Cardiovascular disease (CVD) is a leading cause of mortality worldwide, representing over 30% of all global deaths (NICE, 2023). CVD refers to atherosclerosis of arterial vessel walls as well as thrombosis, and thus includes coronary artery disease, ischaemic stroke and peripheral arterial disease. Risk factors include those that are modifiable, including type 2 diabetes, hypertension, dyslipidaemia, smoking, diet and physical activity, as well as non-modifiable risks such as being male and increasing age (Shah et al, 2015; NICE, 2023). Hypertension can increase the risk of ischaemic heart disease, stroke and chronic renal disease. It is important to detect hypertension because it is often asymptomatic. CVD and hypertension are common comorbidities in those living with type 2 diabetes (Ali et al, 2019; Mach et al, 2020).
The NHS Diabetes Eye Screening Programme (DESP) invites people living with diabetes who are 12 years old or over for eye screening. The aim of the programme is to reduce the risk of sight loss in people with diabetes by screening for diabetic retinopathy (NICE, 2023). If no retinopathy is detected for two tests, patients are invited to be screened every 2 years; otherwise, screening is performed at more regular intervals.
Cardiovascular disease, of which hypertension is the greatest risk factor, is the largest cause of the life expectancy gap between the least and most deprived quintiles in Sussex. There are approximately 293 000 people included in practice hypertension registers across Sussex, and prevalence is rising across all age groups. The current prevalence is 15.9% among a population of approximately 1.8 million. The proportion of people with hypertension who were managed to target in 2023/2024 (excluding personalised care adjustments and exception reporting) was 68.6%, an increase from previous years but short of the national ambition to achieve 80% of patients treated to target.
We therefore created an innovative pathway whereby patients attending their DESP appointments were offered an opportunistic blood pressure check.
Methods
Participants
Eligible adult patients were those attending appointments for diabetes eye screening. Consecutive attendees to the DESP clinics were offered opportunistic blood pressure monitoring. The majority of patients were willing to participate in the pathway.
Procedure
If a normal blood pressure was recorded, the participant was given lifestyle advice on diet and exercise in relation to diabetes and/or hypertension, and their GP was informed in writing of the results.
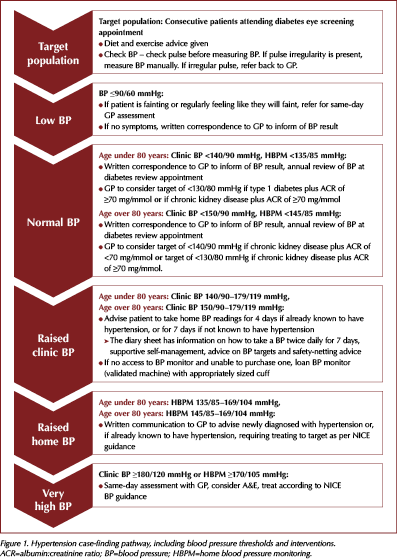
If a raised blood pressure reading was recorded, depending on the thresholds recorded as per the flowchart in Figure 1, the individual was advised to take home blood pressure monitoring (HBPM) readings. Detailed instructions were given to participants on how to monitor their blood pressure at home, and on how and where to escalate concerns. Participants were advised on blood pressure thresholds and were given safety-netting advice about low or very high readings. At any point, if a participant opted out of the pathway once enrolled, their GP was informed.
The project team took responsibility for reviewing blood pressure readings and was the point of contact for participants’ queries or concerns. If hypertension was newly diagnosed or it was demonstrated that a participant with known hypertension was not being treated to target, the participant’s care was referred to their GP practice for review and medication advice. Written communication was sent to the participants’ registered GP once verbal advice was given. During the project, participants were followed up to ensure that relevant actions, such as treatment to target, had taken place. Participant feedback was also sought.
The pathway was aligned with the principles of personalised care, including shared decision making and supported self-management. Our local Standard Operating Procedures included:
- Patient pathway.
- Process for collecting blood pressure measurements.
- Responsibility for following up on blood pressure measurements.
- Interface with primary care.
It is estimated that 30–40% of people with a diagnosis of hypertension have access to an HBPM device (Hodgkinson et al, 2020). Validated monitors can be confirmed against the list published by the British and Irish Hypertension Society (2024). Where monitors were loaned to participants, there was a register for stock management, return, cleaning and re-use.
Blood pressure targets were as per NICE guidance, and targets were individualised where clinically appropriate. Participants were counselled on this; for example, they were told that if they recorded consecutive readings above 170/115 mmHg, they should contact their GP for urgent same-day advice. The frequency of blood pressure monitoring was person-specific, with 4 days or 7 days of readings being requested as appropriate.
All blood pressure readings were submitted to the project team. Due to different IT platforms being employed locally, participants were encouraged to submit their HBPM readings via email or via a paper diary. Participants were advised on self-monitoring apps, which offered an alternative to keeping a paper diary as well as supporting longer term self-management. These apps are patient-held and do not automatically share readings with healthcare teams; however, many will allow the patient to download a report for emailing to their healthcare team.
Results
Key outcomes of this study are summarised in Figure 2. Consecutive attendees to the DESP clinics were offered opportunistic BP monitoring. In total, 200 people participated in the study. Of these, 91 (45.5%) had clinic blood pressure readings above 140/90 mmHg.
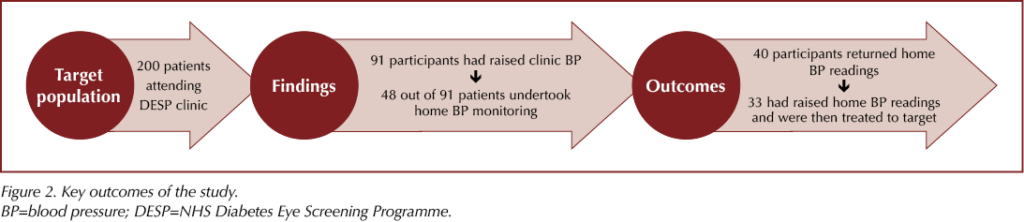
Forty-eight of these 91 individuals agreed to undertake HBPM (53.3%). Of those, 40 participants (83.3%) returned their results, with some requiring reminders to do so. Thirty-three participants had elevated home BP readings, of whom 13 received a new diagnosis of hypertension and 20 were already diagnosed but required treatment to target.
All 33 participants with elevated home blood pressure readings were contacted to ensure that they had been followed up by their GP practice; this was found to be the case for all.
Results for eight participants remain pending as no contact was received following telephone reminders. The non-respondents were aged 50–64 years and comprised four male and four female participants.
Of the 91 participants with raised clinic blood pressure readings, 43 (47.3%) declined further intervention. Of these 43 participants, 23 already had follow-up planned with primary care and five had follow-up planned with secondary care under cardiology or renal teams. Three participants were unable to take home blood pressure readings and one was leaving the country. Eleven declined all follow-up; two stated that they aware of raised blood pressure readings and were prone to white-coat hypertension, while nine gave no reason as to why they would not want further intervention.
Feedback on the pathway was positive. Participants valued the reminders to return their HBPM diaries, and there was also positive feedback regarding the communication back to GP surgeries.
Discussion
This pathway was developed to support hypertension case finding as well as treatment to target in those people known to have hypertension. The pathway promoted patient choice and facilitated primary and secondary care collaboration, as well as utilisation of home blood pressure readings. Importantly, capacity to check blood pressure opportunistically was increased. This may reduce some demand on nursing and healthcare assistant appointments within general practice. Improved collaboration between primary and secondary care aided interface working for the benefit of patients. Similar projects may be considered in outpatient settings, for example.
It is noteworthy that, out of 200 people in the study population, 33 were found to have raised home blood pressure readings and were subsequently treated to target. There were 13 new diagnoses of hypertension identified.
This study identified a high proportion of non-responders in the management of hypertension, with many declining further intervention and several requiring telephone reminders to return their home blood pressure readings. There is a role for education and self-management, as a number of individuals felt well and were therefore not inclined to continue participating in the pilot despite personalised reminders. There were a number of participants who were under the review of their GP and secondary care; it is likely that these patients would also require follow-up to ensure engagement with clinical management and achievement of treatment targets.
The pathway was very well received by participants, who valued the opportunity to have a blood pressure check and discussion about lifestyle. Written communication to the patients’ GPs was important to ensure that there was a safe transfer of care in addition to verbal and sometimes written communication with the patients.
We hope to continue this work on hypertension case finding and treatment to target as part of the DESP. We would hope that we can continue to build upon interface working with community providers/secondary care and primary care providers. Early treatment of hypertension and treatment to target of blood pressure is known to improve cardiovascular outcomes, especially in people with diabetes. Opportunistic testing may support early intervention and more favourable outcomes.
Resources
● British and Irish Hypertension Society – List of monitors for home use
● NICE – Hypertension in adults: diagnosis and management [NG136]
● UCL Partners Blood Pressure Optimisation Programme – includes a tool for estimating the impact of improving blood pressure control rates on CVD and the UCLP Proactive Care Framework
● British Heart Foundation – Manage your blood pressure at home – includes useful videos on measuring blood pressure at home and FAQs for patients
● Diabetes UK – Diabetes and Blood pressure
● Gov.uk – NHS diabetic eye screening programme





Counselling on appropriate genital hygiene is important for both men and women when initiating SGLT2 inhibitors and regularly thereafter.
21 Oct 2025