The Clinical Research Network (CRN) is part of the National Institute for Health Research (NIHR), which is effectively the “research wing” of the National Health Service (NHS). The CRN is funded to deliver high quality, ethically approved research studies on its portfolio, across all clinical specialties within the NHS, as well as in social care and public health. Primary care is one of 30 clinical specialties within the CRN and, in 2017/18, just under a third (32%) of all practices in England took part in CRN research.
The CRN is made up of 15 local networks covering England. Each has a Primary Care Clinical Research Specialty Lead, usually a GP. Their remit is to encourage and facilitate local primary care research, as well as contributing to the national agenda. A number of these networks have general practice incentive schemes that financially reward those practices undertaking CRN research and recruiting patients. This incentivisation funding allows practices to increase their capacity to deliver research, provide mandatory training to all practice staff involved in research and, in some cases, allow protected time for staff. This enables GPs or practice nurses, for example, to recruit patients into studies in person.
The full cost to the practice of undertaking a study is covered by the local network, so that each practice should never be out of pocket. Increasingly, local networks are engaging with groups of practices, federations, super-practices and mega-practices as the CRN evolves to promote research at scale. The local CRN team also employs research nurses to work within a practice to help deliver studies in these larger organisations.
By 2017, a million patients had been recruited into CRN studies led by primary care and over 1.5 million patients had been recruited in a primary care setting into studies across different specialties, including diabetes. Some high-profile diabetes studies, such as DiRECT (Lean et al, 2018), have recruited through practices, in this case in Newcastle and Scotland, facilitated by the CRN. Primary care is an excellent setting for diabetes research given the high prevalence of the condition, the quality of GP electronic records and because each patient with diabetes has at least an annual review.
Practices can also support local diabetes research by acting as a Patient Identification Centre (PIC) and identifying potentially eligible patients for secondary care. These patients are then sent a letter inviting them to contact the local diabetes centre for further information about a specific research project. This is relatively resource-light for the practice. Nowadays, the process can be made easier by sharing IT solutions, such as computerised search programmes that select eligible patients. These are disseminated to all interested practices by the CRN. A large number of practices undertake this type of activity.
Practices often ask why they should become research-active and undertake CRN research. There are many benefits to the practice in taking part in research. It can be empowering for GPs and patients alike to be helping to answer important research questions that are relevant to UK general practice. This is particularly true for chronic health conditions, such as type 2 diabetes, for which care is predominantly conducted in general practice. Patients will often receive new treatments for their diabetes in the context of a controlled trial. This has benefits for the patients both in the intervention and control arms, as evidence has shown that all patients in clinical trials have better outcomes. This may be due to the extra focus and attention on their health that participants receive.
Practices have found that developing a research interest not only produces a new income stream, but leads to a novel aspect of staff development and portfolio careers. In some instances, undertaking CRN research has been identified by the Care Quality Commission (CQC) as a marker of quality. Both patients and doctors also receive the satisfaction of participating in research that can expand the boundaries of medical science. Patients often comment that they enjoy “giving something back to the NHS” and GPs often say that it can be satisfying to be able to offer something extra to patients. The CRN has a strong “patient voice”, with many examples of patients who have had positive experiences from taking part in research at their GP surgery.
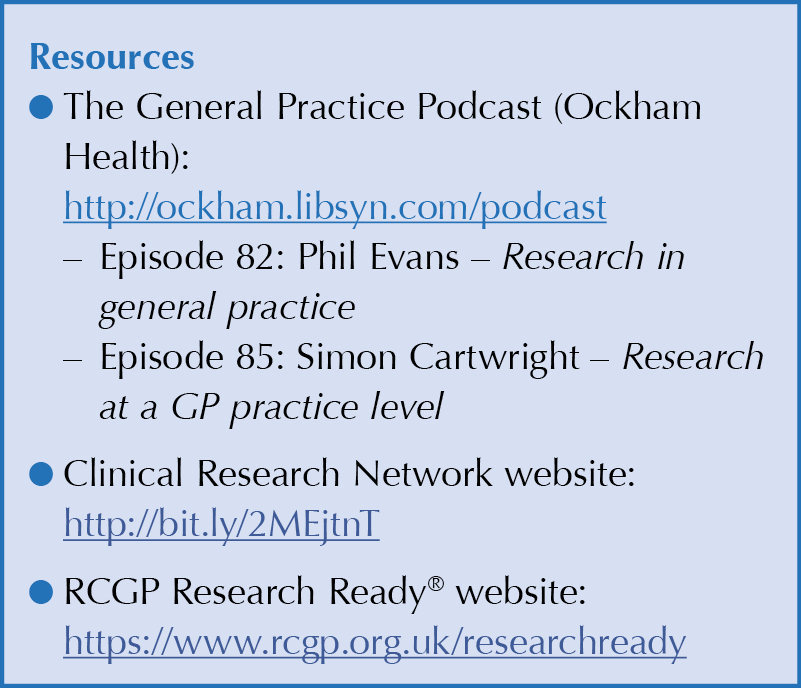
One way to become more involved in research is to seek accreditation with the Royal College of General Practitioners’ Research Ready® scheme. This programme allows the practice to become prepared to undertake research. In addition, every GP or staff member that actively takes part in research needs to have Good Clinical Practice (GCP) training, which is provided by the NIHR free online.
A few practices undertake their own research and there are a small number of stand-alone research practices in England doing just this. For example, PHE’s practice (St Leonard’s Practice in Exeter) has published papers on opportunistic screening for type 2 diabetes (Evans et al, 2008). In addition, a small proportion of practices (around 3%) undertake industry-funded research in the CRN. These studies can provide a good income stream, but they are more complex and require a greater level of governance and scrutiny given that new, commercially sensitive treatments may be being brought to primary care for the first time.
In some cases, practices develop very close links with their local diabetes study teams, such as Claremont Medical Practice in Exmouth (LG’s practice). They have piloted new ways to deliver diabetes studies, with pop-ups to remind clinicians to hand out a leaflet or to introduce a study of a new drug (if relevant to the patient). This is light-touch and easy for practice teams and patients alike.
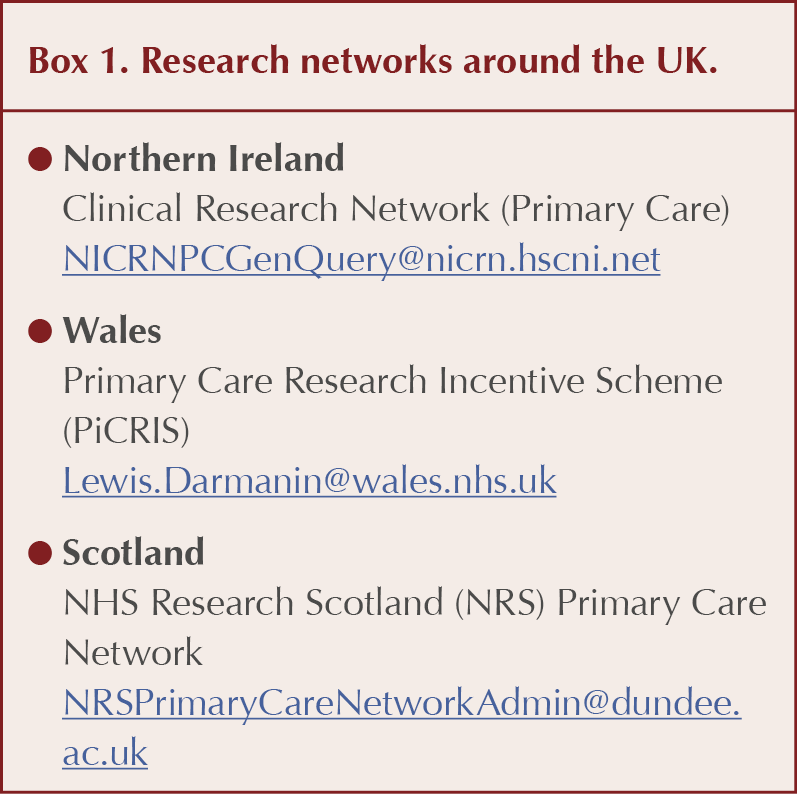
If you or your practice are interested in moving into research (in England), please contact your local Clinical Research Network (see Resources below) and talk to the team. There are also similar research networks in the devolved nations (see Box 1 for details). A number of networks have an annual primary care forum for research and, again, this may be a useful way of “dipping your toe into the water” to see if research is for you.





Satish Durgam reviews who will be eligible to receive tirzpepatide for weight management and when.
24 Apr 2025