Aim of deprescribing
The aim of deprescribing is to reduce overtreatment, treatment burden and risk of harm. Deprescribing is a supervised process and involves the following (Aubert et al, 2021):
- Stopping or reducing the dose of a glucose-lowering drug.
- Switching to an alternative glucose-lowering class with a more favourable risk–benefit ratio or lower risk of hypoglycaemia.
- Simplifying a medication regimen.
- Reduction in self-monitoring of blood glucose.
- Reduction in the frequency of diabetes-specific assessments (e.g. checking of urinary albumin:creatinine ratio).
- Cessation or reduction of blood pressure medications or statins.
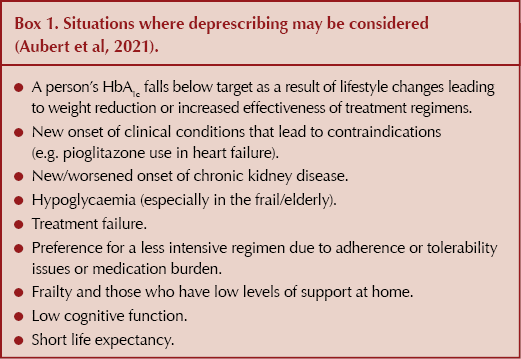
Box 1 highlights the situations where deprescribing may be considered.
Individualising treatment targets
Although SIGN (2017) and NICE (2022) recommend HbA1c treatment targets of ≤53 mmol/mol (48 mmol/mol at diagnosis) and ≤48 mmol/mol, respectively, HbA1c treatment targets should be individualised and agreed with the patient. This requires a multifactorial approach depending on the patient and disease features such as coexisting comorbidities, risk of hypoglycaemia, life expectancy, duration of diabetes and motivation (Davies et al, 2022). See Table 1 for recommended individualised HbA1c and fasting blood glucose level targets (Aubert et al, 2021; Strain et al, 2018).

Tips on deprescribing effectively and safely
If deprescribing is deemed necessary:
● Stop or reduce doses of glucose-lowering drugs that can cause hypoglycaemia (e.g. sulfonylureas), especially if a person is experiencing hypoglycaemia.
● If the patient is on an SGLT2 inhibitor, consider continuing it, especially if they have other comorbidities including chronic kidney disease, heart failure or established cardiovascular disease, as they may benefit from continuing this class of drug.
- However, the additional benefits of the class will need to be balanced with the risk of hypotension, mycotic genital infection and the need for the person to be able to implement sick day rules.
- Ensure the person’s eGFR is checked regularly to determine the SGLT2 inhibitor’s safety and efficacy.
● Treatment should only continue if the person’s individualised HbA1c target has been achieved 3–6 months after starting the treatment, or there has been an HbA1c reduction of 5.5 mmol/mol or more; otherwise, following review of adherence, treatment discontinuation and intensification of treatment with another therapy class should be considered (SIGN, 2017).
Deprescribing process
Deprescribing of glucose-lowering medicines should always be done following shared decision-making with the person or with their family/carer. When in doubt which glucose-lowering medicine should be deprescribed, the person could be asked their preference.
A tapering plan should be developed with the person or their family/carer to either stop the glucose-lowering drug, switch to another class or reduce the dose gradually over several weeks. In cases where a sulfonylurea dose has been reduced, increased frequency of blood glucose monitoring is required to ensure the deprescribing has been appropriate.
If the person has been experiencing hypoglycaemia, then dose reduction should continue until the hypoglycaemia resolves. If, following deprescribing, there is symptomatic hyperglycaemia or blood glucose levels rise above the individual’s target, return to the previous dose or consider switching to an alternative drug class with a lower risk of hypoglycaemia.
At each stage, optimise diet and lifestyle measures, but bear in mind this does not apply to the frail and elderly. Refer to Table 2 for the author’s suggestions on the principles of dose adjustment of glucose-lowering drugs.

Follow-up
Following deprescribing, follow-up with the patient to check their HbA1c or blood glucose levels is pertinent to ensure that deprescribing has not been detrimental to their glycaemic control. The clinician will need to ensure their practice has a good recall system in place.
As any HbA1c changes will not be seen until after 3 months, the patient should be advised to monitor symptoms of hyperglycaemia (excessive thirst or urination, fatigue) if they do not have a blood glucose meter and are not on any glucose-lowering drugs that cause hypoglycaemia. Those who have been provided a glucose meter should monitor their blood glucose levels regularly. In both cases, the person should be advised to contact their diabetes healthcare team if they have any concerns.





Daily oral GLP-1 receptor agonist in development results in significant weight loss but with no dosing requirements.
24 Sep 2025