The aim of maternity care is always to provide as positive an experience as possible for women and their family, and one of the most effective ways to achieve this is to focus on a level of health and well-being, as opposed to the more pathogenic focus on risk and morbidity (Ferguson et al, 2016). As health professionals, orientating to a health and well-being focused framework can be challenging when confronted with women with pre-existing medical conditions, such as diabetes. This may be due to the constrained nature of the complex multidisciplinary approach to care, where women can sometimes be absorbed into a systematic process in which the focus is not necessarily on the normal transition to motherhood issues that healthy women are exposed to.
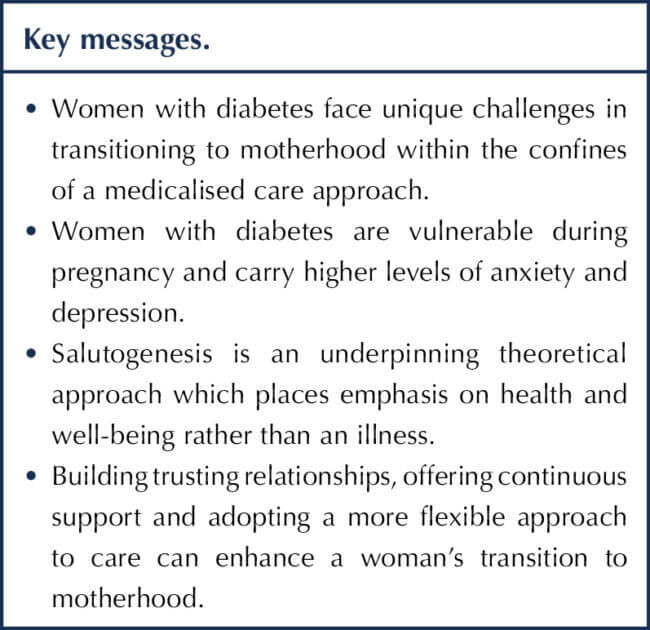
This article will explore some of the challenges women with diabetes can face when transitioning to motherhood and explore Antonovsky’s theory of salutogenesis (1987) as a strategy for nurses and midwives to support women at this crucial time in their lives.
Transition to motherhood
Making the transition to motherhood is recognised as an important psychological journey for a woman (Royal College of Midwives [RCM], 2021). Anticipated worries normally related to pregnancy include baby well-being, finance, partner relationships, body image and issues around the birth itself (Browne et al, 2014). Research suggests that whilst most women negotiate this journey reasonably well, a significant number of women have reported an element of emotional distress during pregnancy (Gourounti et al, 2012).
Anxiety during pregnancy has been linked to adverse obstetric outcomes, such as preterm birth and low birth weight, but also to challenges of adjustment to motherhood (Alderdice and Lynn, 2009). Relationship difficulties and feelings of loss of control can be commonly experienced by new parents (RCM, 2021).
For women with diabetes, this psychological journey can be particularly challenging. Pregnancies with additional care needs create vulnerability, and may expose women to higher levels of anxiety and pressure than those with a universally healthy pregnancy (Sparud-Lundin and Berg, 2011). Many women with diabetes are acutely aware of the possibilities of influencing their baby’s well-being through their own personal health management. They are expected to continuously maintain normoglycaemia for the duration of their pregnancy to minimise the risk of conditions, such as macrosomia, and congenital malformations, such as cardiac anomalies and neural tube defects (NICE, 2020). This continual pressure can impact on women’s psychological well-being, and create guilt and anxiety if an optimal lifestyle is not always maintained (Rasmussen et al, 2013).
It is suggested that, owing to the real risk of fetal loss from miscarriage or intrauterine death associated with their condition, women with diabetes can adopt a detached approach to pregnancy as a self-preservation tactic (Levy-Shiff et al, 2002). Levels of depression are recognised to be higher within the general population of people with diabetes and there is supporting evidence to show that women with measurable depression in the early stages of pregnancy have a higher risk of preterm birth. The specific causative factor for this is less easy to identify, with some suggestion of associated poor glycaemic control (Callesen et al, 2015).
Egan et al (2017) suggest that levels of psychological distress in pregnancy are higher among women with gestational diabetes compared with women with pre-existing diabetes. They hypothesise that this may be because women with pre-existing diabetes have had opportunities to control their condition prior to pregnancy, and have also already adapted to coping with the anxiety of a chronic medical condition. A systematic review by OuYang et al (2021) also identified that women with gestational diabetes carry higher levels of anxiety and depression than women with healthy pregnancies.
Qualitative research by Darvill et al (2010) identified a theme of change in relation to women’s self-concept when transitioning to motherhood. Women can feel that they lose control over their bodies during the early stages of pregnancy and feel more vulnerable to physical change, which creates an early transition from their own needs to that of their baby. Women with diabetes relate similar psychological impacts from the perspective of anxiety about the ability to cope with diabetes and pregnancy, and the responsibility of needing to care for a new baby (Rasmussen et al, 2013). Women with type 1 diabetes have expressed feelings of vulnerability, due to the medicalised management of their pregnancy, and the isolation from normality, due to their diabetes condition (Berg, 2005).
Qualitative research by Carlsson et al (2017) suggests that women with diabetes transition into motherhood with a new perception of accountability. There is a degree of transference from the primary responsibility of maintaining health to maximise fetal well-being to a focus of staying healthy to care for their newborn. Women often experience unstable glycaemia in the early postnatal period, which may affect their ability to care for the baby as effectively and independently as they would like. Unfortunately, this is a time when the intensive one-to-one multiprofessional team input that women are exposed to in pregnancy tends to filter away, leaving women more vulnerable and less able to seek advice (Carlsson et al, 2017). Helping women with conditions, such as diabetes, to feel more in control of their pregnancy may lower their degree of psychological anxiety (Lobel et al, 2002).
Can diabetes specialist nurses influence a woman’s journey with diabetes?
Although increased efforts are being made by midwives and diabetes specialist nurses (DSNs) to enhance the experience of pregnancy and birth for women, maternity care continues to be dominated by a focus on risk outcomes, rather than the more positive notion of well-being (MacKenzie Bryers and van Teijilingen, 2010). Women with diabetes receive significant multidisciplinary team input throughout pregnancy, with an intense regimen of antenatal visits to detect complications and manage the pregnancy as safely as possible. Whilst this is a vital component of care, there have been suggestions that, rather than experiencing a positive journey to motherhood, women with diabetes suffer a disconnect with nurses and midwives, mainly due to the medicalised focus on their pregnancy (Rasmussen et al, 2013).
This adds to the anxiety felt by women with diabetes, where the degree of surveillance in pregnancy can pervade their experiences (Browne et al, 2014). Women can also feel a sense of frustration when their expertise in their own medical condition is not recognised by health professionals (Rasmussen et al, 2013). A qualitative study by Toxvig et al (2022) identified that women with gestational diabetes can feel discontented and less likely to comply with care if their personal needs are not identified.
Women carry their own set of priorities and life issues, which optimally influence their decision-making ability. Health professionals may be more isolated in their medical focus, which may cause a dissonance in supportive care (Lyerly et al, 2007). Even though childbirth is now generally considered safe for women in the developed world, a perception pervades maternity care that pregnancy is a time of risk to well-being, with many health professionals still feeling that it is their duty to eliminate any degree of that risk (Jordan and Murphy, 2009). As Browne et al (2014) rightfully highlight, the mere fact that what is considered “normal” is discussed so prevalently in current literature emphasises the degree to which it has deviated from the central ethos of care.
What is salutogenesis?
The theory of salutogenesis was developed by Aaron Antonovsky in 1979. It resulted from work he carried out with female concentration camp survivors from the Second World War who demonstrated considerable resilience and positive attitude despite the unimaginable horrors they had witnessed and suffered. This triggered Antonovsky to ask, “What creates health?”, which consciously helped him to develop the theory (Antonovsky, 1987).
Antonovsky surmised that every individual is exposed to stressors during their life journey. He identified that these are an inevitable part of humanity and that, rather than viewing this negatively, recognised the need to have coping strategies in place to deal with them.
Antonovsky construed that it was people’s ability to assess and understand their situation (comprehensibility); the ability to access resources to promote coping (manageability); and the ability to find meaning and purpose (meaningfulness) that helped them to develop a sense of coherence, an ability to cope and a motivation to continue (Smith et al, 2014).
The foundations for an individual’s sense of coherence are grounded in their social, cultural and historical background, and include their genetic disposition and childhood upbringing. The stronger a sense of coherence that an individual carries, the more likely they are to cope with a situation and develop a sense of well-being (Downe et al, 2022). Smith et al (2014) have suggested a definition of a salutogenic outcome as being one reflecting positive health and aspects of well-being, as opposed to an illness focus.
If Antonovsky’s theory is translated and considered in relation to pregnancy and birth, it would recognise that they are potential stressors within a woman’s health continuum. These may require additional coping resources to be set in place to strengthen her sense of coherence, and thus enhance her ability to negotiate through the experience and maintain a sense of well-being. The challenge is recognising which women may be more vulnerable and require more support. A quantitative study by Linden et al (2016) utilising measures of well-being, including Antonovsky’s sense of coherence scale, suggests that women with pre-existing diabetes appear to carry reasonably high levels of self-efficacy in early pregnancy and a sense of coherence possibly related to greater adherence to glycaemic control. This indicates that DSNs could enhance a woman’s experience through encouraging and motivating her to maintain normoglycaemia.
How can DSNs utilise salutogenesis in practice?
Trusting relationships and a stable daily life balance are identified as core to optimising a positive pregnancy and birth experience (Dahlberg and Aune, 2013). Women value reliable, honest antenatal education that offers realistic expectation for birth outcomes, which relates directly to Antonovsky’s theoretical strand on comprehensibility (Aune et al, 2015). Every antenatal interaction with a woman affords opportunities for education in relation to pregnancy and diabetes, and opportunities to tackle the more personal concerns and anxieties that a woman may have.
The use of telemedicine, such as apps and other mobile phone technologies, is an area under current investigation for pregnant women with diabetes. Most young women are technologically proficient, and it is unlikely that they would be intimidated by this form of communication and management (Mackillop et al, 2014). This could offer women opportunities to reduce the number of hospital visits required during pregnancy, which, in turn, may offer more stability at home and increase maternal satisfaction levels (Hirst et al, 2014). Telemedicine allows women to feel a sense of control over their condition at a time when they often feel overwhelmed by the impact that pregnancy has on diabetes.
A systematic review by Ming et al (2016) suggests that the current lack of robust evidence for the use of telemedicine for this group of women leaves prediction of true satisfaction unclear, but highlights that it certainly offers no harm. A recent meta-analysis by Xie et al (2020) highlighted the significant lowering of HbA1c levels and maternal/fetal complications when women with gestational diabetes are monitored. DSNs could consider the integration of this technology into practice, and contemplate how community home visiting could be utilised as an alternative to hospital interactions to provide a sense of normality for women and to promote salutogenesis by reducing stress. The recent developments with COVID-19 have reconfigured many antenatal services and significantly increased the degree of telemedicine being utilised. It will be important to review the outcomes in research generated from that challenging period of isolation for pregnant women, to measure the social acceptability of this approach.
Participative decision-making and negotiation are key elements of supporting women with diabetes, especially recognising the expertise they carry in self-managing their condition. However, an important element of professional support is being able to recognise that, at times, women need release from the full burden of responsibility that having diabetes can bring. Berg and Sparud-Lundin (2009) suggested that, at times, women with diabetes can feel trapped between care professionals, particularly around issues of treatment management, where they feel overly responsible for managing care. DSNs and midwives can sometimes misinterpret or over emphasise the expectation for women to be independent and self-managing at a time when women may feel the need for additional support.
Conclusion
Salutogenesis offers a theoretical framework to consider the factors that can contribute to a woman’s ability to cope during pregnancy and birth. Understanding the individual needs of women with diabetes in pregnancy, and adopting a flexible approach to care, will enhance a woman’s experience during her pregnancy journey. Participative decision-making and concentrating on more positive health elements, rather than focusing on a medicalised agenda, could also help to narrow this gap. DSNs provide a key role in helping women with their transition to motherhood.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025