In the previous issue of the Journal, I provided an overview of the conventional dietary advice currently offered to people with type 2 diabetes and suggested that basing meals around starchy carbohydrate foods – albeit the “healthy” wholegrain variety – may not be the best approach (Diggle, 2019). This article seeks to improve our understanding of carbohydrates in the diet, how they affect us and, importantly, the impact they can have in those with type 2 diabetes. It also provides a practical approach that I have found to be successful for people with type 2 diabetes.
Raising carbohydrate awareness
There are different forms of carbohydrates that interact with the body in different ways. As healthcare professionals, we need to understand this before we can help those with diabetes to make informed decisions about the food they eat.
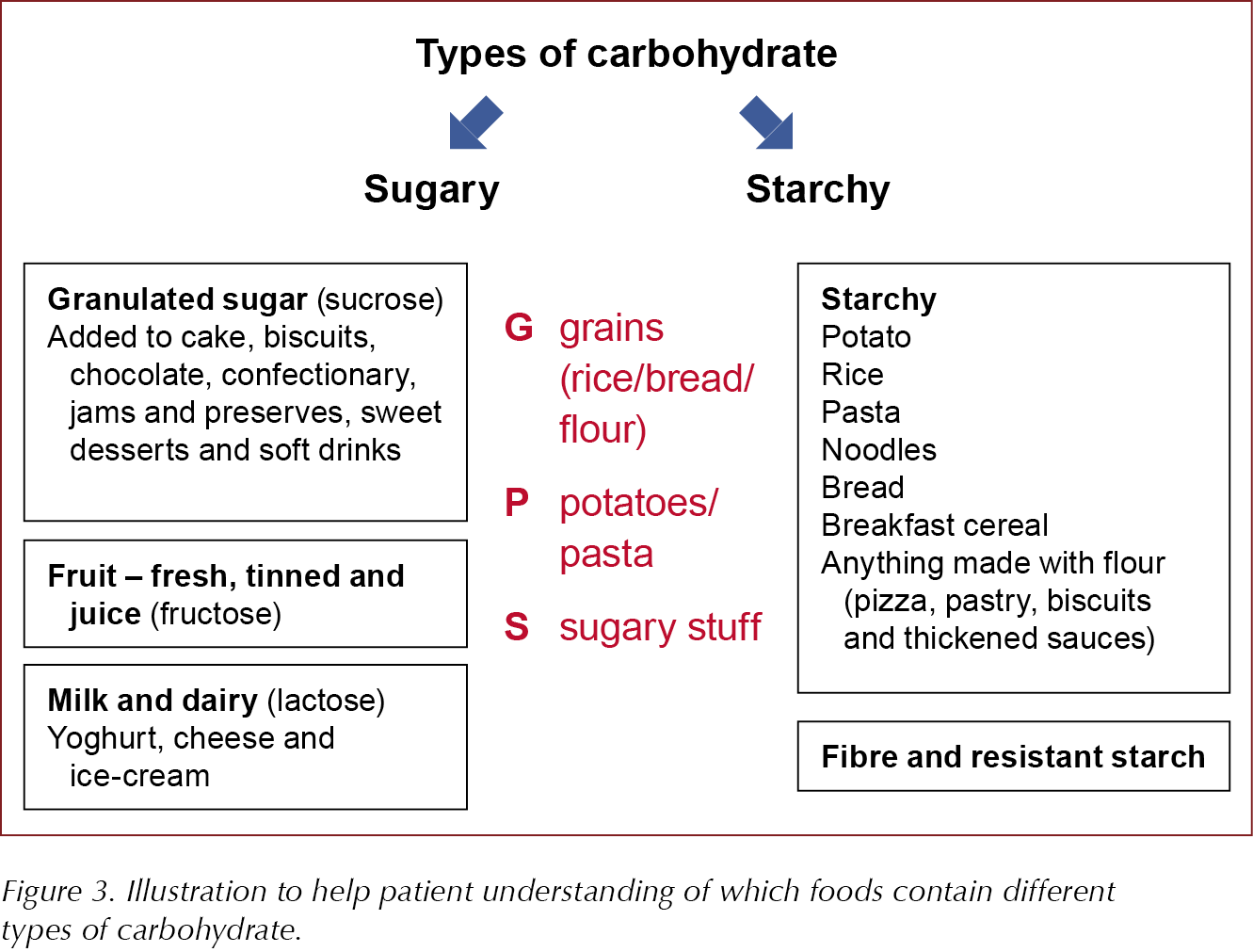
Carbohydrates are found in a wide variety of foods, which tend to be categorised as follows:
- Starchy foods, such as bread, pasta, potatoes, cereals, rice and couscous.
- Sugary foods, which can be subdivided into those containing:
- – Natural sugars, such as whole fruits (fructose), milk and milk products (lactose).
- – Free sugars, which are added to sweets, chocolate, sugary beverages and desserts, but also occur naturally in fruit juices, fruit concentrates, syrups and honey.
- Fibre-containing foods. There are two types of fibre:
- Insoluble fibre found in wholemeal bread, brown rice and wholegrain cereals (beneficial for digestive health).
- Soluble fibre found in fruit and vegetables, pulses, oats and barley (may help to reduce cholesterol levels and slow the breakdown of carbohydrates to glucose).
The World Health Organization (WHO, 2015) strongly recommends that, in both adults and children, the intake of free sugars (i.e. all monosaccharides and disaccharides added to foods by the manufacturer, cook or consumer, plus sugars naturally present in honey, syrups, and fruit juices) be reduced to <10% of total calorie intake (about 12 tsp/day) and calls for a further reduction to <5% (about 6 tsp/day), if possible.
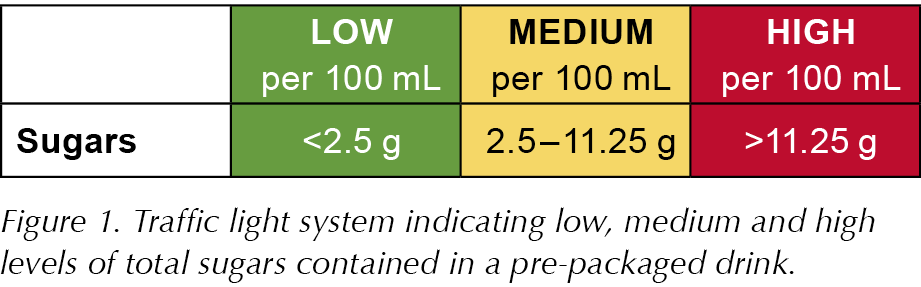
The traffic light system on food labels can help consumers to identify the sugar content (Figure 1). However, caution must be exercised. The branding and naming of several commercial smoothies, for example, imply that they are healthy options but, in the unit volumes typically sold, they can contain the equivalent of 10 cubes (>50 g) of sugar per portion.
Not all carbohydrates are the same
Different carbohydrate sources are digested and absorbed at different rates. The glycaemic index (GI) is a measure of how quickly certain foods raise blood glucose levels compared to glucose, which has a value of 100. Sweet, sugary foods have a higher GI than starchy foods and individuals with diabetes may opt for lower GI foods. However, meta-analyses have reported that low-GI diets are not effective in promoting weight loss in people with diabetes, although they can improve glycaemic control (Thomas and Elliott, 2010; Brand-Miller et al, 2012). An important factor to consider is that, despite having a lower GI, a large portion of starchy carbohydrate can also lead to a significant rise in blood glucose levels.
Another measure, glycaemic load (GL), takes account of portion size as well as GI (by multiplying the carbohydrate content in grams by the GI and dividing by 100). So, one tablespoon of honey has a high GI of 87 but a GL of only 3, whereas a cup of dried apricots has a low GI of 23 but a high GL of 23. GI and GL values are commonly interpreted as indicated in Figure 2.
Food processing and cooking methods may also alter the impact on blood glucose levels. Most people assume that wholemeal bread will have much less impact on blood glucose levels than white bread. In terms of total carbohydrate content, it is much the same at around 14 g per slice. Seeded varieties with more fibre should slow down carbohydrate absorption, but sugar is sometimes added to counteract the bitterness of the wholegrain.
In 2018, the BBC broadcast The Truth About Carbs, a documentary that investigated how different types of carbohydrate may be impacting our health. The information was delivered in an entertaining way and, while there may have been some inaccuracies (Williams, 2018), it included a lot of interesting and practical information on carbohydrates and their effects on the body (including that freezing bread before toasting it converts some of the starch into “resistant starch”, which is indigestible and therefore reduces the GI).
What constitutes a healthy diet is one of the most vehemently argued topics of our time. As scientists, nutritionists, academics, researchers and journalists battle it out, I suspect that most healthcare professionals are left feeling confused about the advice they should be offering.
We may be waiting a long time before national guidelines change, but I was interested to see Zoë Harcombe invited to speak at an All-Party Parliamentary Group for Diabetes meeting in February this year. In her 10-minute presentation, entitled The Science of Reversing Type 2 Diabetes with Low Carbohydrates, she gave a very powerful critique of the high-carb, low-fat advice that underpins national guidance on healthy eating (see Diggle, 2019). Highlighting the nutritional deficiencies of the Eatwell Guide and its bias for carbohydrate, she questioned why members of the processed food industry dominated the advisory panel setting the guidelines and called for a Government strategy that supports low-carb and low-calorie dietary advice.
It will be interesting to see how things pan out. As practising clinicians, we can adopt an approach that does not dictate what people should eat, but does provide more logical information and advice than that depicted in the Eatwell Guide. Below I have highlighted some of the key issues that I cover in consultations with people interested in addressing their weight, and summarised the main messages in Box 1.
A different approach in practice
If they want to lose weight, people often focus on the fats they eat and do not appreciate that excess consumption of carbohydrate can lead to fat accumulation and, for some individuals, increasing insulin resistance and, ultimately, type 2 diabetes (see explanations of Roy Taylor’s twin-cycle hypothesis and Jason Fung’s fridge–freezer analogy in Part 1 [Diggle, 2019]).
When discussing diet with patients, I often begin by explaining what happens to the food we eat, particularly how carbohydrates are converted to glucose before entering the bloodstream, stimulating the secretion of insulin. The insulin helps to move the glucose into the cells to produce energy, but any excess is stored as glycogen in the liver and muscles or, if those stores are full, converted to fat. I use the images in Appendix 1 to explain this process.
Calorie intake is important, but consideration of the amount and type of carbohydrate being consumed is essential for optimal glycaemic control and weight management. People often underestimate the total amount of carbohydrate they eat. It is always worth checking that an individual is clear about what we mean when we talk about carbohydrates. It may help to provide food examples categorised into the different types of carbohydrate, as shown in Figure 3.
Individuals will often gain much better carbohydrate awareness by keeping a food diary and counting their calorie and carbohydrate intake over several days.
Carbs & Cals provides some excellent resources to support this activity, including an app. To support this learning, I have created a library of books that I loan to patients, though many have invested in their own copies.
I find it useful to give an example of the calorie and carbohydrate intake for a seemingly healthy eating day that actually provides a total carbohydrate intake of 345 g – far in excess of the maximum recommended reference intake. I then compare it to a lower carbohydrate menu suggestion, as illustrated in Appendix 2.
This provides an opportunity not just to identify foods with high carbohydrate content, but also to look at “food swaps” (e.g. replacing rice with cauliflower “rice”). I avoid suggesting they eat more of anything, even the healthy stuff, but instead focus on replacing unhealthy options with healthier ones.
Having explained how to calculate carbohydrate intake, it often helps to agree a total carbohydrate and total energy intake target to work towards – this is likely to vary between individuals.
The notion of eating little and often seems to prevail and is another myth I try to dispel. Low-calorie diets, intermittent fasting and time-restricted eating (TRE) are becoming increasingly popular (Mosley, 2015; 2019; Fung, 2018) and are strategies that people with type 2 diabetes may wish to pursue. However, it should be stressed that a careful review of medication is essential before embarking on such a diet, as adjustments may be required. It may be necessary to reduce doses, change regimens or drugs, or even stop certain medications. Particular caution should be exercised for those taking blood glucose-lowering medications that are associated with an increased risk of hypoglycaemia, such as sulfonylureas or insulin.
Sharing practical tips for those wishing to fast, such as keeping well hydrated, compensating for low salt intake (which can lead to dizziness and headaches) by having a cup or two of bone broth (with a pinch of sea salt added) and increasing intake of fibre (e.g. with green, leafy vegetables) on non-fasting days to help with constipation, is also useful.
I generally encourage a Mediterranean style of eating: reducing refined, simple and starchy carbohydrates (including pasta, bread, white rice and starchy vegetables, such as potatoes) and most breakfast cereals; limiting fruit juices; avoiding sweet drinks and smoothies; reducing fruit intake to 2–3 portions per day; moderately increasing intake of healthy fats (including more olive oil, rapeseed oil, nuts, avocado, eggs and some full-fat dairy products), whilst avoiding trans and processed fats; and including plenty vegetables, oily fish and occasional meat.
Finally, we cannot ignore the emotional, psychological and social factors that are irrevocably entwined with what, why and when we eat. People may have quite complex relationships with food. We might eat because we feel happy or because we are sad, to socialise or when we are lonely or bored. We cannot successfully tackle diet without also addressing the psychosocial elements of eating. It is beyond the scope of this article to discuss this, but I encourage you to look at a series of articles by Dr Jen Bateman (née Nash) published in the Journal of Diabetes Nursing that explore the non-hunger reasons for eating and how to tackle them effectively, or to visit www.EatingBlueprint.com.
Conclusion
There may be insufficient evidence to support any specific dietary intervention for people with type 2 diabetes, but I encourage you to challenge some of the deep-rooted beliefs you hold about diets and healthy eating, and to consider whether directing people to the Eatwell Guide and telling them to base their meals around starchy carbohydrates is a logical approach. Most of all, believe that people do want to make their lives better. Perhaps the reason so many people fail to improve their diabetes control or achieve (and maintain) weight loss with lifestyle changes is because the advice they are given is flawed and not because they lack the will to make changes.








Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025