The National Diabetes Audit (NDA) is one of the largest annual clinical audits in the world. It measures the effectiveness of diabetes healthcare in England and Wales against NICE Clinical Guidelines and Quality Standards. Through the collection and analysis of data, it aims to drive improvements in the outcomes for adults with diabetes receiving care from primary, secondary and community providers.
What is new in the National Diabetes Audit?
1. Addition of prescribing data
Prescribing data is being added to the National Diabetes Audit (NDA) at an individual patient level for the 2017–18 audit. This enables the NDA to align with the NICE guidance on type 1 diabetes in adults (NG17; NICE, 2015a) and type 2 diabetes in adults (NG28; NICE, 2015b), which recommend statin prescribing rather than getting to below a specific total cholesterol level.
So, in the 2017–18 report, the metric will be the proportion of patients aged 35–80 years with no history of cardiovascular disease (CVD; angina, myocardial infarction, heart failure or stroke) prescribed a statin. A further secondary prevention metric will capture the proportion of patients with diabetes and documented CVD prescribed a statin.
The NDA has, since its start in 2004, reported on the proportion of patients with diabetes with a total cholesterol level below 5 mmol/L and below 4 mmol/L. These will continue to be reported for continuity and to enable comparisons with previous years.
The addition of prescribing data will, within a few years, enable the NDA to become a very important source of prescribing safety data that will be of worldwide significance.
2. Data extraction is now via the GP Extraction Service
Data for the NDA is now being extracted from GP clinical computer systems via the GP Extraction Service (GPES), which is the way Quality Outcomes Framework (QOF) data has been extracted for many years. It means that extraction is automatic and requires virtually no work by the practice. This should be a big improvement over previous years when participation in the NDA for those with certain clinical computer systems was more complicated and often took up to an hour to achieve.
Data on care processes and treatment targets at practice and Clinical Commissioning Group (CCG) level for the year ending 31 March are now published in a more timely manner in the autumn of the year of collection.
3. Practice participation has increased
Practice participation under the previous extraction mechanism reached a peak of 87.9% in 2011–12. It then dipped significantly to 70.7% in 2012–13, and 57% in 2013–14 and 2014–15. We think this was due largely to the reorganisation of the NHS from Primary Care Trusts to CCGs, and the loss of support staff who encouraged and supported practices in submitting data to the NDA.
Participation increased to 82.4% in 2015–16 and to 95.3% in 2016–17. The NDA primary care collection now forms part of the agreed GP contract, so even higher participation levels in the future may be anticipated.
4. Data will be collected quarterly for 2018–19
This will occur in August and November 2018, and February and May 2019. This allows more timely feedback on progress towards end-of-year care processes and treatment targets to aid service planning and quality improvement activities.
The data will be published quarterly at practice and CCG level. A national report will continue to be published annually.
5. Data for the Diabetes Prevention Programme is now being collected in the NDA
Information on people “at risk of developing diabetes”, their referral to the Diabetes Prevention Programme (DPP) and the outcomes from attending the programme are now being collected. This will enable the success of the programme to be evaluated through the assessment of long-term complication development and, eventually, mortality.
What do the results of the latest NDA report show?
The latest published data is from the 2016–17 audit year, collected in the spring of 2017. Data on care process and treatment target achievement were published in late 2017 as a short report at practice and CCG level. The national report was published on 8 March 2018. This delay occurs because the national report has to have sign-off from NHS England.
The complications and mortality report for the 2016–17 audit year has a planned publication date of summer 2019.
Key findings from the NDA core audit report 1 for 2016–2017
Variation
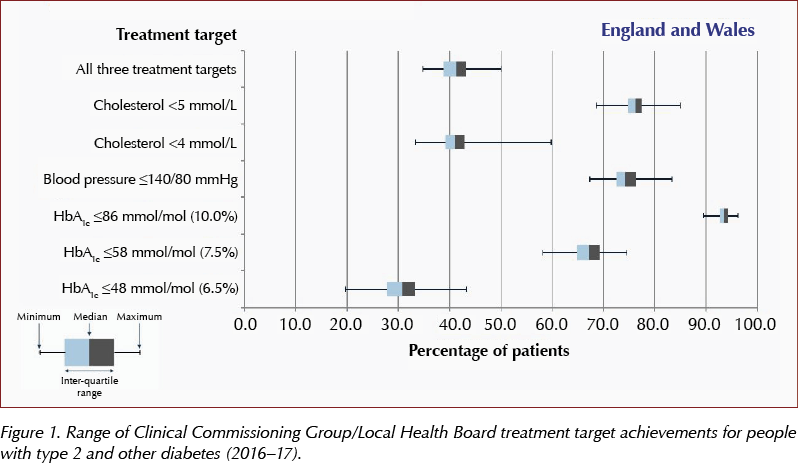
The NDA continues to show marked variation in both care process completion and achievement of treatment targets (HbA1c at or below 58 mmol/mol [7.5%]; blood pressure (BP) at or below 140/80 mmHg; and cholesterol below 5 mmol/L) between CCGs and between practices within high and low achieving CCGs. If poorly performing CCGs and poorly performing practices improved towards the mean, there is the opportunity of significant improvements overall. Figure 1 provides an indication of the overall picture across England and Wales.
Annual care processes
Foot surveillance and urine albumin care process checks are completed less frequently than other checks in all types of diabetes. The lower levels of BMI recording that started in 2013–14 are unaltered.
Achievement of treatment targets
There has been a greater than 10% improvement in HbA1c target achievement for type 1 diabetes and a 10% improvement of the BP target in people with type 2 diabetes over the 6-year period from 2011–12 to 2016–17. However, people of working age and younger are almost half as likely to achieve treatment targets as their older counterparts.
Structured education
The percentage of people being recorded as being offered structured education has risen from 18.4% in 2011–12 to 77% in 2016–17. However, recording of attendance on a course is less than 10%, which is thought to be an underestimate. Ways of getting more information on attendance rates from those providing group education courses into GP clinical computing systems are being explored.
Severe mental illness and learning disability
There are some small differences from the general population of people with diabetes in care process completion by those who, as well as having diabetes, have been recorded as having severe mental illness (SMI) or learning disability (LD). However, those with diabetes and SMI or LD are equally likely to achieve their treatment targets as those in the general population of people with diabetes. This is counter to what was thought, and shows that people with LD and SMI are having their physical health assessed and monitored.
Conclusion
Changes to the NDA have resulted in increased participation. The addition of prescribing information will be a huge potential benefit, and will allow us to understand how different glycaemic-lowering agents, statins and BP-lowering agents affect treatment target achievement, complication rates and mortality. The NDA is also now set up to record the outcomes of the DPP.
In the next 5–10 years, the NDA should reach its full potential and be able to answer many pressing questions for the diabetes community worldwide.
Further information:
National Diabetes Audit:
http://bit.ly/2JJrKnr
National Diabetes Audit Report 1 – Findings and recommendations 2016–17:
http://bit.ly/2Lpm6fd





Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025