Diabetes has a significant focus within the NHS Long Term Plan in terms of prevention, access to diabetes healthcare services and promoting self-management (NHS, 2019). It is important that healthcare services invest in ways to support people to manage their diabetes to reduce pressure on secondary care and costs associated with poor glycaemic control (Stedman, 2020).
Diabetes and oral health
There is an increasing amount of evidence of the association between poorly controlled diabetes and oral health (Preshaw and Bisset, 2014). People living with diabetes are more likely to develop oral health conditions, including dry mouth, dental caries, fungal infections, poor wound healing and increasing severity of periodontal disease (NHS England, 2019). Periodontal disease is a major cause of tooth loss, which in turn impacts on nutrition, self-esteem and quality of life. Almost 50% of the global population is affected by some form of periodontal disease. The risk of periodontitis increases by two to three times in people with diabetes and is associated with poor glycaemic control (Preshaw and Bisset, 2019).
There is a bidirectional relationship between periodontitis and diabetes (Poudel et al, 2018). Hyperglycaemia results in an increase in inflammatory markers in the saliva and gingival crevicular fluid. In the presence of oral bacteria, the immune response is exaggerated and leads to accelerated periodontal tissue destruction. Conversely, inflammation arising from chronic periodontitis has also been found to elevate HbA1c levels and impact on blood glucose levels.
There is a need to include oral health and diabetes awareness in preventative health programmes. For people to make positive changes to their lifestyle habits, they need to be aware of their risk factors through preventative healthcare messages. There have been efforts to increase awareness of the links between poor oral health and diabetes. NHS England (2019) has released the document Commissioning Standards for Dental Care for People with Diabetes, which discusses the need for integrated care pathways and the importance of signposting patients with diabetes to periodontal screening.
Increasingly, more efforts are being made to extend oral health advice to multidisciplinary healthcare professionals, and this should include the diabetes team (Health Education England, 2016). Mouth Care Matters, a Health Education England quality improvement initiative, is an example of a programme that focuses on the education and upskilling of healthcare professionals.
Nurse-led management of diabetes
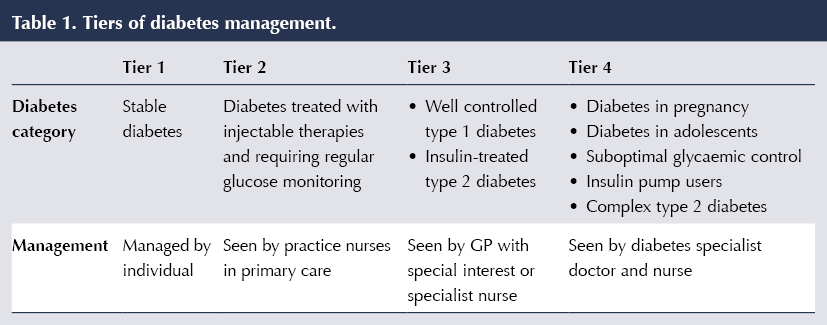
After being diagnosed with diabetes, people will have their care managed in clinics in either primary or secondary care depending on their needs and the type and severity of their condition. People with more complex needs, including those with suboptimally controlled type 1 and type 2 diabetes and those requiring insulin pumps, will typically be seen in Tier 3 and 4 specialist diabetic clinics (Table 1). Observations of these clinics at the local hospital by the authors found that people are typically booked in with a diabetes specialist nurse for 20–30 minutes. They are given tailored healthcare advice, supplemented with resources such as leaflets and posters, and are signposted to appropriate health services. However, the authors observed that there was no discussion about any aspect of oral health at these appointments, and there were no leaflets or posters in the waiting room about oral health or visiting the dentist.
The primary aim of this survey was to assess whether people attending Tier 3 or 4 diabetes clinics are aware of the links between periodontal disease and diabetes, and whether they had received information about this from their diabetes team or a dental care professional.
Methods
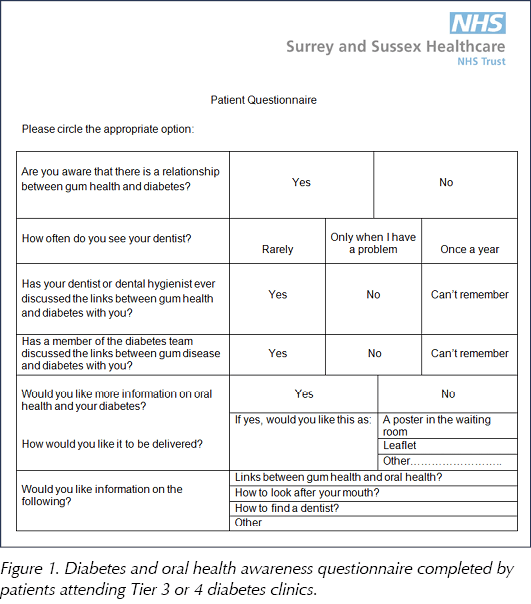
Patient questionnaire
A short questionnaire was developed for patients attending the nurse-led Tier 3 and 4 clinics to complete in the waiting room. It included questions on their awareness of the links between oral health and diabetes, dental attendance and whether they would like further oral health information and in which format (Figure 1). The questionnaires were voluntary and did not ask for any patient-sensitive information.
The research office at the hospital was consulted and advised that ethical approval was not needed for this questionnaire. The survey was registered with the Clinical Governance department.
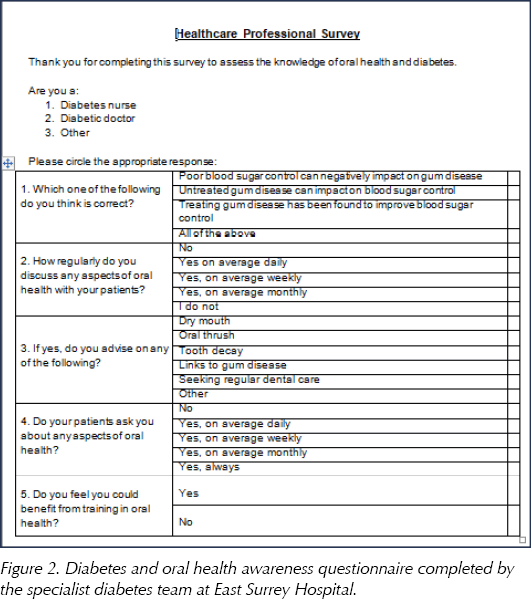
Healthcare professional questionnaire
The diabetes team at East Surrey Hospital consists of registrars, consultants, diabetes specialist nurses and support staff, who meet once a week for teaching and information-sharing sessions. These sessions cover a range of topics, including diabetes medications, audit presentations and teaching from other specialities. A training session on oral health was arranged with the team, covering the links between oral health and general health including diabetes, and providing information on how to access dental care. A survey (Figure 2) was distributed before starting the training to determine the team’s baseline knowledge about the links between diabetes and periodontitis, whether oral health links are ever discussed with patients and the perception of a need for further oral health training. The results from this survey were used to develop further training for the diabetes team.
The information from these surveys was entered into an Excel spreadsheet and analysed. Descriptive statistics were used to summarise the data and expressed as percentages.
Results
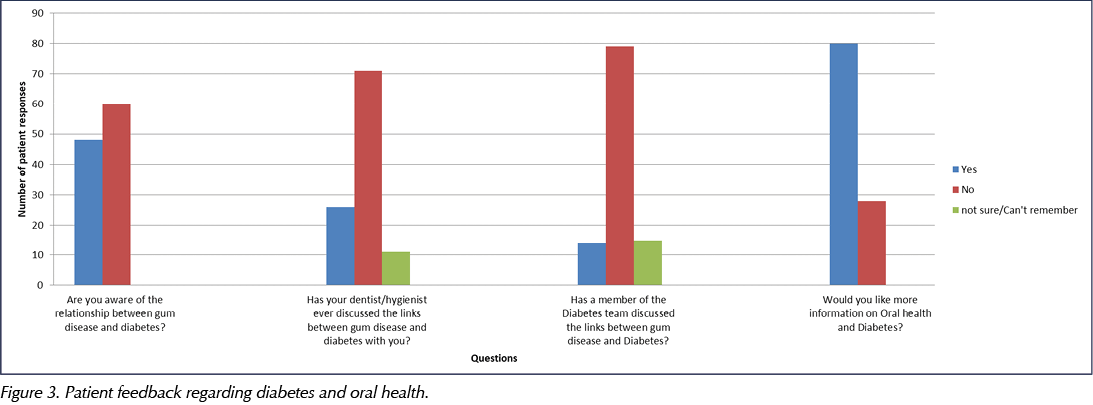
Survey of people with diabetes
A total of 108 patient questionnaires were completed and analysed. Over half of attendees at the diabetes clinics (60 of 108; 55%) responded that they were not aware of the relationship between gum disease and diabetes (Figure 3). Two thirds of patients (71 of 108; 66%) reported that the links between their diabetes and gum health had never been raised by the dentist at a dental visit. Around one quarter (26 of 108; 24%) recalled discussing the links with their dentist, and the remaining 10% (11 of 108) could not remember whether this had been discussed.
Seventy-three percent of respondents (79 of 108) reported that they had not received information from their diabetes team of the links between gum disease and diabetes.
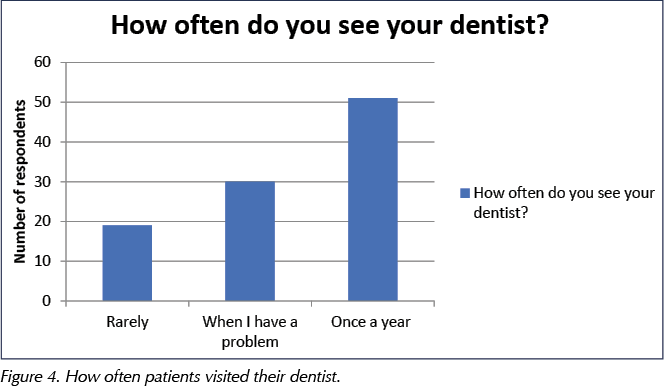
Twenty-eight percent of patients (30 of 108) answered that they only see their dentist if they have an urgent issue and 18% (19 of 108) said they rarely attended the dentist (Figure 4).
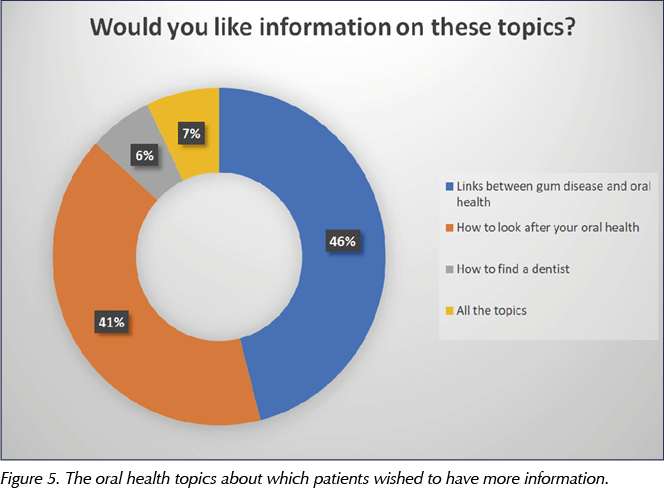
Three quarters of respondents (80 of 108; 74%) claimed they would like more information about oral health and diabetes (Figure 5).
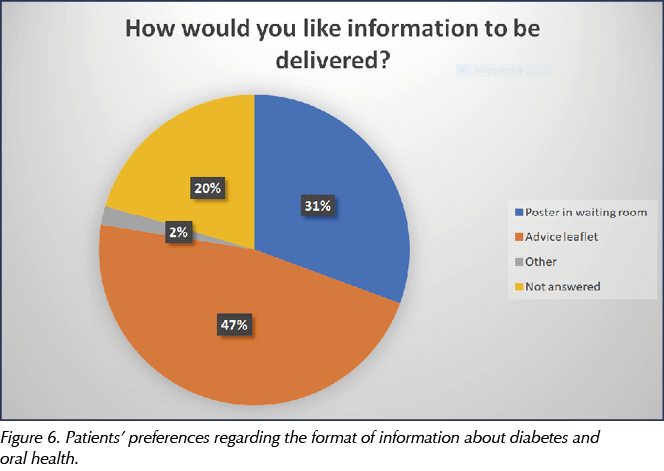
When asked how they would like information to be delivered, the most popular answer was advice leaflets (46 of 108; 43%). Twenty-eight percent (30 of 108) said they would like posters outlining important healthcare messages in the clinic waiting room. Nine percent (10 of 108) preferred digital forms of communication, mainly via email and websites, and 20% (20 of 108) did not answer the question (Figure 6).
Survey of diabetes team
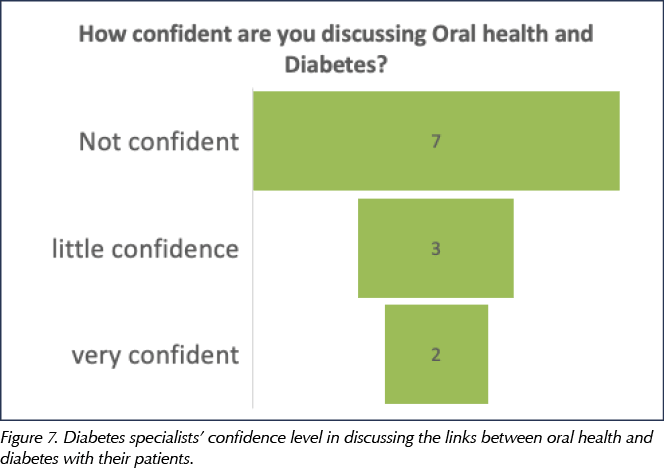
Overall, 83% of specialist diabetes team members (10 of 12) reported a lack of confidence in discussing the links between oral health and diabetes with their patients (Figure 7), and 75% (9 of 12) stated they would like to receive training in delivering oral health advice to their patients.
Discussion
The findings from this survey indicate a relatively low awareness of the links between oral health and diabetes amongst people with diabetes. The diabetes Commissioning Standards released in 2019 state that 100% of dentists should be raising awareness of periodontitis and diabetes with their patients (NHS England, 2019).
Fifty-five percent of patients in this study reported that they were unaware there was a link between their diabetes control and their oral health. This is particularly concerning considering that these individuals were in the highest risk categories for diabetes (Tier 3 and 4 clinics) and were accessing regular healthcare appointments. There is a larger cohort of people living with diabetes (Tier 1 and 2) who visit healthcare professionals less frequently in primary care, and it can be extrapolated that these will have similar, if not lower, levels of awareness. Given the strong evidence of the benefits of regular periodontal treatment for people with diabetes, it is important that this information is accessible to patients as it may modify their oral health behaviours.
According to the last Adult Dental Health Survey, in 2009, 29% of patients did not visit a dentist regularly (Hill et al, 2013). A large percentage of the population – an estimated 10–11% in the UK – is living with undiagnosed periodontitis (Steele and O’Sullivan, 2011), and many patients report difficulties in accessing dental services (Freeman, 1999). This will have been made worse by the impact of the COVID-19 pandemic (COVID-19 Dental Services Evidence Review Working Group, 2020).
There is strong evidence to suggest that intensive periodontal therapy can improve glycaemic control; clinically significant reductions in HbA1c of 3–4 mmol/mol have been observed 3–4 months after non-surgical periodontal therapy (Preshaw and Bissett, 2019). This can reduce both the need for treatment intensification and complications associated with raised HbA1c levels. For the NHS, appropriate dental treatment for periodontitis can potentially lead to savings of over £124 million (NHS England, 2019).
An increased knowledge of the link between oral health and diabetes amongst people living with diabetes may result in more regular visits to their dentist and dental hygienist/therapists, and to improvements in oral hygiene habits. From the literature, it is clear that there are both personal and cost benefits if people with diabetes maintain good levels of periodontal care.
It is important that healthcare professionals who come into contact with people with diabetes are aware of the oral health links themselves; this includes both dental professionals and diabetes teams. Evidence suggests that oral health training for doctors and nurses is limited (Health Education England, 2016; Binks et al, 2017). A study by Doshi et al (2019) found that 94% of junior doctors had no previous training in oral health and 100% did not feel confident to manage oral conditions if they were presented to them. Blaylock et al (2020) showed that doctors in primary care and hospitals had very limited previous oral health training and found training sessions very useful for their role. In our study, among the 12 members of the diabetes team who attended the training session, 83% did not feel confident in delivering any oral health messages. Oral health should form part of mandatory training for doctors and nurses who care for people with diabetes.
Preventative advice is a very important part of healthcare and can contribute to reducing morbidly and mortality of many long-term conditions (Goodwin et al, 2010). The effectiveness of oral health promotion measures has been demonstrated in a systematic review by Hausen (2005), which highlighted that oral health promotion was effective in reducing plaque and bleeding scores in patients suffering from periodontal disease, albeit only in the short term. Oral health promotion should be included in overall general health preventative programmes. There has been an increased focus in the NHS on population health management, an approach for improving the physical and mental health outcomes and wellbeing of people whilst also reducing health inequalities within and across a defined population. Oral health could be included in population-level health management by increasing awareness among non-dental professionals within, for example, Primary Care Networks.
As patients attending these specialist Tier 3 and 4 clinics have more risk factors or are particularly susceptible to diabetes-related complications, it is important that they receive general oral health advice in addition to advice they already receive on other diabetes complications, including eye, foot and kidney disease. The International Diabetes Federation (2009) has developed guidelines that recommend that doctors in primary care ask patients about oral self-care and whether patients have noticed any signs of gum disease. This should be performed at a basic level by all healthcare professionals caring for the person with diabetes and, if necessary, the person should be advised to seek advice from a dental professional. It is recognised that oral health is not included in self-management education programmes such as DESMOND. There is a clear need for education regarding diabetes and its oral health complications; these should be made available to people with or at risk of diabetes at the earliest clinical contact.
The limitations of this study include the small sample size. Nonetheless, the findings highlight the need for further research into this area to look at the most effective ways to deliver oral health awareness and increase health behaviours.
It was planned to repeat this survey, but to date this has not been possible owing to the COVID-19 pandemic.
Further oral health training
A large proportion of patients (80 of 108) expressed a desire for further information about the links between diabetes and oral health, which is very encouraging. The most preferred methods were written information leaflets and posters in the waiting room. In addition, the majority of patients wished for further information on how to look after their oral health and some wished for help to find a local dentist for treatment. In response to this, the diabetes team was provided with a range of leaflets that had been developed (see Further resources below). A further Trust-specific leaflet was developed on how to access local dental services and NHS payments, as this had been raised repeatedly. All these leaflets were made available in the waiting room and, as a result of the COVID-19 pandemic, online.
Oral health training is now part of the teaching programme for the diabetes team at East Surrey Hospital. Training is also made available to general medical practitioners through Integrated Care Partnerships (Blaylock, 2020). As discussed in the commissioning guidelines, it is important for medical and dental teams to communicate effectively about the oral health of patients living with diabetes. Due to the bidirectional relationship that exists between gum disease and diabetes, integrated care can improve the patient’s disease status.
Conclusions
There is a great need to increase awareness amongst people living with diabetes on the importance of oral health. This information should be disseminated from both dental and non-dental professionals. There is a need for better integration of oral health into general healthcare, and this is achievable through training.
Further resources
 |
Scottish Dental Clinical Effectiveness Programme (SDCEP) leaflet – Diabetes and your Oral Health
Available at: https://bit.ly/2NmAXJX |
 |
British Society of Periodontology (BSP) Leaflet – Diabetes and gum disease: information for patients
Available at: https://bit.ly/3it3Rnd |
 |
British Society of Periodontology (BSP) Leaflet – Diabetes and gum disease: information for healthcare professionals
Available at: https://bit.ly/3sGn4q4 |
 |
Diabetes.co.uk online resource – Diabetes and dental health
Available at: https://bit.ly/3bVyosp |





Developments that will impact your practice.
29 Aug 2025