Abnormal liver tests and NAFLD in diabetes: A primary care approach
Sarah Davies
GP, Cardiff
● Abnormal liver function tests are very common in primary care – look for patterns and make an active diagnosis if possible.
- ALT the most abnormal = hepatic cause.
- Alkaline phosphatase the most abnormal = cholestatic cause; can be from bone – if GGT also elevated then liver cause.
- AST – less liver-specific than ALT, sensitive indicator in alcoholic liver disease.
- GGT – in liver but not bone. Commonly elevated due to obesity and alcohol. Non-specific for liver disease but good predictor of liver mortality.
● NAFLD is common and not benign, especially in people with metabolic syndrome or type 2 diabetes. Can progress to steatohepatitis and fibrosis. Primary care role:
- Identify and make active diagnosis.
- Assess likelihood of significant fibrosis (FIB-4, NAFLD fibrosis score – see RCGP liver disease toolkit) and refer if required.
- Support to achieve weight loss.
- Cardiovascular risk management. Statins are generally safe: no need to “over-monitor LFTs”.
- Potential for benefit from newer diabetes medications (GLP-1 RAs and SGLT2 inhibitors), although not yet licensed for this indication.
● Take-home point: NAFLD is not a benign condition – that raised ALT requires action!
Resources
- RCGP liver disease toolkit – open-access and includes links to tools and calculators as well as additional e-learning resources
- British Society of Gastroenterology Guidelines on the management of abnormal liver blood tests
- NICE NG46: NAFLD assessment and management
- All Wales abnormal LFT pathway
Managing diabetes in the elderly and frail
Chris Cottrell
Diabetes Specialist Nurse, Swansea Bay University Health Board
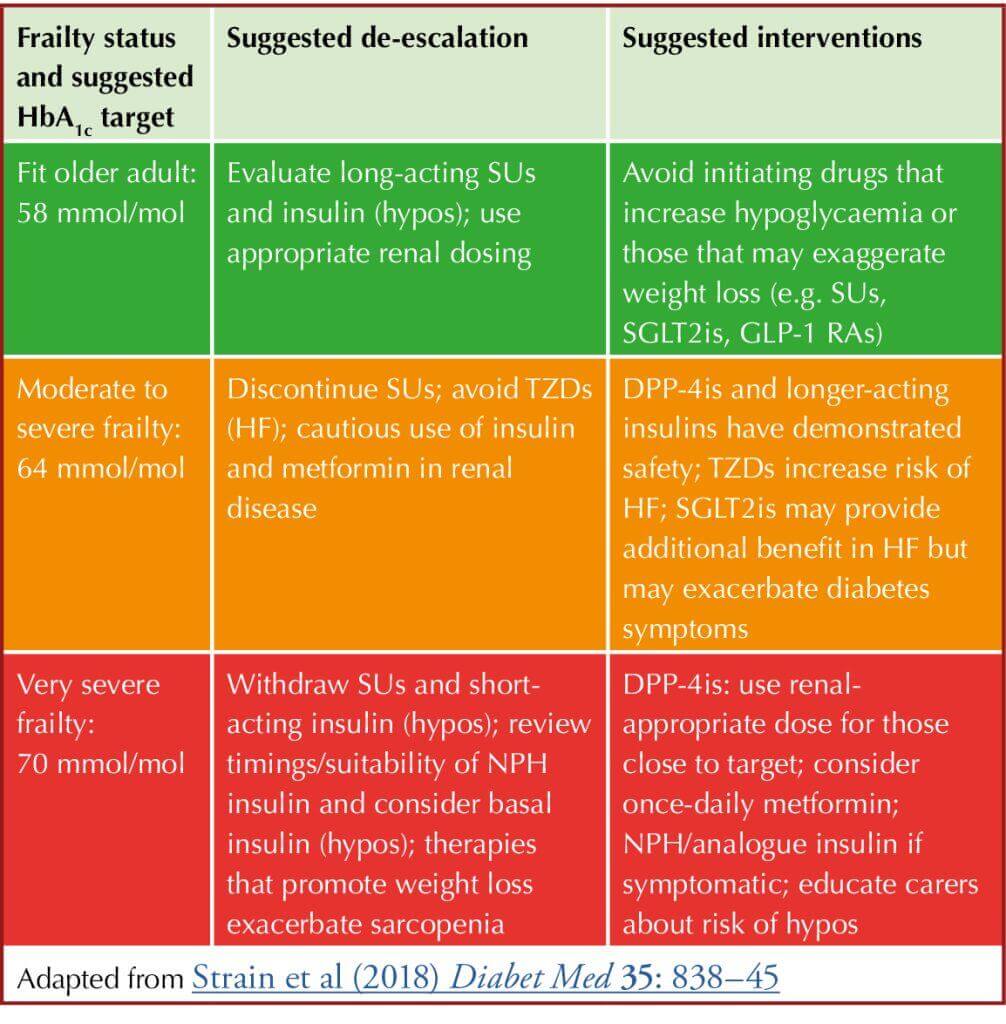
● Diabetes management in older adults is complicated by frailty, comorbidities and polypharmacy.
● Undertake a frailty assessment using a recommended tool, such as the electronic Frailty Index or Rockwood Scale, and use it to guide agreement of glycaemic targets.
● Frailty may be improved by simplifying, switching or stopping therapies to avoid hypoglycaemia, falls, hyperglycaemia, weight loss and sarcopenia.
● Consider de-escalation when appropriate – discuss with the person with diabetes and carers so everyone understands it is to ensure safety and improve quality of life, rather than “giving up” on providing care.
● Individualise glycaemic targets after discussion, depending on personal preferences, comorbidities, frailty, polypharmacy risks, likelihood of benefit or harm:
Resource
- National Advisory Panel on Care Home Diabetes Strategic document of diabetes care for care homes
Insulin in practice
Julie Lewis
Nurse Consultant, Primary Care Diabetes, Central Area, North Wales
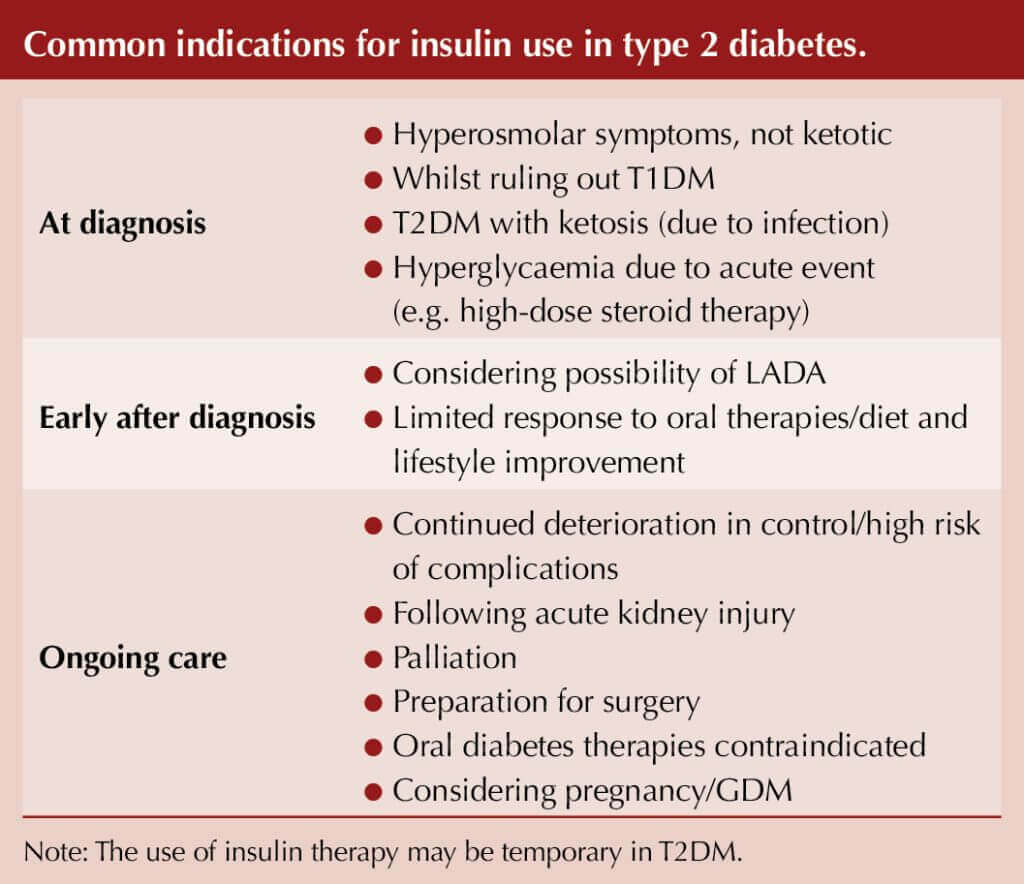
● A perception of mystery and art to insulin management exists in clinical practice that can create delays to initiating and adjusting this very effective treatment for type 2 diabetes.
● Matching the insulin profile to the person’s specific requirements is key to insulin being an effective therapy choice.
- Glucose targets need to reflect the needs of the individual.
- Consider the support that may be needed to administer and monitor this treatment.
● A thorough understanding of the person’s glucose profile will inform an appropriate insulin regimen choice.
- Self-monitoring of blood glucose (SMBG) is the standard approach to obtain glucose profiles. However, NICE NG28 now supports the use of flash glucose monitoring in certain type 2 diabetes situations.
● Continuing other glucose-lowering therapies: use the guidance to inform a safe and individualised approach:
- Sulfonylureas: Reduce by half or consider stopping. Can re-introduce if needed.
- Metformin: Continue if tolerated/eGFR permits.
- Other oral therapies/injectables: What benefit are they adding (e.g. renal/cardiovascular disease/weight management)?
- Review safety to continue and/or impact of discontinuation (concomitant use of therapies for other conditions; e.g. heart failure).
- Reinforce guidance (e.g. sick-day rules, hypoglycaemia recognition and treatment).
● Insulin initiation:
- Refer to British National Formulary for starting dose advice.
- A lower starting dose is acceptable provided there is active dose adjustment thereafter.
- Use a checklist to guide the process of initiation: confirms what has been covered and records important advice.
● Ongoing management/support:
- Utilise insulin education programmes whenever possible to improve self-management competence.
- Insulin dose adjustment is a fundamental factor to assure insulin effectiveness. This cannot be completed safely without glucose data.





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025