People with diabetes have a 19%–34% lifetime risk of foot ulcer. Ulcers are the leading cause of non-traumatic lower limb amputations, yet they are largely preventable with good foot self-care. Five-year mortality rates following amputation are 45%–57% (NICE, 2019), much higher than with most cancers. Previous studies have identified that, unfortunately, people with diabetes often do not take care of their feet until foot ulcers develop, when amputation may already be inevitable. This UK, qualitative study (Hill et al, 2022) aimed to identify barriers and facilitators motivating foot self-care, to identify areas of consensus between the perspectives of people with diabetes and healthcare professionals (HCPs), and to identify ways to improve foot self-care. In-depth, semi-structured patient interviews (9) and HCP interviews (7) were undertaken, and interview findings discussed by two separate patient groups to identify areas of agreement and difference.
Concerns over the consequences of diabetes, informed by personal experience, vicarious experience watching others with complications, and clinician messages about seriousness were identified as increasing people with diabetes’ motivation to self-care for their feet, while absence of these meant that people did not see foot care as important. Being well-informed, communicating well with their HCPs and having the time and physical ability to tend to their feet, enabled self-care.
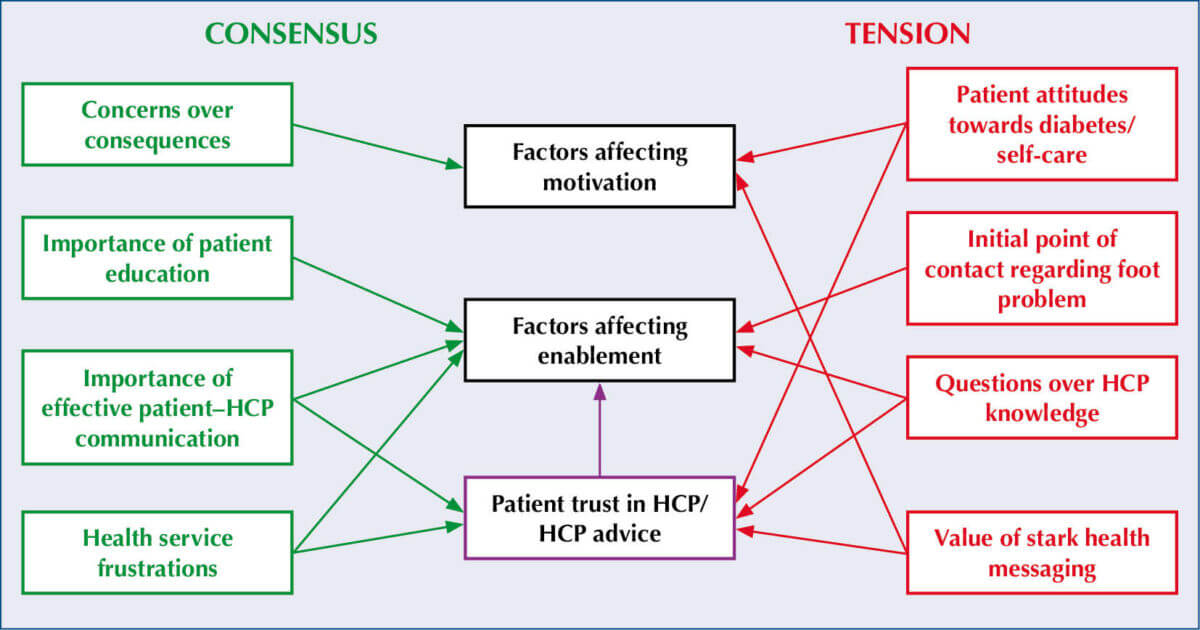
Areas of consensus between the people with diabetes and HCPs in the study are summarised in Figure 1. They included concerns around consequences of diabetes complications, importance of patient education and frustrations around aspects of NHS care delivery. Important tensions included mixed messaging from HCPs around who has responsibility for foot health, and confusion over who to contact should a foot problem develop. HCPs appeared to attribute lack of motivation to undertake foot self-care to lack of patient knowledge, and non-specialist HCPs tended to avoid foot-care discussions owing to perceptions of their own lack of knowledge.
Despite the limitations of the study (conducted in an affluent and largely white British population, small sample size and limited range of HCPs included), this paper helps us identify simple steps we can easily take to overcome some of the barriers to foot self-care, as well as raising important questions for discussion within our practice or service. For example, do all our team know when and how to access the specialist foot care team? Do people with diabetes clearly understand their own foot self-care role and to consult immediately if foot problems develop? And post pandemic, do our current access arrangements ensure people with diabetic foot problems can get same-day access to an appropriate clinician?
Take-home messages for clinicians include the importance of:
- Improving motivation by helping people develop their own, individual reasons to undertake foot self-care.
- Consistent messaging across all team members, including the roles of HCPs and people with diabetes in foot care.
- Clear education on when, where and how to ensure rapid clinician access, which will differ in different parts of the UK.
- Identifying and filling gaps in our own diabetic foot-care knowledge to increase our confidence in discussing foot self-care, rather than just examining feet.
Click here to read the full article.






Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025