There is good evidence that insulin pump therapy can reduce both HbA1c and the frequency of hypoglycaemic episodes (Pickup and Sutton, 2008; Quirós et al, 2016), provided that the settings are correct in the insulin pump. The ability to tailor insulin administration to the individual’s requirements leads to a reduction in glycaemic variability, and this in turn improves aspects of quality of life, particularly in relation to food choices and exercise (REPOSE Study Group, 2017). Further evidence is emerging regarding the use of insulin pump therapy and reduced mortality (Steineck et al, 2015).
Insulin pump therapy demands a high level of self-management, and these individuals require regular review and support by a diabetes specialist team. NICE (2008) stipulates that this team should, at a minimum, include a pump-trained consultant diabetologist, a diabetes specialist nurse and a dietitian. The decision to start insulin pump therapy should be made following discussion by the whole specialist (multidisciplinary) team.
This article provides basic information for non-specialist staff about what a pump is, how it works, the pros and cons, how to identify emergency situations and how to signpost the patient to appropriate services.
What is an insulin pump?
For any healthcare professional to be able to support this group of individuals, it is vital to have a basic understanding of how insulin pump therapy works. With so many insulin pump manufacturers (some of which have more than one model of insulin pump), it is very easy to get extremely confused with all the different functions and facilities. However, in basic terms, an insulin pump is a battery-operated, portable and programmable device that delivers rapid-acting insulin (Everett, 2004). It consists of several components:
- A mechanical pump operated from the battery – this operates like a piston and pushes insulin out of the reservoir according to pre-programmed settings (basal programme) or on the operator’s instruction (bolus dosing).
- A reservoir (a small syringe that holds the rapid-acting insulin within the pump).
- A cannula (a small needle or plastic device) inserted into the subcutaneous layer of the skin.
- Tubing that connects the reservoir and cannula together.
How does a pump work?
Basal rate
The basal insulin infusion rate is usually adjusted according to the individual’s requirements at different times of the day but can be varied hourly. It can also be temporarily adjusted upwards or downwards by a fixed percentage during periods of illness or exercise; this is referred to as a temporary basal rate (TBR). For some people, there may be more than one basal rate setting saved (e.g. a work-day setting versus a weekend setting). This allows the person to switch between the settings easily according to their activities (Diabetes Technology Network UK, 2018a).
Bolus dosing
Bolus doses can be delivered by the insulin pump in a number of different ways. The insulin-to-carbohydrate ratio (e.g. 1 unit of rapid-acting insulin for 10 g of carbohydrate) is pre-programmed in the insulin pump settings and can be adjusted for different times of the day according to the individual’s requirements. These are usually given with meals and can be delivered via the pump either as:
- An immediate bolus. This gives the suggested amount of insulin all at the same time.
- An extended bolus. This gives the suggested amount of insulin but prolongs the delivery time, and is usually used for foods with a low glycaemic index (GI) or those high in fat or protein.
- A combination bolus. This is a mixture of an immediate and extended bolus and allows for the quick-acting carbohydrates to be managed by the immediate part of the bolus and the longer-acting/lower-GI carbohydrates to be managed by the extended part.
- A correction bolus. Nearly all pumps incorporate bolus calculators. This function allows users to correct blood glucose levels accurately by adjusting bolus advice according to the amount of insulin still active in their system from a previous bolus. The specialist team will calculate how much 1 unit of insulin will lower the blood glucose level by, and this setting – often referred to as insulin sensitivity factor (ISF) – is inputted into the insulin pump.
Hypoglycaemia
The causes of hypoglycaemia are often multifactorial; however, by looking at the information stored in the insulin pump device, the cause can often be identified. The cause may be attributed to excess insulin administration, either due to an overestimation in the bolus dose of insulin or a build-up of active insulin from previous insulin doses (insulin stacking); incorrect settings in the pump device; or exercise.
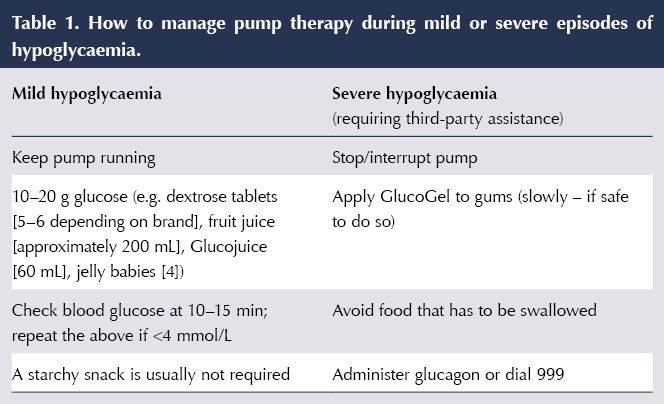
Assuming that the pump settings are correct and the hypoglycaemic event is caused by one of the reasons identified above, the person would be advised to follow the advice in Table 1 for correction of blood glucose levels. There is generally no need to eat a long-acting-carbohydrate snack once the blood glucose level has been corrected (Pender, 2012). If the user is struggling with persistent episodes of hypoglycaemia, they should be advised to contact their specialist team for review as soon as possible.
Hyperglycaemia
One of the most common causes of hyperglycaemia with insulin pump therapy relates to cannula failure (displacement or incorrect insertion). If this is not detected promptly, it can lead to insufficient levels of insulin being delivered and has the potential to result in ketosis/ketoacidosis within a matter of hours (Diabetes Technology Network, 2018a). Insulin pump users should be encouraged to explore the reasons why they have developed high blood glucose as soon as it is detected. Box 2 highlights some of the reasons for hyperglycaemia and areas we can encourage patients to explore (Ponder et al, 2008).
Insulin pump users should be advised that they must carry, or have access to, an alternative means of insulin delivery (pens or syringe), as well as blood glucose and ketone monitoring equipment, in case of pump failure or illness/ketosis. They should also have access to long-acting insulin and know the dose to take in the event of pump failure. These should remain on their repeat prescriptions and be carried with their emergency supplies at all times (Diabetes Technology Network, 2018a).
How to identify emergency situations
Illness
It is imperative that insulin pump users know the sick day rules and also have access to in-date blood ketone monitoring. As recommended by the Diabetes Technology Network (2018a; 2018b), they should be advised to:
- Check for ketones if they feel unwell or have elevated blood glucose levels >14 mmol/L (if not explainable by e.g. excess food intake).
- If there are no ketones present and no cannula/infusion set issues, users should correct their blood glucose using the insulin pump.
- If ketones are present, they should double the correction bolus and administer this with a pen device or syringe, and then change the cannula and infusion set.
- Continue to test blood glucose levels and ketones every 2 hours until ketones are resolved (≤0.3 mmol/L) and illness has settled with BG returning to usual levels (this may be different for each individual).
- Continue to correct blood glucose levels every 2 hours (either by using a pen device or the insulin pump bolus function – as above).
- Be actively using a temporary bolus rate.
- Drink plenty of water.
It is important to remember that the pump does not know when the user is unwell, and they will need to proactively manage elevated blood glucose levels. If they are unable to do this, they must seek specialist advice urgently or present at Accident & Emergency.
Admission to hospital
As over 90% of people with diabetes are admitted for non-diabetes-related issues (NHS Digital, 2018b) and are usually admitted to the clinical area that best fits the cause of admission, they are extremely likely to be cared for by teams with limited or no experience of insulin pump therapy. The Diabetes Technology Network (2018b) states that approximately 7% of people with diabetes who are admitted to hospital have type 1 diabetes, and only a fraction of these will be using insulin pump therapy. Therefore, most non-specialists are unlikely to have even seen a pump, let alone be familiar with the functions. As a result, if the pump user is not able to self-manage their therapy, most non-specialist teams will choose to discontinue the insulin pump and switch to variable-rate insulin infusions or subcutaneous injections of insulin, as these are therapies that all staff are generally experienced in or trained to manage.
There are also areas of the hospital where pump therapy may not be suitable (e.g. MRI/imaging, as the magnetic fields may cause integral damage to the insulin pump). In these instances, it is also advised to remove the insulin pump and store it in a safe place (e.g. a locked medicine cabinet) for this period. If the interruption of insulin pump therapy is expected to be for a prolonged period (i.e. >2 hours), the team would be advised to switch to the therapies mentioned above (Diabetes Technology Network, 2018b).
It is important that the specialist diabetes teams be involved in any care decisions for these individuals as soon as possible. If the admission is planned and the specialist teams are informed, often a treatment plan can be discussed with the patient and relevant services prior to the admission, and this enables the person with diabetes to manage their own therapy.
Considerations for initiating insulin pump therapy
In order to gain optimal outcomes with insulin pump therapy and demonstrate an appropriate use of NHS resources, individuals must be assessed for their suitability using a structured process that involves the whole multidisciplinary team. This process should consider the following characteristics (NICE, 2008; Diabetes Technology Network, 2018a):
- Has the person been provided structured education and are they able to carbohydrate count?
- Are they able to understand and implement the principles of intensive insulin therapy (i.e. adjust insulin as required, never miss injections)?
- Are they testing blood glucose levels at least four times a day or using flash/continuous glucose monitoring devices that demonstrate regular monitoring of glucose levels?
- Are they motivated to pursue CSII therapy and improve diabetes control?
- Do they engage with diabetes services (attend appointments/screening)?
- Do they have realistic expectations of CSII (understand how the therapy works and what is involved)?
- Are they able to manage the technology?
- Do they have any psychological factors that may impair safe CSII use that need to be explored (e.g. psychosis, severe anxiety or severe depression)?
The majority of people who meet the criteria above but continue to experience an elevated HbA1c or frequent hypoglycaemic events are usually considered for insulin pump therapy. Additional considerations include those who are unable to manage glycaemic excursions related to the dawn phenomenon or exercise, despite the intensive therapy and support given throughout the assessment process. The specialist team may also consider the use of CSII for people from additional subgroups of service users, if there is clinical need for this therapy under NICE NG3 and NG17 guidance (NICE, 2015a; 2015b).
Pros and cons
When offering insulin pump therapy, it is important that the individual consider all the pros and cons, as highlighted in Table 2 (Diabetes Technology Network, 2018a).
Travel
Traveling with an insulin pump requires some extra considerations on top of the usual planning for people with diabetes. These individuals should:
- Carry all supplies in their hand luggage. When traveling by air it is important to remember that, if put into the hold, insulin can freeze, rendering it useless. They should also carry consumables in their hand luggage, as any loss of luggage could cause significant risk to them. Obtaining replacement insulin and consumables can take time and can be costly.
- Carry a letter from their doctor/specialist team. This must inform security staff of the requirement for insulin pump therapy, the care and management of the equipment, and the need to carry sharps, medicines and emergency treatments. Most of the insulin pump manufacturers will also have template letters available, and many will provide them in specific languages if required for foreign travel.
- Keep their pump out of X-rays/magnetic fields, as these may damage the internal integrity of the pump.
- Replace the cannula, reservoir and tubing every 2 days whilst in hot climates, as insulin quality deteriorates more quickly in the heat. In addition, there also may be issues with cannula displacement if the adhesive is affected by heat, sweat or swimming.
- Store insulin supplies in a fridge.
- Use a temporary basal rate according to blood glucose levels. Remember that insulin absorption rates are altered in hot/cold climates.
- Adjust for time zones. Individuals are usually advised to wait until they arrive at their destination and then change the insulin pump to local time.
- Disconnect the insulin pump during take-off and landing (extreme changes in pressure may affect the pumping mechanism and could deliver an unexpected insulin bolus).
- Get travel insurance. Ensure this covers the insulin pump device as well as medication and medical assistance, if needed.
- Carry medical alert identification in case of an emergency. This allows others to seek the right medical attention promptly.
- Specialist teams would also advise that individuals take long-acting insulins in an emergency pack in case of pump failure. In addition, they would advise individuals to take a copy of their insulin pump settings and familiarise themselves with conversion to injection calculations/management in case of emergency.
Indications to discontinue pump therapy
Until recently, there was no clear guidance for clinicians regarding the discontinuation of insulin pump therapy, and this led to widespread variance in decisions made by specialist teams. However, the introduction of the best practice guidance from the Diabetes Technology Network (2018a) has provided some clear structure to this process. This document states that the decision to discontinue insulin pump therapy should be made after discussion with the whole specialist team. These discussions usually proceed if there is a concern that insulin pump therapy is not safe or there is no clinical benefit. Reasons for discussion may include the pump user requesting to stop; the absence of adequate glucose testing (the pump may be removed temporarily or permanently if there is no evidence of improvement); admissions with ketosis or ketoacidosis; cognitive impairment; non-attendance at clinic for reviews; failure to improve HbA1c or reduce frequency of episodes of hypoglycaemia. In any of these cases, the insulin pump user must be supported by the specialist team with education and psychological support, with the aim to return to insulin pump therapy again, if this is appropriate.
Conclusion
The population of insulin pump users is growing in the UK. Despite NICE (2008) guidance specifying that these individuals require specialist teams to provide care and support, there is a growing need for non-specialists to have some basic knowledge in order to identify emergencies and signpost users to correct services, especially as many will present to non-specialist areas with difficulties. Many people who could benefit from this therapy will be identified in community and GP practices, and it is hoped that this article will assist in the identification and referral of these individuals to specialist teams for further assessment.
To achieve the best possible outcomes with insulin pump therapy, these individuals will need a clear understanding of what the therapy is and how it may aid them to achieve their therapeutic goals. This therapy is complex and requires individuals to persistently and consistently:
- Check their blood glucose levels more than four times a day.
- Use the technology correctly.
- Carbohydrate count.
- Change cannulas every 2–3 days.
- Attend clinic reviews.
- Download and review pump data.
The flexibility of these devices enables the user to adjust settings instantaneously for daily activities and prospectively to reduce risks associated with recurrent hypoglycaemia whilst improving HbA1c. If used in accordance with NICE guidance, insulin pump therapy has the ability to improve the individual’s quality of life and reduce the risks associated with hypoglycaemia, and has been clinically approved as cost-effective in this particular cohort.








Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025