There are currently 4.4 million people living with type 2 diabetes in the UK. Provision of structured diabetes education around the time of diagnosis, and with annual reinforcement and review, is an integral aspect of care to support patient self-management (NICE, 2015).
Bedfordshire Integrated Community Diabetes Service (ICDS) has provided specialist community diabetes care across Bedfordshire since 2012. From inception, the ICDS has offered patients structured, evidence-based, group diabetes education sessions. In 2017, Clinical Commissioning Group funding was secured by the ICDS to create a specialist diabetes education service as part of the NHS Treatment and Care Programme. The diabetes education team was commissioned to provide group and one-to-one structured education sessions specifically for individuals diagnosed with type 2 diabetes in the past 12 months. ICDS specialist nurses and dietitians continued to provide education for patients who had lived with type 2 diabetes for more than 12 months, in the form of either the Diabetes Education and Self Management for Ongoing and Newly Diagnosed (DESMOND) Foundation course or an in-house structured education course, Advanced Diabetes Awareness and Management (ADAM).
ADAM covers similar ground to the DESMOND Foundation course but also includes sessions delivered by a podiatrist and representatives of the local health and wellbeing team. The North Bedfordshire ICDS team is currently working towards QISMET accreditation for the ADAM course. The plan is to offer ADAM across Bedfordshire to all patients who have been diagnosed with type 2 diabetes for more than 1 year.
Pre-pandemic
Prior to the pandemic, the education team delivered whole-day, face-to-face group DESMOND sessions on weekdays and Saturdays across the Bedfordshire area, excluding Luton (which is served by Luton ICDS). Patients of South Asian origin were offered the option of attending either DESMOND or a locally developed, culturally specific group education session. These sessions were held in community locations accessible to the local South Asian community and supported by two educators, one of whom has multilingual South Asian language skills.
The team also developed a structured education session designed to last approximately two hours, to be delivered in a patient’s own home for those who were unable to attend group settings. Those eligible for a home education visit included those who had a learning disability, mobility difficulties, or a hearing or sight impairment.
COVID-19
On 11 March 2020, the World Health Organization declared COVID-19 a pandemic. In the UK, the first lockdown was initiated on 23 March, and the education team immediately cancelled all planned face-to-face sessions for the following month. Patients already booked to attend were contacted to inform them that their course or one-to-one session would be rearranged as soon as possible.
In early May 2020, with the extension of the first lockdown, the team’s educators started contacting patients on the waiting lists to let them know that dates would be offered once lockdown was lifted and to ask if they had any questions. The most vulnerable groups were called first and then prioritised in descending order of age. Once the backlog had been cleared, calls then continued as patients were referred into the service.
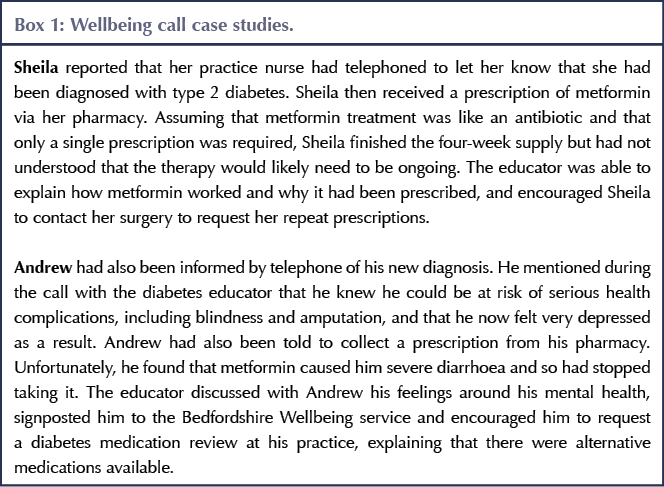
During these calls, some individuals reported that, due to lockdown, they had been given their type 2 diabetes diagnosis over the phone by their healthcare professional. Some felt that little or no further information about diabetes had been provided at that time, and they used the call to ask questions about managing their newly diagnosed condition. Gradually the educator calls became “diabetes wellbeing” calls. People isolated at home during lockdown mostly seemed grateful for the opportunity to be able to talk to someone. Examples of these wellbeing conversations are shown in Box 1.
The Diabetes UK booklet Everyday Life with Type 2 Diabetes was posted out to all patients who were contacted, and a login to the interactive, web-based MyDESMOND portal (see Northern et al, 2021 for more information) was offered to those patients who had access to appropriate IT and expressed an interest in online self-learning.
Patients were asked during these calls if they would like to receive a more formal diabetes education call, specifically to help them learn more about self-management of type 2 diabetes. The response was overwhelmingly positive.
Structured education calls
Using the material developed for the pre-pandemic home visits for structure and consistency, in July 2020 the team commenced providing two-hour diabetes education sessions via telephone for individual patients. A printed booklet (Appendix 1) summarising the information to be covered in the telephone call was sent to the patient, and during the call the educator guided the patient through the booklet material, with ample opportunity for questions as they arose.
Our South Asian language-speaking educator offered individual patient telephone calls in either Hindi, Urdu or Punjabi.
By September 2020, the team was able to offer the structured education calls via both telephone and NHS Attend Anywhere to those patients who had access to suitable video technology.
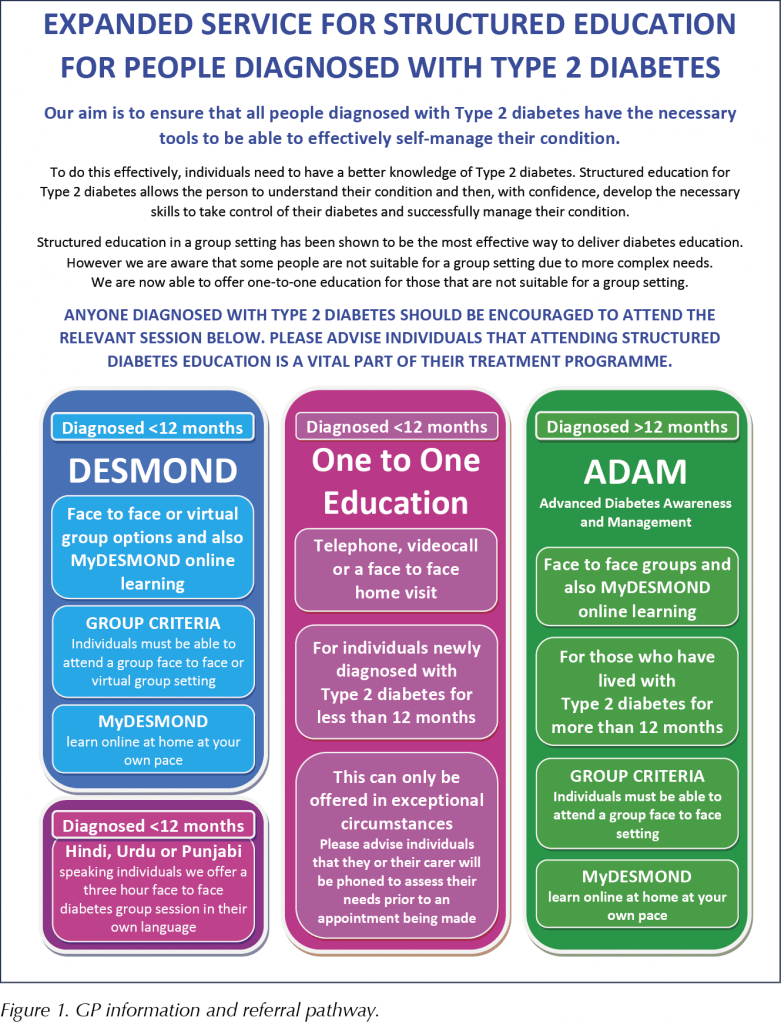
GP practices in the Bedfordshire area were kept updated about the services the diabetes education team could provide as the service evolved. A clear referral pathway (Figure 1) is provided for GPs and practice nurses to refer patients for structured education. Patient self-referrals are also accepted.
Virtual DESMOND groups
Between September and December 2020, the education team continued to provide telephone- or video-based, one-to-one educational calls. Following the national release of the virtual DESMOND slides, in January 2021 the education team practised delivering virtual DESMOND group sessions by trialling with a panel of individuals from the local Diabetes UK support group. We found that the NHS Attend Anywhere platform was unable to host groups of more than four people; however, Microsoft Teams could support larger groups and was approved by the Trust’s information governance department as an appropriately secure platform.
Our first virtual DESMOND course was delivered to patients in February 2021 over three 2-hour sessions via Microsoft Teams (Figure 2), with each session held at the same time and day on consecutive weeks. Evening virtual sessions were also offered but in a format of two 3-hour sessions. Finding that the 2×3-hour structure worked well, the daytime virtual courses were also moved to this format.
The team found that technical checks with each patient via Microsoft Teams prior to the course date helped troubleshoot any technical issues that the participants might have encountered on the day of the actual course, thus ensuring that the virtual courses start on time and mostly without technical hitches.
Referrals and attendance
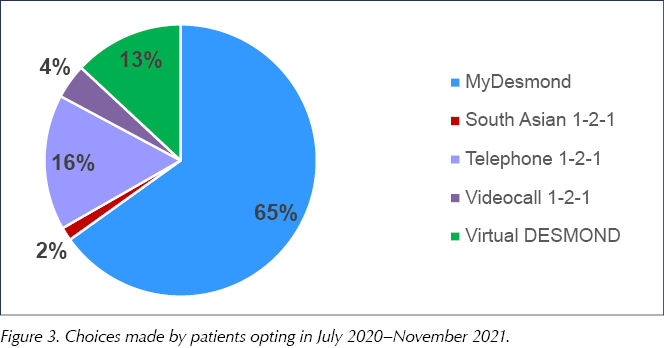
All patients were invited to opt in to the service by letter, and many were also telephoned as well. Between July 2020 and November 2021, the team delivered 90 one-to-one structured patient calls via telephone, as well as 23 via video between September 2020 and the end of November 2021. In the period of February–November 2021, 19 virtual DESMOND courses have been delivered to groups of 3–6 patients. Thirty seven percent of patients referred to the service between July 2020 and November 2021 attended a structured education option, 7% were in the process of choosing an option in November 2021 and the rest either had not responded, did not attend or had declined the service. Figure 3 illustrates the educational options chosen by those who opted for referral.
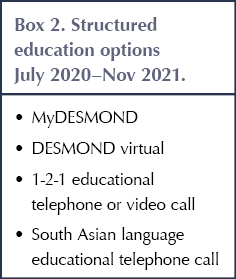
Telephoning patients to discuss the available educational options (Box 2) improved service uptake. Some patients were keen to accept the offer, while others required some explanation and counselling. Common responses from those declining to participate included: “I know a lot about diabetes; my mother had it”, “My wife has diabetes; we eat healthily”, “I’m too busy to attend” and “I don’t think it’s for me”.
Challenges
Challenges have typically been of a technical nature. On one occasion, Microsoft Teams failed across the Trust, and neither educator was able to join the virtual call, where six patients and an observer were waiting to join the session. Another time, despite successful pre-course technical checks, while the educators could join the virtual session, most of the patients were unable to. The only patient who did join was a passenger in a car travelling up the M1 motorway. The course was rescheduled!
One patient was under the impression that our educator was a cold caller trying to initiate a scam. It transpired that this particular individual had a YouTube channel showing videos of him stringing “scammers” along. He had started to record the encounter until he realised that our educator was making a genuine call about his recent diagnosis.
Observers
Observers including GPs and practice staff are invited to attend our virtual courses. To date there has been a renal dietitian, a student dietitian, a new member of the education team, a Primary Care Network care coordinator and two students researching dissertations on long-term health conditions.
Educator accreditation
One of our educators has been assessed and has passed their DESMOND educator accreditation via the virtual platform, with the assessor attending virtually along with the patients.
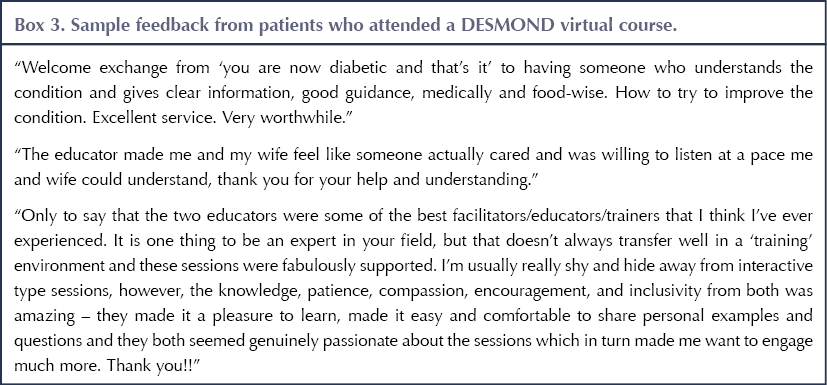
Patient feedback
Of 62 respondents who attended a DESMOND virtual course, 97% agreed that the course had been either useful or very useful in helping them to self-manage their diabetes. The remaining 3% did not give an opinion. Box 3 gives a selection of patient feedback comments.
Signposting
Participants are signposted at the end of a call or virtual course to appropriate local services. These include MoreLife, Bedfordshire Wellbeing and our Trust’s virtual weight management course for people with type 2 diabetes, Eat Smart Keep Active (ESTA). Virtual and face-to-face exercise opportunities in the Bedfordshire area are signposted and reliable online sources of health information, such as Diabetes UK and the British Heart Foundation websites, are recommended.
Plans in 2022
At the time of writing (January 2022), the team is planning to return to face-to-face DESMOND courses, with appropriate social distancing and hygiene measures in place. The team’s long-term vision is to ensure all patients newly diagnosed with type 2 diabetes are able to access structured education adapted to their needs.
Once face-to-face courses and home visits are reinstated, the education team will continue to offer a hybrid mixture of both in-person and virtual course options. Verbal feedback has shown that virtual education suits those patients who would not attend a group in person.
Patient engagement following referral continues to be a challenge. To increase uptake of the service, the team will continue to call referred patients to explain the available options as well as sending letters of invitation, including an introductory leaflet about DESMOND. The personal calls have noticeably increased the likelihood of patients opting into the service.
Despite the restrictions of the past 22 months, the entire team is proud to have been able to continue to support those newly diagnosed individuals who opted into the service with structured diabetes education and relevant information via telephone and virtual platform sessions. Many of the patients we have educated will now be a year or more into their journey with type 2 diabetes and eligible to attend a DESMOND Foundation or ADAM structured education course. We very much hope that they will take up these opportunities when available.
Acknowledgements
The authors wish to thank our wonderful team of administrative staff: Maria Buonpane, Hannah Saddington and Trudi Williamson.





How a new model of care has improved outcomes for people with diabetes.
2 Dec 2025