledge deficits related to diabetes medication, blood glucose monitoring and complications (Alotaibi et al, 2016). Poor diabetes knowledge amongst healthcare staff is not restricted to hospital settings; gaps in knowledge have been reported amongst staff in care homes and mental health practitioners working in a variety of different settings (Smide and Nygren, 2013; Hemingway et al, 2013). This is of concern because of the increasing number of people with diabetes living in care homes and the prevalence of diabetes in those with mental health problems (Robinson et al, 2018; Sinclair et al, 2020).
There is a paucity of information on diabetes knowledge in undergraduate nursing students. One study reported poor levels of knowledge particularly in relation to insulin therapy and general diabetes knowledge (Tawalbeh et al, 2014). Cardwell et al (2016) and Trepp et al (2010) have reported similar findings, with substantial knowledge gaps related to the management of acute clinical situations and insulin therapy.
Conversely, a study involving final-year medical students reported high knowledge scores relating to clinical management of diabetes (such as the adjustment of insulin doses and the management of hypo- and hyperglycaemia), although aspects of living with diabetes (such as dietary advice) yielded lower scores (Sagar, 2011). This may reflect the focus of undergraduate medical education compared to nurse education. Such knowledge gaps can have detrimental effects on clinical outcomes, as reported by the National Diabetes Audit (NHS Digital, 2020). Knowledge and skills gained as an undergraduate form a basis for confidence and competence. However, to influence the quality of diabetes care, evidence-based theory needs to be linked to clinical practice.
Aims
The aims of this study were to investigate diabetes knowledge in final-year nursing students, and how this knowledge is applied to common clinical situations.
Methodology
Methods
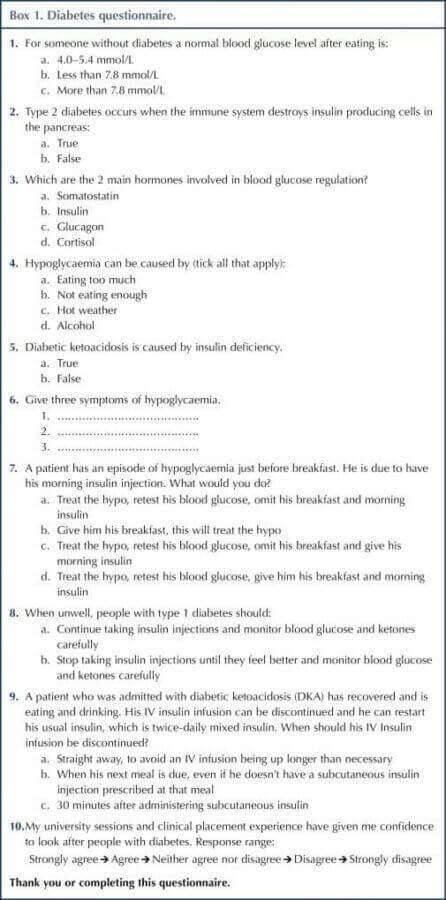
An “in-house” online questionnaire (Jisc, 2021) was used to assess knowledge related to diabetes and its application to clinical practice. The questionnaire (Box 1) was developed following a review of literature and was reviewed by clinicians currently working in the field of diabetes to maximise content validity (Polit and Beck, 2010). The questionnaire consisted of 10 questions. Nine were either multiple choice questions or elicited a “true” or “false” response, and considered two aspects of diabetes knowledge – general diabetes knowledge (5 questions) and application to clinical practice (4 questions). Higher scores indicated greater knowledge. In addition, one question required a response using a 5-point Likert scale (“Strongly agree” to “Strongly disagree”). The questionnaire utilised a variety of responses to maintain the participants’ interest.
An online questionnaire was considered suitable for this study as, at that time, teaching had moved online due to the COVID-19 pandemic.
Participants
The questionnaire was sent to a cohort of 92 final-year, adult branch, BSc Nursing students who had completed all academic modules and were soon to become new NMC registrants, thereby needing to translate theory into practice in the clinical situation.
Ethical approval
The study was approved by the ethical committee at Edge Hill University’s Centre for Learning and Teaching. Potential participants were encouraged to read the online information sheet before agreeing to take part in the study. Access to the questionnaire was not possible until electronic consent was obtained. Data collected was anonymous and participants had the right to withdraw from the study at any time.
Data analysis
Data was analysed using IBM SPSS (version 25.0) for Windows. Results are expressed as whole numbers and percentages. Questions 1–5 are knowledge-based questions and questions 6–9 focus on relating theory to practice.
Results
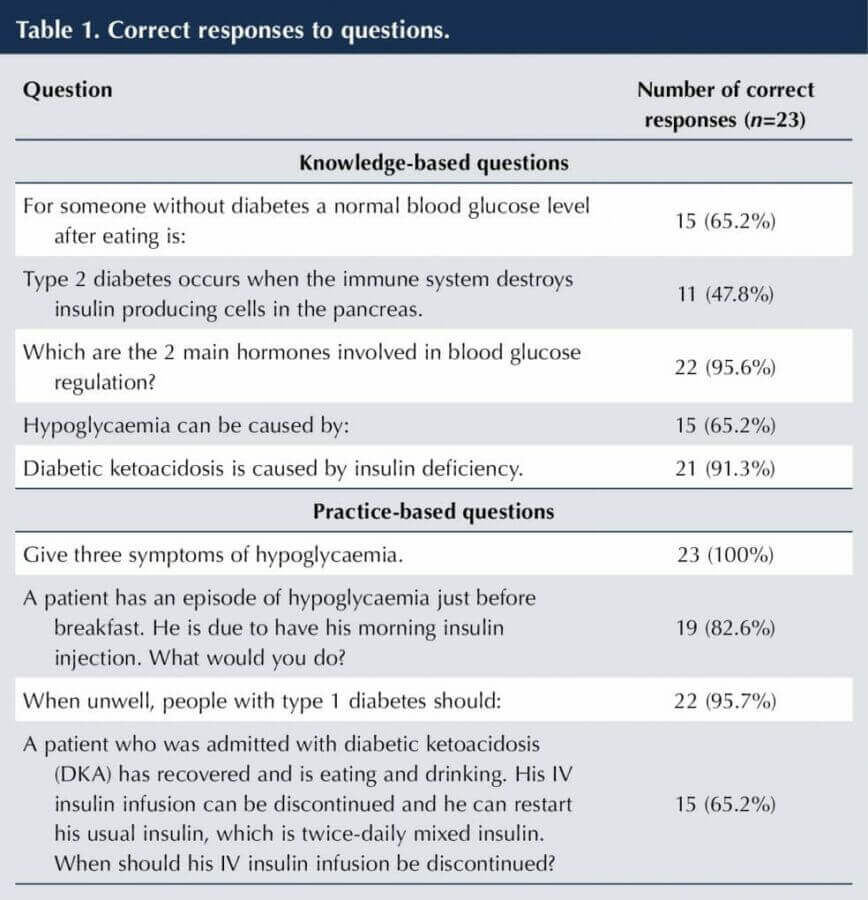
Twenty-three online questionnaires were completed, giving a 25% response rate.
Response to individual questions
Fifteen (65.2%) participants answered question 1 correctly, stating that a normal blood glucose after eating is < 7.8 mmol/L. Question 2 was answered correctly by 11 (47.8%) participants; 12 (52.2%) answered incorrectly, stating that type 2 diabetes occurs when the immune system destroys insulin-producing cells in the pancreas. Twenty-two (95.6%) participants answered question 3 correctly, identifying insulin and glucagon as the main hormones involved in blood glucose regulation. Question 4 asked participants to select all possible causes of hypoglycaemia from a list of four responses (3 correct and 1 incorrect). Fifteen (65.2%) selected all three correct answers (not eating enough, hot weather, alcohol). Twenty-one (91.3%) participants answered question 5 correctly, stating that DKA is caused by insulin deficiency. Question 6 asked participants to list three symptoms of hypoglycaemia; all 23 (100%) participants answered correctly. The most common symptoms stated were sweating (17 responses), trembling (16), confusion (7) and slurred speech (5). Question 7 was correctly answered by 19 (82.6%) participants, stating that they would treat the episode of hypoglycaemia, retest blood glucose, and give breakfast and morning insulin. Question 8 was correctly answered by 22 (95.7%) participants, stating that, when unwell, people with diabetes should continue taking insulin injections and monitor blood glucose and ketones carefully. Fifteen (65.2%) participants answered question 9 correctly, stating they would discontinue an intravenous insulin infusion 30 minutes after giving subcutaneous insulin. A summary of results is shown in Table 1.
Question 10 revealed that fifteen (65.2%) participants either strongly agreed or agreed with the statement, “My university sessions and clinical placement experience have given me confidence to look after people with diabetes.” Four (17.4%) neither agreed nor disagreed, 4 (17.4%) disagreed and none (0%) strongly disagreed.
Overall results
Results are expressed as mean ± standard deviation, percentage and range. The mean overall score was 7 ± 1.36 (77.8%; 5–9) correct answers from a possible score of 9. Five (21.7%) participants answered 5 questions correctly, 1 (4.3%) answered 6 correctly, 9 (39.2%) answered 7 correctly, 4 (17.4%) answered 8 correctly and 4 (17.4%) answered all 9 questions correctly.
Knowledge-based questions (questions 1–5)
The mean score for knowledge-based questions was 3.6 ± 0.99 (72%; 2–5) (maximum score 5). Three (13%) participants answered 2 questions correctly, 8 (34.8%) answered 3 questions correctly, 7 (30.4%) answered 4 questions correctly and 5 (21.8%) answered all 5 questions correctly.
Relating theory to practice questions (questions 6–9)
The mean score for practice-based questions was 3.4 ± 0.66 (85%; range 2–4) (maximum score 4). Two (8.7%) participants answered 2 questions correctly, 10 (43.4%) answered 3 questions correctly and 11 (47.9%) answered all 4 questions correctly.
Discussion
Hospital admissions and length of stay are increased for people with diabetes compared to age and sex-matched controls, although most of these admissions are not diabetes-related (Sampson et al, 2007). Nurses are at the forefront of clinical care as they are responsible for the day-to-day management of diabetes and recognition of the deteriorating patient. It is, therefore, of paramount importance that pre-registered nurses are prepared for this role, gaining the skills and knowledge to enable them to deliver high-quality care.
Results from this study investigating diabetes knowledge in final-year student nurses indicate some deficits, particularly related to general diabetes knowledge. This is in keeping with previous studies identifying knowledge gaps in this group (Trepp et al, 2010; Tawalbeh and Gharaibeh, 2014; Cardwell et al 2016). However, although knowledge deficits were identified, overall total score was reasonably high (77.8% correct answers), particularly for questions relating theory to practice, indicating that participants are prepared for their future roles.
It is difficult to compare knowledge scores with previous studies, as a variety of different questionnaires and scoring systems have been used. One local study involving 86 final-year student nurses reported lower total scores (55%), especially relating to insulin management (Cardwell et al, 2016). Furthermore, a study from North Jordan, using the previously validated Michigan Diabetes Knowledge Test (MDKT) to measure general diabetes knowledge and insulin knowledge, reported poor knowledge scores in both areas (Tawalbeh and Gharaibeh, 2014). In addition, a study comparing knowledge levels in Australian and Japanese undergraduate nurses, again using the MDKT alongside a clinical diabetes knowledge test, reported higher scores in general diabetes knowledge than clinical knowledge in both groups (Ramjan et al, 2017). This differs from the findings of this current study, where higher scores were noted in the questions related to application to practice (85% correct answers) than questions relating to general diabetes knowledge (72% correct answers). This may, in part, be due to the questionnaires used. The MDKT is a 23-item questionnaire that comprehensively assesses general diabetes knowledge, including insulin use, although the clinical diabetes knowledge test used by Ramjan et al (2017) was developed in house. It must, of course, be acknowledged that undergraduate nurse education and access to practice placement learning may differ in these countries compared to the UK. Indeed, Ramjan et al (2017) reported that Japanese students were exposed to more didactic teaching and less clinical contact with patients with diabetes compared to Australian students, although the curricula appeared similar. This could be applicable to the cohort of students in this study as, although they have all had access to the same university sessions, practice placements vary and not all will have had placements within a diabetes specialist area that could help consolidate knowledge.
Despite using different knowledge-assessment tools, several areas of poor knowledge have emerged from previous studies, notably the management of acute clinical situations, such as hypoglycaemia and insulin therapy (Trepp et al, 2010; Cardwell et al, 2016). In this current study, two questions related to the management of acute situations (hypoglycaemia and DKA). Almost 83% of participants identified the correct action to take in a patient with a hypoglycaemic episode compared to 60% in a previous study of registered general nurses that asked a similar question (Lange and Pearce, 2017). In addition, all participants in this current study were able to correctly list three common symptoms of hypoglycaemia, which is clearly important in recognising the deteriorating patient. With regards to DKA, 65% of respondents demonstrated correct application of theory to practice in this current study compared to 25.7% in a previous study of 116 qualified nurses, although it is unclear if the question related to a similar scenario (Abduelkarem and El-Shareif, 2013). Nevertheless, although these results are encouraging, 17% of participants in this study did not know how to manage an episode of hypoglycaemia and 35% were unable to manage a case of resolving DKA, both potentially life-threatening conditions. It is heartening to see that all but one participant (95.7%) in this current study were aware that, when unwell, people with type 1 diabetes must continue to take insulin injections. Lack of knowledge of insulin therapy has previously been identified as a knowledge deficit in both student and registered nurses from a variety of clinical areas (Abduelkarem and El-Shareif, 2013; Alotaibi et al, 2016).
It is difficult to say why student nurse participants in this study scored higher in questions related to application to practice than in other studies. It is possible that the focus of the university sessions were geared towards frequently encountered clinical situations and “take-home messages” owing to the experience of the presenter, who had only recently left clinical practice and was aware of common diabetes-related clinical challenges.
The majority (65.2%) of participants in this study felt that the combination of university and practice placement experience had given them confidence to look after people with diabetes. Nevertheless, 17.4% disagreed with this statement and this warrants further investigation. The relationship between confidence, perceived knowledge and actual knowledge is complex, with one study reporting a negative discrepancy between perceived and actual knowledge in relation to diabetes (Gerard et al, 2010). Conversely, in a study of Japanese student nurses, high diabetes knowledge scores were attained despite low levels of reported self-confidence (Ramjan et al, 2017). This has implications for current curricula and ongoing continuous professional development (CPD). Currently, the majority of university-based diabetes education is lecture-based. This is due, in part, to large cohorts. Alternative learning strategies, such as complexity-based, computerised scenarios, have been shown to have a positive effect on student nurses’ diabetes pharmacology knowledge when compared to more traditional teaching methods (P < 0.001; Dubovi et al, 2018). In addition, high-fidelity simulation as an adjunct to didactic sessions has been shown to have a positive effect on diabetes knowledge and decision-making in student nurses (Woda et al, 2019). Resource and cost implications of implementing such learning strategies need to be considered and balanced against the need to improve patient safety. Lifelong learning, evident in the NMC revalidation process (NMC, 2019), is a key element in the nursing profession. Therefore, working with diabetes specialist teams to develop undergraduate curriculum and ongoing CPD modules is essential.
Limitations
This study is not without its limitations, and the results need to be interpreted with care. The study involved students from one university, and difficulties with generalisation are acknowledged. The questionnaire used was developed in-house and subjected only to content validity. Finally, response rate was low (25%), so there is potential for non-response bias (Bruce et al, 2017). This low response, although disappointing, was not surprising as this cohort was subject to emergency standards affecting their university and clinical placement hours, owing to the COVID-19 pandemic (NMC, 2021).
Conclusion
This study has revealed knowledge gaps in areas of general diabetes knowledge and application to practice in final-year student nurses, although overall total scores were higher than previously reported studies. A review of future curricula should consider working in partnership with specialist teams and novel educational approaches as an adjunct to traditional teaching and learning strategies.






Key scientific developments presented at the conference.
6 Aug 2025