The Brooklands and Northenden Primary Care Network (PCN) comprises five practices. The diabetes population has remained relatively consistent over recent years, comprising 1671 people, of whom 87% have type 2 diabetes. Within this population, 10.5% are aged 18–50 years.
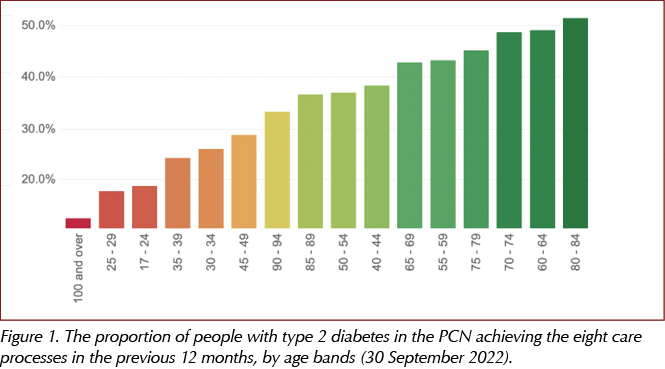
One of the key objectives of the PCN is to engage with and deliver focused care to underserved populations. In progressing this, we used “Diabetes Dashboards” created by the Manchester Integrated Care Team to identify which specific populations these were. We reviewed deprivation levels, ethnicities, frailty, age and type of diabetes in the dashboard data, and identified two particular underserved populations: adults with type 1 diabetes, and those under the age of 50 years with type 2 diabetes (Figure 1). Work by the PCN to optimise care for people with type 1 diabetes was presented at the Diabetes UK Professional Conference in 2023. This article focuses on the latter cohort.
Younger people with type 2 diabetes are known to be a population with particularly increased risk of long-term diabetes complications (Misra et al, 2023). This has significant long-term impact not only on the person with diabetes and their families, but also on the NHS and wider services. In addition, recently published data from the National Diabetes in Pregnancy Audit has demonstrated that the number of women entering pregnancy with pre-existing type 2 diabetes is increasing, as is the rate of severe adverse pregnancy outcomes in this group, while preparedness for pregnancy is decreasing (NHS Digital, 2023).
It is well evidenced that early intervention, to include lifestyle and appropriate management pathways such as weight management and possible remission of type 2 diabetes, is beneficial in this cohort (Wilmot and Idris, 2014; Lean et al, 2018). This article outlines how the PCN attempted to improve engagement with persons with type 2 diabetes under the age of 50 years, and the resulting outcomes and feedback.
The DiaST model of care
In seeking to restore and enhance diabetes pathways across the PCN in the wake of the COVID-19 pandemic, the PCN looked to the DiaST (Diabetes Support Team) model of care, described in the document Best Practice in the Delivery of Diabetes Care in the Primary Care Network(Ali et al, 2021). Recommendations on the formation and roles of the DiaST are listed in Figure 2 and Box 1.


In March 2022, COVID recovery monies were used to facilitate a primary care Diabetes Specialist Nurse working 24 hours a week across the PCN to lead the DiaST team to ensure deliverable outcomes in relation to three key aims listed in the PCN best practice guidance:
- Healthcare professionals (HCPs) delivering diabetes care should be appropriately educated and upskilled in diabetes management, thus supporting clinical governance and training needs.
- The focus for diabetes management should not solely reside in glycaemic management but also address the need for a holistic approach to diabetes care, to include cardiorenal protection and long-term disease burden.
- Delivery of focused care to certain groups and underserved populations in the PCN localities (e.g. people with frailty, young adults, people of black and minority ethnic background, people with type 1 diabetes, people with learning difficulties).
A clear difference in this model of care was the emphasis that the DiaST Lead was not there to take over the caseload of diabetes reviews but was there to deliver mentorship, education, advice and support in diabetes care. Fixed-term projects using a healthcare specialist in diabetes to undertake multiple review clinics may give improved clinical results in terms of treatment target attainment for the duration of input, but they may not leave a legacy for the PCN in terms of HCP learning and development, or give a dedicated focus on wider community engagement and population health management.
Alongside the local pay-for-performance Primary Care Quality Recovery and Resilience Scheme (Greater Manchester Integrated Care Partnership, 2023), we have implemented assessments outside of Quality and Outcomes Framework requirements, including a frailty review, mental wellbeing review and alcohol screening. This has allowed for greater holistic care consideration. Cardiorenal interventions, including bespoke clinics, have been at the forefront of education and review consultations, to align with the latest NICE NG28 guidance (NICE, 2022).
This innovative model of care allows for closer collaboration with secondary care. With current protracted waiting times due to capacity challenges, it has been relevant to ensure that referrals are for those who appropriately need specialist review (Nicholson et al, 2016). The DiaST Lead has the support of community and secondary care specialists for advice on the management of particularly complex cases.
Education for HCPs regarding earlier-onset type 2 diabetes
We used multiple educational outputs to highlight the optimal care of younger-onset type 2 diabetes, including educational meetings, hot-topic bulletin emails, dissemination of guidelines, leading by example, direct mentorship and the development of an “At a glance” aide-mémoire for use in consultations. The latter document is a one-page sheet serving to remind the HCP that, for those with earlier-onset type 2 diabetes, there are additional needs to address alongside what would be the gold standard of diabetes care for a person over the age of 50 years. Such specific considerations include pre-conception advice to women of childbearing potential, looking to lifetime cardiovascular risk as per NICE NG28, and a particular focus on ensuring a correct classification of diabetes.
Engaging people with earlier-onset type 2 diabetes
The DiaST team had bespoke conversations with people in the earlier-onset type 2 diabetes population to identify and try to understand barriers to engagement. From these conversations, the PCN developed and embedded the following actions:
- Active searches to identify those who needed to be reached.
- Development of the under-50s type 2 diabetes At a glance guide discussed previously.
- Extended-hours appointments, including evenings and weekends, enabled for phlebotomy and diabetes reviews.
- A home-visit team of HCPs to undertake required care processes and health education where needed.
- Collaboration with community teams (learning disabilities coordinators, social prescribers, care navigators).
- Bespoke phone contact from DiaST team members to assist with review and to encourage engagement.
- Opportunistic screening through diabetes templates and IT alerts.
- Creation of Data Protection Impact Assessments to support data-sharing for technology use (e.g. glucose monitoring platforms), thus enabling remote diabetes reviews.
- Community engagement work and attendance at local events with Health Development Coordinators.
- Joined-up work with Greater Manchester Strategic Clinical Network, facilitating a local engagement event to encourage uptake of the NHS England type 2 diabetes remission pathway.
- Review of data flow from secondary to primary care for recording care processes where these had been undertaken.
- Review of call/recall systems to ensure exemption coding is only used when appropriate.
- Enabling text messaging to include links to self-book appointments for diabetes reviews.
- Use of joined reviews such as cardio-renal-metabolic clinics to reduce the need for repeated/multiple visits to practices.
- Video on practice websites by two HCPs discussing the importance of regular diabetes review/care processes.
Results
Care process achievement
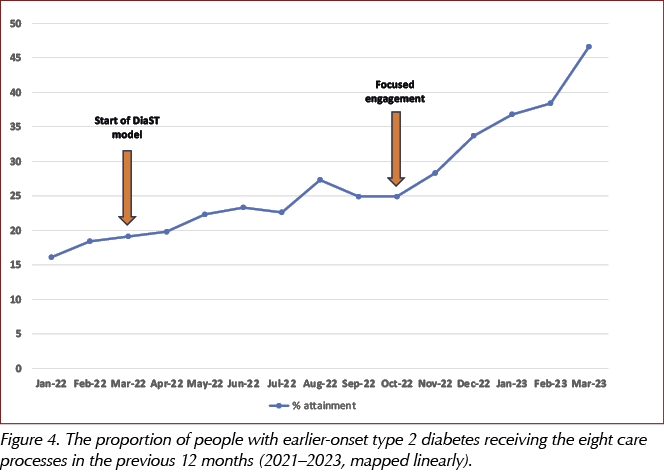
The proportion of people under the age of 50 years who had all eight of their care processes more than doubled, from 19.8% in April 2022 to just over 46.6% by the end of March 2023 (Figure 3). For comparison, across all age groups within the PCN overall, 53.4% of persons had received all their eight care processes. This serves to underline that variation, although reduced, does still persist and there remains the need to focus on engagement and outreach to the younger cohorts.

It is noted that the increased focus on this population from October 2022 accelerated the rise by 22% (Figure 4).
In addition to the 46.6% who had all their eight care processes completed, a further 30.1% had seven out of eight care processes completed (Figure 5).

The most commonly missed care process was the urine albumin:creatinine ratio, but nonetheless the proportion of people who had this measured more than doubled, from 31.5% in April 2022 to 67.0% at the end of March 2023. This has greatly served the cardiorenal workstream. Foot examination rates increased from 54.9% to 81.8%.
Achievement of treatment targets
There is the concern that, initially, as care process attainment increases, this may lower treatment target attainment rates, as more cases of hypertension, raised HbA1c and dyslipidaemia are identified. In line with this, the PCN was just over 1% down (from 32.0% to 30.7%) on three treatment target attainment rates over the 12 months from April 2022 to end of March 2023 (Figure 6). We were pleased, however, that there was not a more significant deficit.

In comparison with the 30.7% in the under-50s, across all age bands in the PCN, 45.5% of persons attained all three treatment targets. Again, this serves to highlight the health inequality in the 18–50-year-old population – in whom early, appropriate management is particularly important. We must continue to focus on achieving optimal treatment of all holistic parameters.
Economic analysis
We have not been able to undertake any specific economic modelling; however, Keng et al (2019) have modelled the impact of achieving primary care targets in type 2 diabetes, predicting improved health outcomes and reduced lifetime healthcare costs due to reduced complications, while Gæde et al (2016) have demonstrated the beneficial effects of holistic diabetes care on lifespan.
The costs for the project solely lie in the DiaST Lead time. Other DiaST multidisciplinary team members were from existing PCN staff, thus making best use of existing resources.
User and staff feedback
We have gathered comments from persons with diabetes and their families and carers. Much relates to the benefits from having engaged with care where they previously struggled to do so. Two case studies are included in Box 2.

Secondary care services have also been supportive of the PCN model and appreciative of prevented referrals and assumed reductions in admissions for acute complications of diabetes. HCPs value the support of a specialist clinician within their PCN who can offer timely advice, guidance and support. With staff burnout, recruitment and retention challenges at the forefront of current local and national policies, having the DiaST Lead within the PCN has led to an increase in HCP confidence and satisfaction in enabling optimal diabetes care.
Dissemination and sustainability
This project has developed into embedded and ongoing work. The inequalities in care processes and treatment target attainment we found for the PCN’s under-50s cohort are reflected nationally and highlight the timely need for NHS England’s T2Day (Type 2 Diabetes in the Young) initiative to provide extended reviews to promote gold-standard care for those with young-onset type 2 diabetes, which has been defined as that occurring in people aged 18–39 years.
The PCN’s work and resources have been shared both locally and nationally in promoting best practice. For 2023–2024, we intend to build on achievements and progress the work further to ensure higher levels of care process and treatment target attainment, and certainly to try to ensure equity with persons aged over 50 years.
We are working with the local ICB to share our learnings and assist in the development of templates and resources in support of the T2Day enhanced reviews.
Of note is that we have disproportionate numbers of younger persons with type 2 diabetes in the PCN’s areas of greatest deprivation. This is reflective of multiple research findings in this age group. A pertinent future ambition is an enhanced focus in the population-health arm of the DiaST model to look at ways to minimise the increased risk of the very development of type 2 diabetes in these areas.





