Survodutide for weight loss
Survodutide (BI 456906), a novel dual GLP-1 and glucagon receptor agonist, demonstrated weight loss of up to 18.7% over 46 weeks in overweight or obese people participating in its phase 2, randomised, placebo-controlled, dose-finding trial presented at the Sessions. A total of 387 participants with a BMI ≥27 kg/m2 were allocated to 0.6 mg, 2.4 mg, 3.6 mg or 4.8 mg of survodutide once weekly, delivered by subcutaneous injection. There was a 20-week, rapid (every 2 weeks) dose-escalation phase and a 26-week maintenance phase.
The primary end point was the mean percentage change in body weight at 46 weeks, with results as follows in the different study arms:
- Placebo: –2.8%.
- Survodutide 0.6 mg: –6.2%.
- Survodutide 2.4 mg: –12.5%.
- Survodutide 3.6 mg: –13.2%.
- Survodutide 4.8 mg: –14.9%.
Those who reached and stayed on the 4.8 mg dose had a mean weight loss of 18.7% at week 46.
Secondary endpoints included the proportions of participants achieving 5%, 10% and 15% weight reductions, and 82.8% of survodutide recipients achieved at least 5% weight loss by week 46, compared with just over a quarter of those on placebo.
The principal investigator for the study, Professor Carel le Roux (University College Dublin), highlighted that, “by activating both the GLP-1 receptor and glucagon receptor, survodutide may both inhibit appetite and improve energy expenditure.”
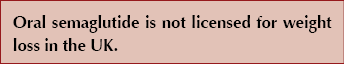
Oral semaglutide for weight loss: OASIS 1 trial
Oral semaglutide is used at doses of 7 mg and 14 mg daily for glucose-lowering treatment in people with type 2 diabetes. In the OASIS 1 (Oral Semaglutide Treatment Effect in People with Obesity) phase 3 trial, higher doses of oral semaglutide – titrated up to 50 mg daily – were investigated, together with lifestyle changes, for impact on weight loss over 68 weeks. The 667 participants had a baseline BMI of ≥30 kg/m2 or ≥27 kg/m2 plus a weight-related complication, but people with type 2 diabetes were excluded.
The co-primary endpoints, compared with placebo at 68 weeks, were both significant:
- Percentage body weight loss: 15.1% with semaglutide 50 mg versus 2.4% with placebo.
- Proportion who achieved ≥5% weight loss: 85% with semaglutide 50 mg versus 26% with placebo.
Weight reductions of 10%, 15% and 20% were also achieved in more participants with semaglutide 50 mg versus placebo, with two thirds of semaglutide 50 mg recipients achieving ≥10% body weight reduction and one third achieving ≥20%. Of those who completed the trial on treatment, 80% were taking the 50 mg dose, suggesting that tolerability was acceptable. Mild to moderate altered skin sensation occurred more commonly in those taking semaglutide during dose escalation but resolved without therapy discontinuation.
Other outcomes included a significant 57% reduction in high-sensitivity CRP, a marker of inflammation that can be used to assess future CVD risk; similar improvements have previously been observed with higher doses of subcutaneous semaglutide for obesity (Verma et al, 2022).
Key limitations included the trial population (largely white with a high percentage of female participants); the exclusion of people with type 2 diabetes; adherence and the fact that monitoring of whether oral semaglutide was taken exactly as recommended did not occur; and the flexibility in implementation of the associated lifestyle intervention.
Results in OASIS 1 were broadly similar to those seen with injectable semaglutide 2.4 mg in the STEP series of trials. Cardiovascular outcome studies – SOUL (oral semaglutide up to 14 mg) and SELECT (injectable semaglutide 2.4 mg) are ongoing.
Commenting on the OASIS 1 results, Professor Filip Knopp (University of Copenhagen) highlighted the significant body weight reductions seen in the trial, and the importance of having both oral and injectable versions of semaglutide available to aid weight loss.
The full study was simultaneously published in The Lancet.
Tirzepatide for weight loss: SURMOUNT-2 trial
The SURMOUNT-2 study, which was simultaneously published in the Lancet, demonstrated an average weight loss of 15% (average weight reduction of 14–16 kg) with tirzepatide after 72 weeks in people with type 2 diabetes and comorbid obesity or overweight. This was noted as the highest degree of weight loss achieved with drug therapy to date in clinical trials in people with type 2 diabetes.
From an average of 8.0% (64 mmol/mol) at baseline, HbA1c decreased to an average of 5.9% (around 41 mmol/mol), and nearly 50% of tirzepatide recipients achieved levels of <5.7% (39 mmol/mol).
Professor Timothy Garvey (University of Alabama at Birmingham) commented, “We are encouraged by these weight loss and glycaemic control results, especially as weight loss interventions are typically less effective in patients with diabetes.”
This study is reviewed in more detail in Diabetes Distilled.
New drugs and new doses for type 2 diabetes
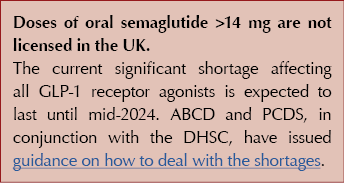
Oral semaglutide for type 2 diabetes: PIONEER PLUS
Oral semaglutide 7 mg and 14 mg daily are currently available for glucose lowering in people with type 2 diabetes. The PIONEER PLUS randomised, double-blind, active-controlled trial aimed to evaluate the safety, tolerability and efficacy of 25 mg and 50 mg doses of a new formulation of oral semaglutide in people with type 2 diabetes. Baseline HbA1c ranged from 8.0% to 10.5% (64 to 91 mmol/mol), mean HbA1c was 9.0% (75 mmol/mol), and participants had a BMI of 25 kg/m2 or greater and were treated with 1–3 other oral glucose-lowering drugs.
The primary endpoint was mean change in HbA1c at 52 weeks, with the following results:
- 14 mg: –1.5% (16 mmol/mol).
- 25 mg: –1.8% (20 mmol/mol).
- 50 mg: –2.0% (22 mmol/mol).
This HbA1c reduction is greater than that seen with the 14 mg dose of oral semaglutide in earlier phase 3 studies in the PIONEER programme (1.0–1.4% reductions), and was likely due to higher baseline HbA1c.
Weight loss occurred in all groups, with mean weight reductions of 4.4 kg, 6.7 kg and 8.0 kg in those taking 14 mg, 25 mg and 50 mg, respectively, at 52 weeks. More people treated with the 25 mg or 50 mg doses achieved weight loss of ≥5% or ≥10% compared to those taking the 14 mg dose at 52 weeks. Waist circumference was also measured, and decreased more in those treated with 25 mg and 50 mg than with 14 mg.
Adverse events were typical of those seen with GLP-1 receptor agonists, and were reported by 76% of participants taking 14 mg, 79% on 25 mg and 80% on 50 mg. Gastrointestinal adverse effects, mainly mild to moderate, were slightly more common in those taking the 25 mg and 50 mg versus 14 mg doses, and mainly occurred during the dose-escalation phase. Despite these adverse events, 83%, 79% and 81% completed treatment in the 14 mg, 25 mg and 50 mg groups, respectively.
The authors proposed that dose increases of existing medications offer clinicians a simple way to individualise therapy. This may help reduce clinical inertia as it is easier than initiating new medication or switching.
The study was simultaneously published in the Lancet.
Orforglipron for weight and glycaemia
Orforglipron is an oral, small-molecule, non-peptide GLP-1 receptor agonist in development for the treatment of type 2 diabetes and obesity at doses of 12–45 mg per day. It can be taken with no restrictions on food or drink intake, unlike oral semaglutide, which must be taken on an empty stomach with a sip of tap water and no food or other fluids for at least 30 minutes to ensure absorption of the drug.
Orforglipron demonstrated improved HbA1c reduction and weight loss efficacy compared to subcutaneous dulaglutide 1.5 mg once weekly in a dose-ranging study conducted over 26 weeks. Two different dose-escalation regimens were used for the 36 mg and 45 mg groups, (different starting doses and escalation schedules to explore tolerability).
The mean baseline HbA1c was 8.1% and BMI 35.2 kg/m2. Orforglipron 45 mg was significantly more effective in reducing HbA1c compared with placebo, achieving a mean placebo-subtracted reduction of 1.67% and a mean weight loss of 10.1 kg versus 2.2 kg with placebo at week 26. Doses of 12 mg and above had a greater impact on HbA1c than placebo or dulaglutide 1.5 mg in this short study.
Almost half of those treated with orforglipron achieved ≥10% weight loss. Adverse events occurred in up to 89% of those treated with orforglipron, compared to 62% with placebo and 56% with dulaglutide. Nausea, vomiting and diarrhoea were reported more frequently with orforglipron than with dulaglutide at equivalent doses. Discontinuation rates for orforglipron were higher, at up to 20%, compared with dulaglutide 1.5 mg (10%), which was thought to relate to the higher starting dose and speed of dose titration of orforglipron rather than the final dose.
The authors of an associated commentary called for more structured evaluation of the gastrointestinal side effects of GLP-1 receptor agonists using validated measures used for other gastrointestinal conditions (Nauck and Horowitz, 2023).
Since orforglipron does not require food or water restrictions, it may in future offer a convenient oral GLP-1 receptor agonist option alongside other oral and injectable drugs within the class. Orforglipron continues to be evaluated in the phase 3 ACHIEVE programme. Further evaluation is needed to identify the optimal starting dose and titration schedule to minimise gastrointestinal side effects and treatment discontinuation.
The study was simultaneously published in the Lancet.
Orforglipron was also evaluated to treat obesity in people without type 2 diabetes, published in the New England Journal of Medicine.
Retatrutide, a triple receptor agonist for type 2 diabetes
Retatrutide, a single-peptide, triple agonist of the GIP, GLP-1 and glucagon receptors, demonstrated dose-dependent, clinically significant reductions in HbA1c and weight, which were greater than with dulaglutide 1.5 mg in this dose-ranging study.
Currently in development, retatrutide is known to have glucose-lowering and weight-reducing effects, and in this randomised, double-blind, placebo-controlled and active-comparator, phase 2 trial, the effects of 0.5 mg, 4 mg, 8 mg, 12 mg and different initiation doses of retatrutide were compared with dulaglutide 1.5 mg once weekly and placebo. Participants had a baseline HbA1c of 7.0–10.5% (53–91 mmol/mol) and a BMI of 25–50 kg/m2.
For the primary endpoint of change in HbA1c from baseline to 24 weeks:
- All but the retatrutide 0.5 mg group had greater reductions than placebo.
- Retatrutide 8 mg (1.9%) and 12 mg (2.0%) had greater reductions than dulaglutide (1.4%).
For the secondary endpoints of change in HbA1c and weight from baseline to 36 weeks:
- HbA1c reductions were maintained at 36 weeks.
- Weight reduction was nearly 17% for the retatrutide 8 mg and 12 mg groups, compared to 3% with placebo and 2% with dulaglutide 1.5 mg.
As expected, mild to moderate gastrointestinal side effects were reported by 35% on treatment with retatrutide, comparable to dulaglutide 1.5 mg.
An accompanying commentary by Bain and Min (2023) explores the development of incretin drugs for both glycaemic management and weight reduction, and calls for the phase 3 trials of retatrutide to include higher-dose GLP-1 and dual GIP/GLP-1 receptor agonists as active comparators, rather than dulaglutide 1.5 mg. Bain and Min remind us that GLP-1 receptor agonists reduce weight by promoting satiety, and that the additional weight reduction from the glucagon receptor agonism is likely to be due to effects on increasing energy expenditure. This means that long-term cardiovascular outcome trials are likely to be mandated, which will slow the progress to clinical use.
The study was simultaneously published in the Lancet, while a phase 2 trial of retatrutide for obesity (excluding people with type 2 diabetes) was published in the New England Journal of Medicine.






SURMOUNT-5 trial pits tirzepatide against semaglutide, plus behaviour change support, for weight loss.
15 May 2025