Oncology and palliative care
Su Down, Diabetes Nurse Consultant, Somerset
● 20% of people with cancer have diabetes.
● Diabetes provides the perfect environment for cancer cell growth:
- Insulin is a growth factor.
- Inflammation.
- Hyperglycaemia.
Type 3c or pancreatogenic diabetes
● Results from structural damage to the pancreas (due to e.g. pancreatitis, cystic fibrosis, haemochromatosis). 80% of cases will be related to pancreatitis.
● Type 3c makes up 8–10% of all diabetes, yet we rarely consider it.
● We should ask ourselves, “How do I know this is type 2 diabetes – could it be another type?”
● Check faecal elastase test; CT to assess pancreatic damage; exclude autoantibodies which would suggest type 1 diabetes.
● Can identify these people by looking at those who needed insulin within 5 years of diagnosis.
Pancreatic carcinoma
● Difficult diagnosis and often made late.
● Have high index of suspicion – NICE NG12 recommends urgent 2-week-wait CT scan in all over age 60 years who have weight loss and new type 2 diabetes; also in those whose glycaemic control suddenly deteriorates.
Management of diabetes during chemotherapy
● Hyperglycaemia can make chemotherapy less effective; increased risk of infections and of hospitalisation.
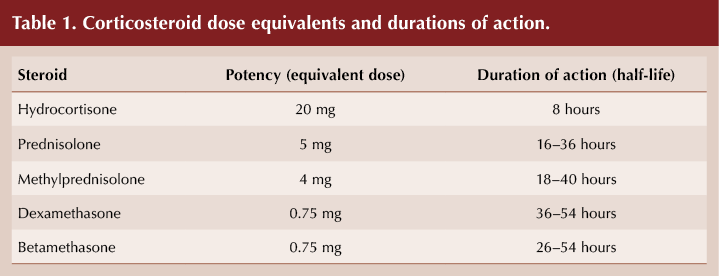
● Steroids are often used in large intermittent doses – goals are to limit glucose rises later in the day whilst avoiding overnight hypoglycaemia.
- Prednisolone usually taken as morning dose; hyperglycaemia may develop a few hours after taking and may then wear off.
- Dexamethasone may result in more prolonged hyperglycaemia through whole 24 hours (see Table 1).
● Some drugs (e.g. checkpoint inhibitors), can cause rapid-onset new type 1 diabetes.
Deprescribing and end-of-life care
● Language matters, good communication is important and regular discussion is needed.
● Manage nausea and vomiting.
● Cancer cachexia and sarcopenia are common; gradually deprescribe therapies and provide nutritional support. Any type of energy intake, including nutritional supplement drinks, is important – it is the clinician’s role to manage the impact on glycaemia. Prescribe to avoid symptomatic hyperglycaemia and hypoglycaemia.
● Ideally provide CGM to avoid distressing capillary glucose testing.
● If prognosis >3 months: deprescribe SGLT2 inhibitors, ACE inhibitors, ARBs, statins.
● If prognosis <2 months: remove mealtime insulin, retain basal background therapy, decrease sulfonylurea.
● Prioritise removing drugs if they interfere with appetite (e.g. metformin, DPP-4 inhibitors, GLP-1 receptor agonists) or carry hypoglycaemia risk.
Psychological care in diabetes
Becky Houghton and Shannon McAleese, Psychologists, Northern Health & Social Care Trust
Qualitative research demonstrates that both HCPs and people with type 1 diabetes have similar views about what is important to them. Three interconnected themes were raised by the research shared:
● The importance of being seen and heard.
● Management should feel like a collaborative alliance of two experts.
● Impact of the healthcare system – time, lack of resources impactful. Telehealth may provide a partial solution.
Questions to use for a wellbeing check-in:
● How can I be of most help to you today?
● What do we need to make sure we talk about?
● How are things going with your diabetes at the moment?
- What do you feel isn’t going as well as you would like?
- What do you feel is going well (can use the PAID [Problem Areas in Diabetes] questionnaire to help identify what is going well or not).
● Who do you talk to when your diabetes gets rough going? And how do they help?
● Is there anything getting in the way of you looking after your diabetes at the moment?
Insulin dilemmas
Neil Black, Consultant Physician and Clinical Lead, Endocrinology & Diabetes, Western Health & Social Care Trust
Steroid-induced hyperglycaemia
● In those without diabetes, 30% develop hyperglycaemia and 18% develop diabetes; may resolve with cessation of steroids. In those with pre-existing diabetes, 100% develop hyperglycaemia.
● Management: gliclazide 40–80 mg morning; uptitrate to 160–240 mg; add afternoon dose – total 320 mg per 24 hours. Insulin may be required.
● Glucose lowers within 2–3 days of steroids being reduced – so adjust gliclazide dose.
● Seek specialist support if insulin required.
● In end-of-life care, avoid hypoglycaemia and symptomatic hyperglycaemia.
Rescue therapy
● Consider if HbA1c is ≥90 mmol/mol, or lower if osmotic symptoms.
● Add in sulfonylurea to maximum dose, then add insulin if needed.
● Remember to exclude other types of diabetes – type 1 and LADA.
Downtitration of hypoglycaemic agents
● Important to understand the modes of action of different therapies and their benefits and potential adverse effects.
● When adding a new agent: halve the sulfonylurea dose (can consider reducing it to once daily); reduce insulin dose by 20–30%.






Jane Diggle examines the draft update to the NICE NG28 clinical guideline, plus new advice regarding the discontinuation of Levemir.
10 Sep 2025