Technology, such as flash and continuous glucose monitoring (CGM) and continuous subcutaneous insulin infusion (CSII) via insulin pumps, is increasingly being used in the management of diabetes. Whilst these advances in technology allow for better insulin control and quality of life for the patients and families who use them, the majority require adhesive devices, such as CGM sensors, to be permanently in contact with the skin. Within 4 months of commencing on insulin pump therapy, 90% of users will report some form of skin complication (Berg et al, 2018). Skin assessment, ongoing prophylactic care and treatment of skin issues are required to support the continuing use of technology in people with diabetes.
Skin assessment
Although this article focuses on skincare in diabetes, generic medical adhesive wound care principles apply throughout.
Skin assessment is common practice in inpatient nursing. Many different tools are used to grade risk, mainly relating to pressure ulcer prevention; for example, the Waterlow score (Waterlow, 1985), Braden scale (Bergstrom et al, 1987) and Braden Q scale (Quigley and Curley, 1996).
CGM and CSII both have the potential to help reduce HbA1c levels; however, some users have reported stopping the devices due to ongoing skin problems, leaving them unable to access the technology available to support their diabetes management (Englert et al, 2014).
A full skin assessment and history should be taken before commencing adhesive medical devices (McNichol et al, 2013), including full visual skin assessment covering all device application sites and, if possible, obtaining photography of problematic areas such as current rashes, lesions and lipohypertrophy/lipoatrophy sites (Messer et al, 2018). Studies have shown that if individuals have previously experienced skin reactions or irritations, they are more likely to develop adhesive-related problems (Berg et al, 2018). A skin assessment should also cover nutrition and hydration, as these play a factor in ongoing skin integrity (Messer et al, 2018). Incorporating these aspects as part of an assessment allows timely delivery of information, equipping patients at the earliest opportunity to follow advised precautionary skincare measures.
Figure 1 shows the assessment tool developed and implemented by the paediatric diabetes team at Great Western Hospital, Swindon, as part of the background research into this article. Contributions and feedback from other members within the multidisciplinary paediatric diabetes team have allowed a full holistic approach to the assessment. The tool is being piloted for use during skin assessments. It is planned to introduce it within the South West Diabetes Network later this year, where further feedback and adaptations will be made in conjunction with the multidisciplinary teams across the network.
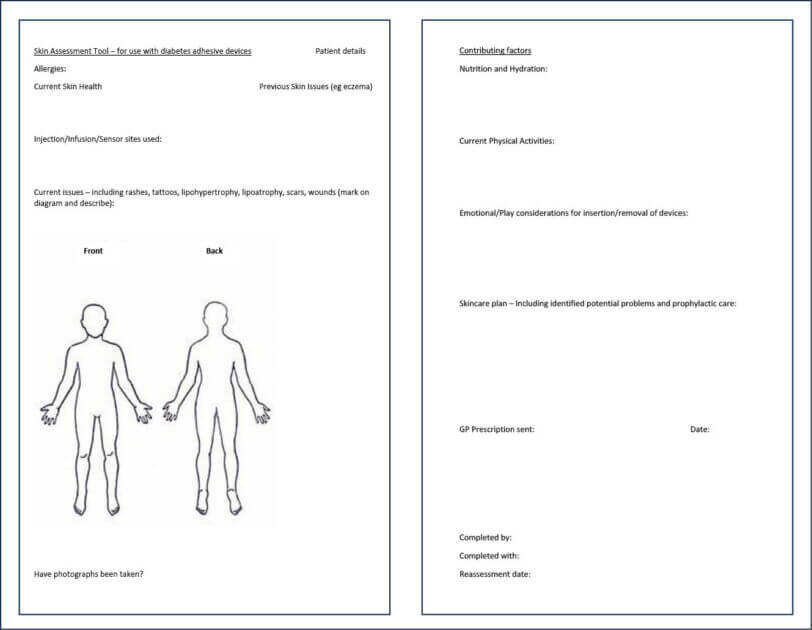
Figure 1. Skin assessment tool for use with adhesive diabetes management devices.
Skin preparation and prophylactic care
Skin preparation is a vital part of maintaining skin integrity in relation to medical device usage (Fumarola et al, 2020). A lot of skin issues, especially in paediatric patients, relate to the adhesion not lasting for the duration of the devices, which can have different causes. Englert et al (2014) outlined the following as contributing factors to these issues: limited body area for application; physical exercise; skin irritation in reaction to the adhesives; and climate.
Infusion sets, CGM sensors and transmitters are all required to lie flat against the skin for optimal adhesion (Englert et al, 2014). For patients, especially those in the younger age groups, who have less surface area, the options for areas of application are reduced (Forlenza et al, 2017). Location is also important, with a need to avoid areas that are likely to get caught or knocked easily, leading to premature removal of devices. Some patients have a preference to wear devices in locations that are not visible to others, further limiting the areas of application.
Site rotation is important for several reasons, including reducing skin trauma and allowing skin and cells to heal in between device usage (Fumarola et al, 2020). This is especially key in CSII management, to ensure insulin administration in different sites in order to protect from lipohypertrophy or lipoatrophy and to ensure optimal insulin absorption. Insulin has growth-enhancing properties which, when combined with reduced site rotation, can lead to lipohypertrophy (Gentile et al, 2016). While CGM devices do not administer insulin and so are not associated with this complication, they can still contribute to medical adhesive skin trauma.
Skin adhesion
The UK Chief Medical Officers advise children aged 5–18 years to undertake an average of 60 minutes of moderate-to-vigorous physical activity a day, while adults are advised to accrue 150 minutes of moderate-intensity or 75 minutes of vigorous exercise a week (Davies et al, 2019). Therefore, it is essential to ensure that CGM and CSII devices can withstand the individual’s normal physical exercise regimen. Issues with sensor adhesion and exercise can arise due to contact sports and movements; therefore, considering the site of application is essential.
Messer et al (2018) support the following guidance for general skin preparation. The skin should be cleaned with pH-neutral soap to remove dirt, oil and sweat prior to application. If perspiration is a big issue, a thin layer of anti-perspirant can also be applied to the skin post-cleaning to reduce the sweat underneath the adhesive area. Finally, ensure hair is trimmed so that the adhesive is applied directly to the skin (Messer et al 2018; Fumarola et al, 2020).
There are also various adhesive dressings that can be applied over the top of sensors that do not affect use, but which provide a larger adhesive surface; these have been reported by some users to improve sensor longevity. There are considerations when using secondary dressings over a sensor or cannula. First, they increase the area of the skin exposed to an adhesive dressing, which can impact in numerous ways. Increased adhesive surface area means more adhesive to remove, potentially increasing skin trauma with each removal. Some devices can be removed every 14 days which, combined with site rotation, allows time for the skin to heal. However, other devices need to be changed more frequently; for example, CSII cannulae are recommended to be changed every 3 days (Forum for Injection Technique, 2020), which, if combined with reduced surface area or limited sites for application, can lead to more frequent applications to the same area of skin. It is also reported that the more skin is exposed to adhesive, the more likely it is to develop irritation (McNichol et al, 2013); thus, by increasing the adhesive area, patients could be more susceptible to develop skin complications (Heinemann and Kamann, 2016).
An alternative to applying a secondary dressing to help with sensor adhesion is the use of adhesive barriers, which can come in the form of wipes, liquid, barrier creams or sprays (Fumarola et al, 2020). These are optimal for people who want to reduce the size or appearance of a secondary dressing. Liquid adhesive can be effective in children involved in water sports or physical activities (Englert et al, 2014). However, care needs to be taken to avoid applying adhesive barriers to the area where the cannula enters the skin, in order to reduce infection risk on insertion. From local clinical experience, adhesive barriers can be obtained on prescription via GP surgeries for paediatric patients, although inconsistency has been reported. Research or user feedback could be sought to help determine more effective methods of increasing adhesion; however, individual preference and individual assessment should be the leading contributor to these decisions (Messer et al, 2018).
Adhesive removal, which can cause trauma and increase local irritation at the device site, is another factor to consider. There are methods to teach patients regarding device removal, such as the low and slow approach (Messer et al, 2018). This involves slowly easing the dressing away from the skin in the direction of hair growth, keeping it low and close to the skin. Medical adhesive remover can also support device removal, and this is especially key if adhesive barriers have been used or sensors are being applied to an overused area (Englert et al, 2014). Medical adhesive remover can also reduce pain when removing the device and could be considered for all patients, but especially children and young people (Chase and Messer, 2016).
Irrespective of the method an individual chooses to support the adhesion and removal of their device, skin should be assessed for any damage with every change that involves adhesive, in order to help maintain skin integrity (Messer et al, 2018). Patients should be taught to assess for early signs of trauma and irritation on every adhesive change to enable early treatment and support (McNichol et al, 2013).
Messer et al (2018) have reviewed the literature on dermatology issues with both CGM and CSII administration, as well as currently available prevention and treatment options for patients experiencing these conditions. Englert et al (2014) evaluated a study conducted by the DirectNet group on children with type 1 diabetes who wore CGM sensors daily, and the complications that arose from wearing the devices. They evaluated different methods for overcoming the common issues that arose. Both papers offer insights into skin complications within diabetes device management and how these can be treated and, ideally, prevented.
Severe contact dermatitis reactions
Most skin irritations occurring from perspiration, occlusions and trauma caused by removal are likely to be controllable (Kamann et al, 2020). However, there are cases where a more severe allergic contact dermatitis can occur; these normally present in an uncontrollable itching, resulting in the user having to instantly remove the device. Reactions can start weeks, months or years following adhesive introduction (Messer et al, 2018). They are likely to be caused by the adhesive used within the dressing, such as isobornyl acrylate. To identify the adhesive as the allergen, rather than another part of the sensor, a patch test can be undertaken. Currently, adhesive ingredients are not routinely displayed on device packaging, but they can be obtained from the individual companies should this be required.
If an allergic reaction has occurred due to sensor usage, a barrier between the skin and adhesive allergen is required to prevent further reactions and allow the patient to continue using the diabetes technology. The most common way to overcome this barrier is to apply a tolerated dressing or barrier film to the skin underneath the device, leaving a small hole for the cannula to insert into the skin. There are multiple options for dressings, allowing patient preference and individual assessment to lead the choice. A thin, transparent dressing can be used or, alternatively, a hydrocolloid dressing may provide more of a barrier (Messer et al, 2018).
Using dressings underneath sensors can have some limitations, as identified by Kamann et al (2020). There could still be irritation at the cannula insertion site due to the small hole that allows the insertion, although patients have reported being able to apply devices through hydrocolloid dressings with the aim of avoiding this complication, following advice from online patient forums and fellow users (Messer et al, 2018). Additional considerations include ensuring that cannulae are fully inserted to the desired layer of skin tissue (interstitial fluid or subcutaneous tissue). Additionally, another dressing can affect patient comfort when wearing a device and, depending on the dressing used, the sensor may be prone to slipping (Kamann et al, 2020).
Individual patient assessment and discussion with healthcare professionals should take place as to whether hydrocolloid dressings or alternative dressings/barrier films are appropriate to support the continuing use of the adhesive device where an allergic reaction has occurred. Dermatology or tissue viability specialist referrals may be required for skin problems that are unable to be resolved within the diabetes team.
Emotional preparation
The emotional needs of the patient should be considered when both inserting and removing adhesive devices. The Forum for Injection Technique (2020) offers guidance regarding pain management and emotional considerations in children with diabetes. Paediatric patients have been reported to have lower pain thresholds, and pain should always be asked about and assessed. Psychosocial factors such as emotional distress, anxiety and anticipatory pain can all contribute to a patient’s perception of pain; these can have a negative impact on skin healing as they stimulate stress and can delay the body’s inflammatory healing response (Fumarola et al, 2020).
Techniques such as distraction or play therapy, including the use of soft toys and demonstration equipment, can be used with younger children (Forum for Injection Technique, 2020). Older children may benefit from other psychological interventions, including cognitive behavioural therapy (Cocoman and Barron, 2008). Consider referring the patient to psychology should further support be required to help with supporting the emotional impact of adhesive devices.
Conclusions
Skincare is an essential part of diabetes management, and with evolving technology the number of patients using adhesive devices is only going to increase. Ideally, a thorough skin assessment covering history and other lifestyle factors should be undertaken prior to commencing any adhesive devices. Principles of adhesive skincare can be applied to diabetes adhesive device management, and patient education on optimal skin preparation and prophylactic care can help reduce the complications that can occur due to, for example, poor removal techniques. Most skin problems associated with adhesive devices will allow for the user to continue with the associated product (Binder et al, 2015), and they should not necessarily stop the patient from accessing the available technology, provided healthcare professionals are able to support and guide the patient in optimum skincare.
Acknowledgements
The author acknowledges and thanks Dr Anne Phillips, Carole Gelder and the wider collaborative teaching and clinical team supporting the Children & Young Persons Diabetes Care Module at Birmingham City University for their teaching and guidance towards the production of this article.






Key scientific developments presented at the conference.
6 Aug 2025