What are calcium channel blockers?
Calcium channel blockers (CCBs) are medications that subdivide into two categories based on their molecular structure:
● Dihydropyridine (DHP) CCBs are used to treat hypertension and for prophylaxis of chronic stable angina. Examples include amlodipine, felodipine, lacidipine, lercanidipine, nicardipine, nifedipine and nimodipine.
● Non-DHP CCBs, otherwise known as rate-limiting CCBs, can also be used to treat hypertension and angina, but additionally are effective in managing supraventricular tachycardias. There are two non-DHP CCBs: diltiazem and verapamil.
CCBs are well absorbed orally and, as lipophilic molecules, are highly protein-bound in the circulation. Metabolism occurs principally in the liver via the CYP3A4 enzyme, and hepatic first-pass metabolism can be extensive. Following metabolism, elimination is via the kidneys.1
Mechanisms of action2,3
● When calcium ions (Ca2+) gain entry to a cell, they bind to intracellular calcium-binding proteins, namely troponin and calmodulin in cardiac and smooth muscle respectively, to initiate muscle contraction.
● CCBs inhibit the inward flow of Ca2+ through ion channels located in the cell membrane.
● By lowering intracellular Ca2+ concentrations, CCBs induce smooth muscle relaxation and, hence, peripheral vasodilation and a reduction in blood pressure (BP).
● In myocardial cells, the consequence of lower Ca2+ concentration is reduced activity at the sinoatrial and atrioventricular nodes, allowing treatment of supraventricular tachycardias with non-DHP CCBs.
- Reduced activity of cardiac myocytes leads to decreased cardiac contractility, reducing oxygen demands of the heart.
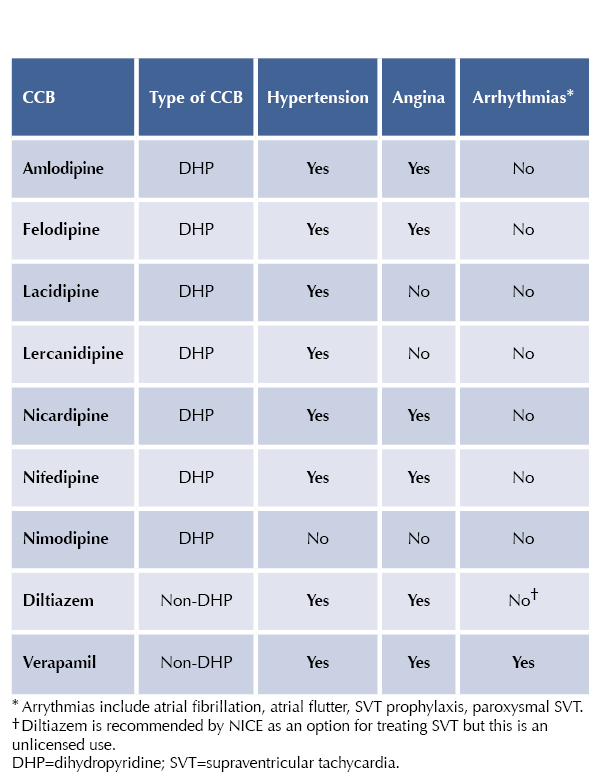
Licensed indications of CCBs for hypertension, chronic stable angina and supraventricular tachycardia4
Other uses
● Nimodipine is licensed for intravenous use in the treatment of ischaemic neurological defects following aneurysmal subarachnoid haemorrhage, and for oral use in prevention of the same.
● Nicardipine is licensed as an intravenous infusion for life-threatening hypertension, including in pregnancy (pre-eclampsia) and for postoperative hypertension.
● Nifedipine immediate-release is licensed for treatment of Raynaud’s syndrome and hiccup in palliative care; an unlicensed use is postponement of premature labour. Avoid using for hypertension and angina.
- By reducing pulmonary artery pressure, immediate-release nifedipine can be used to treat pulmonary hypertension and high altitude pulmonary oedema (unlicensed).
● Further licensed uses of verapamil are: prophylaxis after myocardial infarction where beta-blockers not appropriate, and prophylaxis of cluster headache (initiated under specialist supervision).
● Treatment of chronic anal fissure can be treated topically with 0.2–0.5% nifedipine ointment or 2% diltiazem cream or ointment for up to 8 weeks. Oral nifedipine and diltiazem are unlicensed treatments for anal fissure.
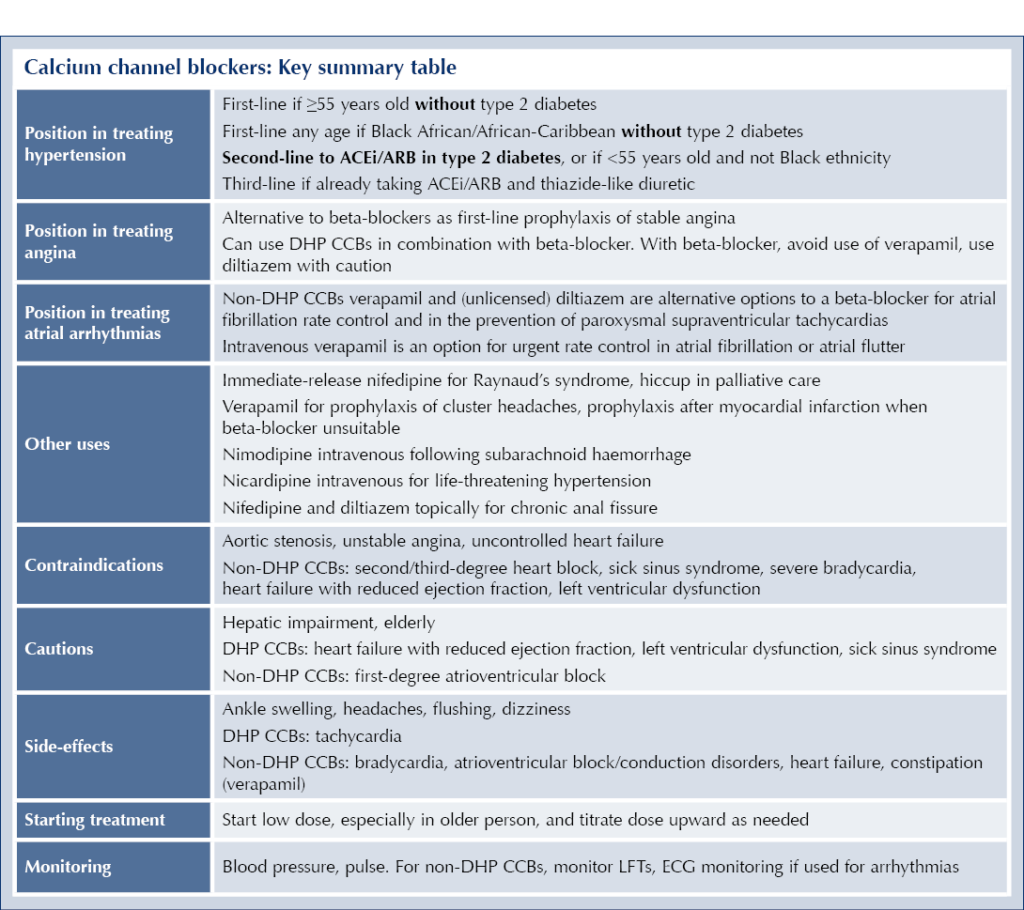
Positioning in guidelines
Hypertension
First line: NICE NG136 recommends CCBs as first-line treatment for hypertension in adults who do not have type 2 diabetes and:5
- are age 55 or over, or
- are of Black African or African-Caribbean family origin, of any age.
A thiazide-like diuretic should be used in preference to a CCB if there is evidence of heart failure or a CCB is poorly tolerated.
Second line: CCBs (or thiazide-like diuretics) are second-line antihypertensive treatments (after an ACE inhibitor or ARB) in people with type 2 diabetes, and in those without type 2 diabetes who are less than 55 years of age and not of Black African or African-Caribbean family origin). CCBs are also a second-line option for hypertension in people with type 1 diabetes (in whom ACEi/ARBs are also recommended first-line.6
Third line: If an individual is taking dual therapy with a RAAS blocker and a thiazide-like diuretic and hypertension remains uncontrolled, a CCB is recommended as third-line therapy.5
Angina
● NICE CG126 recommends a CCB or beta-blocker as first-line regular treatment for stable angina, with the choice made according to comorbidities, contraindications and the person’s preference.7
● If beta-blocker monotherapy does not satisfactorily control angina symptoms, a CCB can be substituted or added.
- If a CCB is used in combination with a beta-blocker, choose a DHP CCB. As rate-limiting CCBs, verapamil especially and diltiazem to a lesser extent could precipitate severe bradycardia and heart failure if used with a beta-blocker.
Arrhythmias8
● Intravenous verapamil is an option for urgent rate control in acute onset of atrial fibrillation or atrial flutter, if cardioversion is not appropriate and if an intravenous beta-blocker is unsuitable. Avoid verapamil if left ventricular ejection fraction is <40% or if acute heart failure is suspected.
● Oral verapamil or diltiazem (unlicensed use) are alternative options to a beta-blocker for rate control of atrial fibrillation that is not of new onset or which has a reversible cause (and less commonly as an adjunctive treatment for atrial flutter).
- Diltiazem can be used in combination with a beta-blocker or digoxin if necessary to achieve the target rate control.
● Verapamil and diltiazem can be used to prevent recurrent episodes of paroxysmal supraventricular tachycardia.
● Where urgent treatment of supraventricular tachycardia is necessary, intravenous verapamil can be used if intravenous adenosine is ineffective or contraindicated.
Principal effects
● BP reduction: typically by 9.5–13.2 mmHg systolic and 5.9–8.5 mmHg diastolic, with consistent reductions through a 24-hour period.9
- CCBs appear to be more effective as monotherapy than other classes of antihypertensive agent (e.g. ACE inhibitors) in Black people compared with other ethnicities.3,10
- When used in combination with other antihypertensive agents, CCBs work synergistically, generating a greater antihypertensive effect than the maximal dose of one drug.11
- DHP CCBs are preferred over non-DHP varieties for treatment of hypertension, as they have the most evidence from clinical trials.12
● Cardiovascular benefits: through their antihypertensive effects, CCBs reduce the risk of major cardiovascular events, heart failure and all-cause mortality.13
- Superior to other antihypertensives for preventing stroke.14
- Inferior to other antihypertensives for preventing heart failure.14
- DHP CCBs are particularly effective in reducing cardiovascular events in the elderly and those with isolated systolic hypertension.15
- DHP CCBs have been shown to reduce cardiovascular events in people with diabetes,16 and so are a good second-line option to RAAS-based drugs for treating hypertension.
● Nimodipine has a unique preferential vasodilatory effect on cerebral arteries; thus, its use is confined to preventing and treating vascular spasm following aneurysmal subarachnoid haemorrhage.4
● The non-DHP CCBs act preferentially on myocardial cells rather than by peripheral vasodilation. They reduce cardiac oxygen demand, allowing treatment of angina, and inhibit atrioventricular node activity, allowing treatment and prevention of supraventricular tachycardias.3
- Verapamil has more powerful cardiac effects than diltiazem.
● Both DHP-CCBs and diltiazem are effective (first-line) treatments for vasospastic (Prinzmetal) angina, by relieving coronary vasospasm.3,17
● CCBs are an effective add-on treatment to RAAS blockers for managing albuminuria.18
Contraindications, cautions and drug interactions4
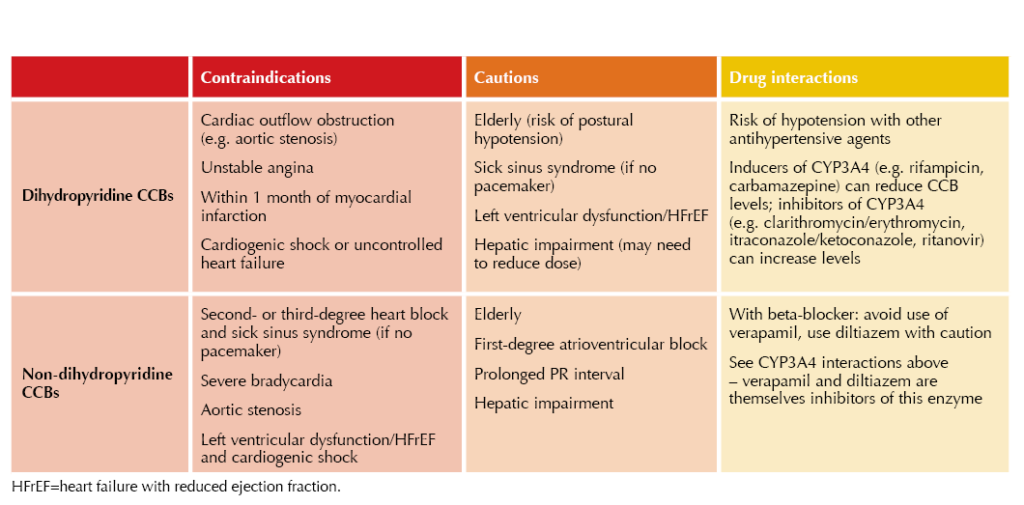
● If a CCB is needed in individuals with stable heart failure, amlodipine is the drug of choice.19
● For those who have left ventricular dysfunction/heart failure post-myocardial infarction, CCBs should generally be avoided except amlodipine.4
● In people with heart failure with preserved ejection fraction, DHP CCBs, notably amlodipine, can be used.
Prescribing in pregnancy
In general, CCBs should be avoided if possible in pregnancy and breastfeeding unless benefits are judged to outweigh risks. Nifedipine is considered a safe option in pregnancy if labetalol is unsuitable, or in combination with labetalol if necessary, with methyldopa as a further option. Check to see which brands of nifedipine are indicated for use in pregnancy. Nifedipine and amlodipine, if previously used to control BP, can be used in the postnatal period.20
● In women with chronic hypertension, the choice of antihypertensive medication should ideally be optimised pre-conception, switching, if necessary, from ACEi/ARBs and thiazide-like diuretics, which could predispose to congenital abnormalities, to labetalol and nifedipine.
Adverse effects
DHP CCBs
Common side-effects, most of which are the result of vasodilation, include:
- Peripheral oedema – ankle swelling.
- Headache.
- Flushing.
- Dizziness – postural hypotension.
- Palpitations – tachycardia.
- Nausea and gastrointestinal reflux (relaxation of oesophageal sphincter smooth muscle).
Peripheral oedema, and other side-effects, are more likely to occur with higher doses. Strategies to reduce CCB-induced ankle swelling include:18
- Reduce the dose of DHP CCB.
- Switch to a more lipophilic DHP CCB (e.g. lercanidipine, lacidipine).
- Switch to a non-DHP CCB.
- Employ combination antihypertensive therapy – diuretic therapy or ACEi/ARB (shown to reduce peripheral oedema in combination with CCB).21
Non-DHP CCBs
The previous vasodilatory side-effects are typically less marked with non-DHP CCBs. Bradycardia occurs rather than tachycardia and this, together with the drugs’ negative inotropic action, can lead to hypotension and dizziness. Other adverse effects include:
- Constipation – especially with verapamil.
- Atrioventricular block, conduction disorders (e.g. QT prolongation).
- Heart failure.
- Rashes – erythema multiforme, Stevens–Johnson syndrome (severe).
Dosing schedules and formulations4
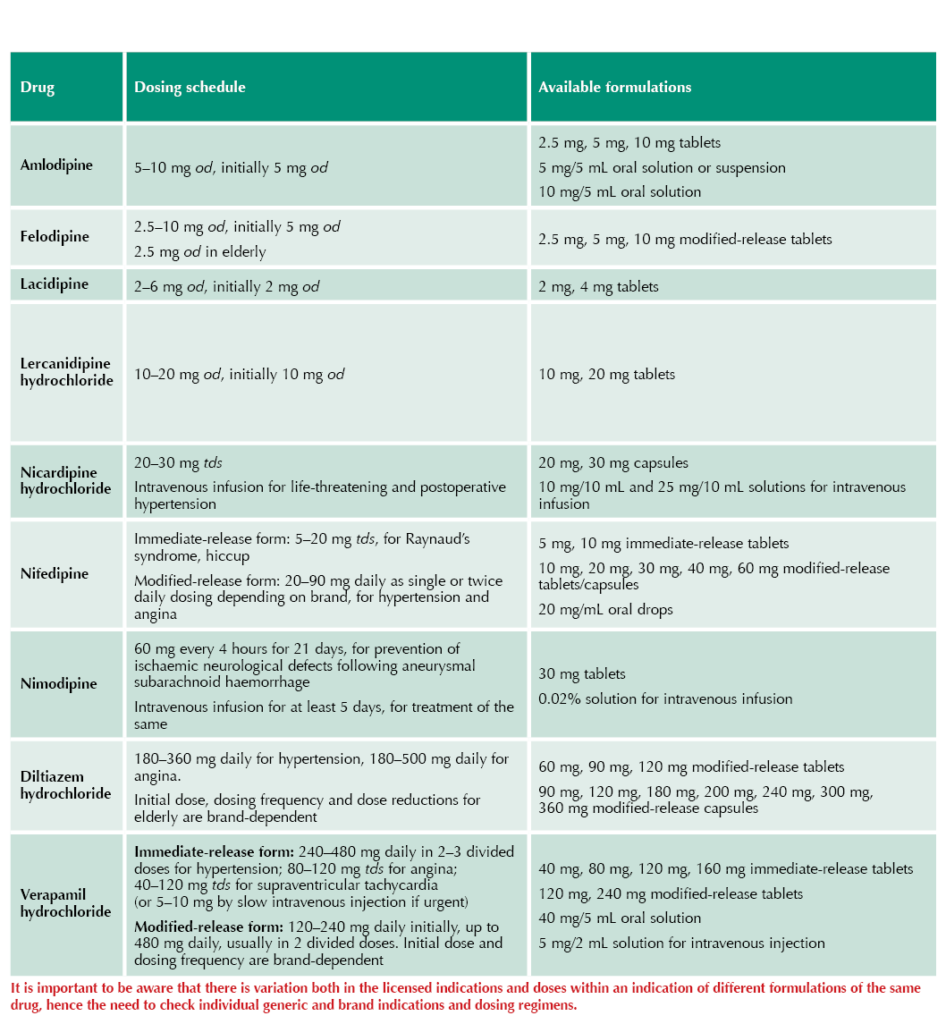
CCBs in combined preparations
- Amlodipine + valsartan
- Amlodipine + olmesartan
- Amlodipine + olmesartan + hydrochlorothiazide
- Amlodipine + perindopril erbumine
- Felodipine + ramipril
Initiating and monitoring1
● Generally start CCBs at low dose, especially in the older person, and titrate upwards as required, monitoring for side-effects.
● Check BP and pulse before starting a CCB, and monitor after initiation.
● Response of BP or symptoms of angina will inform on efficacy.
● In the case of verapamil and diltiazem, LFTs should be monitored. When they are used for treating arrhythmias, ECG monitoring is appropriate.
Prescribing tips
● When prescribing modified-release preparations of CCBs, specify the brand. Different brands may generate different clinical responses.
● Be aware that withdrawal of a CCB may worsen or unmask myocardial ischaemia.
● Avoid use of beta-blockers with verapamil and use them cautiously with diltiazem. There is a risk of severe bradycardia and triggering of heart failure.
● If eGFR is <30 mL/min/1.73 m2, check recommendations for specific drugs (and brands).
● Consider dose reduction of CCB for people with hepatic impairment.
● In general, choose a long-acting DHP CCB such as amlodipine for hypertension, and also for angina if a beta-blocker is being used. For angina not treated with a beta-blocker, a non-DHP CCB is appropriate.
● Immediate-release nifedipine is not recommended for treating hypertension and angina because it can cause a rapid fall in BP (rather than a sustained reduction) with reflex tachycardia – hypotension and myocardial ischaemia may result.
Calcium channel blockers: Key summary table





3-point MACE occurred in 12.2% vs 13.1% of tirzepatide and dulaglutide recipients, respectively, confirming non-inferiority.
19 Jan 2026