The landscape of diabetes care is changing, with growing diabetes prevalence, interest in type 2 diabetes remission, shift of management from glucose-centric to reducing disease burden, evolving technology and greater treatment repertoires. The needs of people with diabetes are also changing, to include:
- a younger population, who require earlier intensive management, including support with self-management
- a significant elderly/frail population with multiple co-morbidities needing particular attention to individualised care targets
- a need to reduce health inequalities in underserved populations.
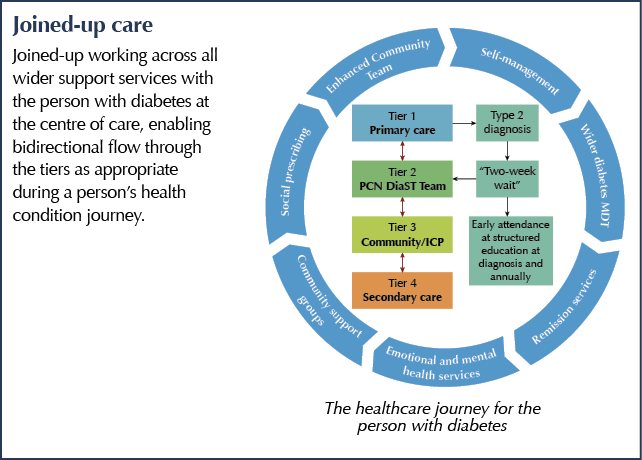
For the delivery of optimal outcomes, there is a pressing need to effectively facilitate the flow of people with diabetes through the different areas of the NHS and wider social support services depending on their needs at the point of healthcare access.
The formation and emergence of Primary Care Networks (PCNs) affords an opportunity to strengthen integration between primary, community and specialist care, and to provide diabetes services that address the needs of the person with diabetes, including the specific needs of underserved populations.
In recognising that PCNs across England are all at varying stages of maturity, the Best Practice in the Delivery of Diabetes Care in the Primary Care Network document serves as a guide to describe best practice in diabetes care. Based on the content, which is a review of current literature, identification of gaps in care and good practice examples, networks can adopt a bespoke “best fit” approach to enable working towards gold standards of diabetes care.
How will this guideline affect the person with diabetes?
- Ensure the delivery of appropriate, early structured education and management input, with improved early access to specialist services and the multidisciplinary team.
- Standardise the delivery of diabetes care, thus reducing variation.
- Facilitate a smooth flow of movement through the different levels of service depending on management needs at any one time-point in a person’s diabetes care journey.
How will this guideline affect primary care?
- Define standards for the management of different patient groups, as well as education and training of staff to ensure provision of high-quality, coordinated, patient-centred care across the board.
How will this guideline affect secondary care?
- Improve access to specialist services to those who require this.
- Develop working relationships with primary care, dissolving “siloed” working to better enable collaborative, coordinated, effective and patient-centred care.
Proposed key stages for PCNs
- Formation of a Diabetes Support Team (DiaST) within the PCNs to enable timely access to appropriate care.
- Ensuring healthcare professionals delivering diabetes care are appropriately educated and upskilled in diabetes management, which will be supported by the PCN DiaST.
- Early referral and intensive treatment for people newly diagnosed with diabetes, including attendance at structured education.
- A focus on holistic care: proposed care processes to address the need for holistic management and to address long-term disease burden.
- Focused care to certain groups and underserved populations in their localities, including those with frailty, young adults, ethnic minorities, certain people with type 1 diabetes and those with learning disabilities.
PCN DiaST (Diabetes Support Team)
This will be a new enhanced tier from within the existing PCN workforce providing care with an MDT approach.
- As a gold standard, practitioners within the team should include:
– GP with an extended role in diabetes (GPwER)
– Practice Nurse with special interest in diabetes
– Clinical Pharmacist (RPS Advanced Stage 2)
– Community/Intermediate Diabetes Specialist Dietitian
– With available access to mental health services and over-arched by strong communication links with the secondary care integrated team. - Practitioners will manage their own case-load and referrals for complex cases unable to be managed at tier 1 care and/or not meeting individualised treatment targets.
- Care at this level includes GLP-1 RA initiation, insulin initiation and multiple morbidity review.
- All new diabetes cases from within the PCN will be referred here to access dietary support, education and support for type 2 diabetes remission where appropriate, and to triage their care to the correct tier/services.
- Women of childbearing potential and all young adults with diabetes will be seen within this tier.
- Practitioners will also provide support and supervision for care homes and diabetes advice for others in the community MDT (e.g. district nurses/active case managers).
- The DiaST will have responsibility for appropriate diabetes-related education and clinical governance of other healthcare professionals within the PCN.







Counselling on appropriate genital hygiene is important for both men and women when initiating SGLT2 inhibitors and regularly thereafter.
21 Oct 2025