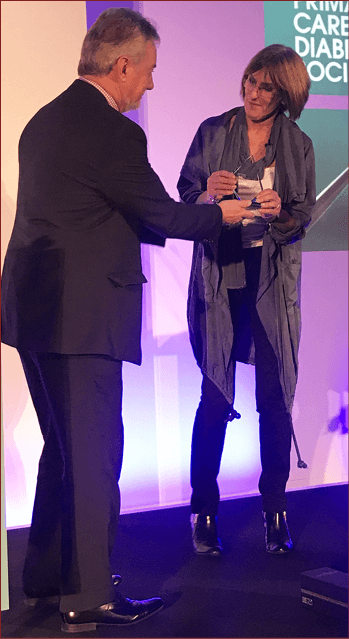
The PCDS Lifetime Achievement Award to Gwen Hall
Presented by Eugene Hughes
I was immensely proud to present my colleague and friend, Gwen Hall, with the second PCDS Lifetime Achievement Award in front of a large audience at our 13th National Conference in Birmingham. I told the delegates that I had better (on pain of death) list some of her notable achievements.
Gwen has long experience as a Diabetes Specialist Nurse and facilitator/educator, having worked across Surrey and, more recently, as part of the award-winning Portsmouth Community Health Services primary care team that devised the Super Six model of diabetes care.
In 2007, Mary MacKinnon invited Gwen to update her authoritative book, Providing Diabetes Care in General Practice. Gwen regarded this as a great honour, as Mary’s pioneering work had hugely influenced her professionally.
Gwen was a long-standing member of the PCDS Committee and, in 2005, was elected as Vice-Chair, a post that she held for nine years. Between 2001 and the end of 2014, she was Associate Editor-in-Chief of Diabetes & Primary Care. She was bold and innovative in this role, introducing new concepts and features to strengthen the educational potential of this prestigious journal, and paving the way for its transition to a digital format. She continues to be an active member of the editorial board.
In addition, she was an Associate Clinical Teacher for the University of Warwick, for whom she also helped to organise and run Diabetes Care courses for GPs, practice nurses and primary care teams.
A measure of the regard in which she is held was the awarding to her of the prestigious Mary MacKinnon Lecture at Diabetes UK’s Annual Professional Conference in 2008.
But Gwen is so much more than the sum of these achievements. She is passionate about all aspects of diabetes, and is an excellent communicator. Her lectures and presentations combine clarity and practicality with a wicked sense of humour.
And, above all, Gwen will always be regarded as a friend. A friend to people who have sought her help and opinions at meetings, a loyal friend to the PCDS and all its activities, and a trustworthy friend to many healthcare professionals who cherish her wisdom and compassion.
In further recognition of Gwen’s contribution to diabetes care, she will be giving the first annual Gwen Hall Education Lecture at this November’s PCDS National Conference. There is no doubt that her address will be both passionate and insightful. Try not to miss it!
Diabetes prevention
Naresh Kanumilli, GP, Manchester, and Lesley Hamilton, Diabetes Specialist Dietitian, Londonderry
- Those at risk of non-diabetic hyperglycaemia can be identified through the NHS Health Check programme in England or by using a practice search tool, such as Leicester practice tool at https://bit.ly/2klqtbS.
- In England, people are eligible for the Healthier You: National Diabetes Prevention Programme if their last HbA1c (carried out within 12 months) is 42–47 mmol/mol (6.0–6.5%), or fasting plasma glucose is 5.5–6.5 mmol/L (6.9 mmol/L in some areas), and they are aged >18 years, are not pregnant and are able to take part in a group programme.
- The programme varies slightly from region to region, but it is evidence-based and includes an initial individual assessment and 18 community-based behaviour-change group education sessions over 9 months (initially weekly, then fortnightly).
- Programmes have demonstrated evidence of weight loss and reduced rates of progression to diabetes. The NHS programme has recently been rolled out across the whole of England.
- Are you keen to learn more? The diabetes prevention module from the PCDS, funded by the Welsh Government, is currently being updated and will be available at www.diabetesonthenet.com/course.
Sexual dysfunction and diabetes
Lesley Mills, Consultant Nurse in Diabetes, Warrington
- Sexual health problems are common in people with diabetes. In the EDIC study (Enzlin et al, 2009), amongst sexually active women with type 1 diabetes, 35% met the criteria for female sexual dysfunction (57% loss of libido, 51% problems with orgasm and 47% problems with lubrication).
- Primary care has a role in helping with coping strategies, diabetes management, prescribing PDE5 inhibitors in men at low risk of CV disease, lubrication and referral for testosterone replacement when appropriate.
- Erectile dysfunction (ED) can be an early sign of vascular disease and diabetes.
- Men with diabetes are 2–5 times more likely to develop ED, and to get it 10–15 years earlier, than men without diabetes. During their lives, 50–74% of men with diabetes will have ED.
- Ask about the speed of onset of ED, presence of physiological erections, bladder symptoms, or symptoms of autonomic or peripheral neuropathy or macrovascular disease, and take a drug history.
- Examine the genitalia and conduct neurological, endocrine and CV (including BP) examinations, and prostate examination, if appropriate.
- Consider managing those at low CV risk in practice. Refer for further CV evaluation those at moderate or high CV risk and defer ED management until receipt of advice or outcome of investigations from secondary care.
- Remember that thyroid problems can cause ED and ejaculation problems.
- Consider testosterone deficiency. Levels >12 mmol/L total testosterone do not require treatment, but a treatment trial (usually initiated in secondary care) may be appropriate at levels below this.
- Treatment options include: oral PDE5 inhibitors (including sildenafil, tadalafil [including daily], vardenafil, avanafil, all prescribed generically); vacuum devices; Vitaros (topical Alprostidil cream with permeation enhancer); MUSE urethral pellet; and intracavernosal injection of Caverject or Invicorp (aviptadil and phentolamine mesilate).
- NICE guidance recommends that all men with diabetes are asked about ED annually and offered a PDE5 inhibitor, unless these are contraindicated. If this is not effective, consider referring to specialist care.
At the heart of diabetes: drugs on trial
Kevin Fernando, GPwSI in Diabetes and Medical Education, North Berwick, and David Millar-Jones, GP, Cwmbran
- Use the QRisk3-2017 calculator to calculate 10-year cardiovascular risk.
- Cardiovascular disease (CVD) is the leading cause of death in type 2 diabetes. The risk is around double those without type 2 diabetes (The Emerging Risk Factors Collaboration, 2010). Despite optimal treatment of risk factors, there is still significant residual CV risk in those with diabetes (Gæde et al, 2016).
- Aim to optimise BP at <140/80 mmHg, or <130/80 mmHg if there is kidney, eye or CV damage – but individualise. BP control is more important than the agent used. Use ACEI/ARB as first-line therapy for established microalbuminuria.
- Use aspirin for CVD prevention only if established CVD (NICE, 2015a). The ASCEND study, due to report in 2018, will provide evidence on CVD prevention in those without known arterial disease.
- The number needed to treat (NNT) to prevent one CV event is 34 for lowering BP by 10/5 mmHg; 44 for lowering total cholesterol by 1 mmol/L; and 119 for lowering HbA1c by 11 mmol/mol (1%).
- The LEADER study demonstrated reduced CV mortality (NNT 104 over 3 years) and all-cause mortality (NNT 98) with liraglutide in those at high risk of CVD. SUSTAIN-6 demonstrated reduced non-fatal stroke (NNT 90 over 2 years) with semaglutide. Exenatide and lixisenatide did not demonstrate reductions in CV or all-cause mortality in ELIXA and EXSCEL.
- EMPA-REG OUTCOME demon-strated a reduction in CV mortality (NNT 45 over 3 years) and all-cause mortality (NNT 38) with empagliflozin; CANVAS/CANVAS-R demonstrated a reduction in the composite endpoint, but no reduction in all-cause or CV mortality with canagliflozin; and CVD-REAL demonstrated decreased all-cause mortality with SGLT2 inhibitors.
- Metformin is safe in CVD and heart failure (HF) and currently remains first-line pharmacological choice, but many studies are still to report.
- HF rates are double in men with diabetes compared to those without; in women, the risk is >5-fold in those with diabetes compared to those without.
- EMPA-REG OUTCOME demon-strated reduced hospitalisation for HF (NNT 71 over 3 years) with empagliflozin; CANVAS/CANVAS-R 33% a relative risk reduction in hospitalisation for HF with canagliflozin; and CVD-REAL decreased rates of hospitalisation for heart failure with SGLT2 inhibitors.
- There is no significant benefit in reduction of HF hospitalisation with GLP-1 receptor agonists or DPP-4 inhibitors, and a small increase with saxagliptin. Pioglitazone is contraindicated in HF.
Complex cases
Eugene Hughes, GP, Isle of Wight
- Non-alcoholic fatty liver disease (NAFLD)
- LFT levels are normal in 80% of people with fatty liver. Screening is not recommended. Fatty liver is the commonest reason for raised ALT levels in those with diabetes.
- NAFLD is a diagnosis of exclusion, and we need to rule out other causes of liver disease.
- In people with type 2 diabetes, NAFLD is a risk factor for atrial fibrillation, myocardial infarction, ischaemic stroke and CV death. CVD risk-factor management is therefore important.
- NAFLD is not a contraindication to statin therapy. ALT level should be checked prior to statin use. If levels are <3 times the upper limit of normal, statins can be started. Check again at 3 months and 12 months – stop statin use if there is a greater than doubling of levels by 3 months or if it is >3 times upper limit of normal.
- Steroid-induced diabetes (SID) or steroid-induced hyperglycaemia (SIH)
– The risk of SIH and SID depends on the steroid dose and duration of use. The risk factors are as for diabetes.
– Monitoring: Use once-daily SMBG, before or after lunch or tea, if there is no diabetes, increasing in frequency if any one reading is >12 mmol/L. In established diabetes, use 4-times-daily SMBG, aiming for a reading of 6–10 mmol/L, but accepting 4–12 mmol/L. Individualise for frail, elderly and other higher risk groups, and for end of life.
– Consider escalation of therapy if there are two SMBG readings >12 mmol/L in 24 hours – optimise metformin, but insulin or sulfonylureas are usually required. Watch for hypoglycaemia and decrease diabetes therapies as the steroid dose is decreased.
- Older people
– Consider any new symptom as being related to a medicine(s) until proven otherwise.
- Mental health problems
- SGLT2 inhibitors
Guidelines and resources
- ABCD guidance on managing steroids: https://bit.ly/1UyudoF
- IDF global guideline: https://bit.ly/2pCXMIz
- Lester Cardiometabolic Health Resource: https://bit.ly/2L5zaTQ
- MHRA guidance on risk of DKA with SGLT2 inhibitors: https://bit.ly/2EV6mK9
Insulin initiation
Jane Diggle, Specialist Practitioner Practice Nurse, West Yorkshire
- Of the 3.9 million people with diabetes in the UK, around one third are treated with insulin, including the rapidly increasing numbers with type 2 diabetes. This places increasing demands on specialist diabetes services and on GPs and practice nurses, who have greatly expanded their role in supporting people on insulin.
- Many people with type 2 diabetes eventually require insulin to achieve satisfactory glycaemic control. Insulin deficiency occurs gradually in type 2 diabetes, so the optimal time to begin the therapy is not clearly defined or easily recognised.
- Despite NICE (2015b) positioning of insulin in the NG28 treatment algorithm, in practice there are often delays of years and very high HbA1c levels before insulin is commenced.
- Healthcare provider and patient barriers to insulin therapy exist. Useful tips for overcoming resistance include: talking about insulin early, demonstrating the pen devices, giving patients the opportunity to try a “dummy” injection, dispelling myths (e.g. the need for insulin signifies personal failure) and making sure that conversion to insulin is never used as a threat.
- When starting regimens, highlight the pros and cons of once-daily basal insulin versus twice-daily pre-mixed options, provide practical advice on safe starting doses and share helpful self-titration algorithms with patients.
- For those on insulin therapy, SMBG is important to guide dose titration, identify hypoglycaemia, support safe driving and provide valuable information on the impact of dietary choices.
- Correctly used, insulin offers huge benefits, but it is a potent drug and has the potential to cause significant harm. There is potential to combine insulin with other blood glucose agents, particularly those with weight loss benefits, to mitigate the weight gain that is often associated with insulin therapy.
- The reduction in insulin doses that can be achieved with SGLT2 inhibitor use may increase the risk of DKA with this combination of therapies. It is important to counsel patients about the signs and symptoms of DKA, when it is appropriate to stop an SGLT2 inhibitor and, most importantly, when to seek urgent medical assistance.
- Structured education is recommended for everyone with diabetes in order to help people make decisions about diet and lifestyle.
Insulin – management considerations
Su Down, Nurse Consultant in Diabetes, Somerset
- Injection technique and care of injection sites are as important as the insulin prescribed.
- Always inspect and palpate injection sites to identify lipohypertrophy. Insulin absorption from these sites is unpredictable, so ensure other sites are used for injections.
- Ensure people understand never to omit insulin when they are sick, even if they are not eating normally – often more insulin is needed rather than less. Ensure everyone on insulin has a copy of a sick-day rules leaflet to refer to when ill.
- There are more than 30 different insulins available in the UK – many have similar sounding names but very different actions. Ensure you are familiar with the action of those you prescribe.
- Ensure you are familiar with the DVLA guidance and that people using insulin know to notify the DVLA.
- Patients with deteriorating renal function are at increased risk of hypoglycaemia as renal clearance of insulin decreases. This is particularly important when eGFR is <45 mL/min/1.73 m2.
- Insulin combined with a GLP-1 receptor agonist is available (e.g. as iDegLira [liraglutide and insulin degludec]). Titration is by “dose steps”, which are a combination of each product.
- U100, U200 and U300 insulins are now available, increasing the risk of overdose if confused. Insulin must never be withdrawn from a pen cartridge or pen for administration using an insulin syringe – pens automatically calculate the dose of insulins of different concentrations and this is not possible using standard U100 insulin syringes.
- Biosimilar insulins, such as Abasaglar, are now available. These are not bioequivalent to other forms of insulin glargine. All insulins should be prescribed by brand name to prevent substitution at the point of dispensing.
- Consider when de-escalation of insulin therapy is appropriate, particularly in the frail elderly and those with hypoglycaemia.
Apply to practice
Simple audits:
- Audit your insulin prescriptions for any generic insulin and amend these to brand names to ensure the same brand is dispensed.
- Search for those over 75 years on insulin or sulfonylureas with HbA1c <58 mmol/mol and review whether de-escalation is appropriate.
Guidelines and resources
- The Six Steps to Insulin Safety – everyone who prescribes insulin should complete this module, even if they do not initiate or titrate insulin: https://diabetesonthenet.com/course
- TREND-UK Sick-day rules leaflet: https://bit.ly/2IvDE4I
- DVLA fitness to drive guidance: https://bit.ly/2GroY4H
Diabetes Shorts: Pumps in primary care
Paul Newman, GP, Glasgow
- It is important to understand the potential roles of primary care. These include providing emergency kit (including insulin, glucose and ketone test strips, and other supplies that are prescribable) and helping to diagnose and admit with DKA if the specialist team is unavailable.
- Indications for referral for an insulin pump are nocturnal hypoglycaemia, frequent mild hypoglycaemia, reduced hypoglycaemia awareness and difficulty managing physical activities.
- Pumps contain a reservoir of rapid-acting insulin. This is delivered subcutaneously as a continuous infusion at a basal rate and in bolus doses that are administered when consuming carbohydrate or to correct blood glucose levels that are outside of the desired range.
- Bolus doses can be set by the user or calculated by the bolus wizard setting on pump. With both, accurate carbohydrate counting is essential.
- Advantages to pump use should be: better control, with a more stable blood glucose profile and fewer hypos; significantly improved flexibility for activity and travel; and fewer injections.
- Disadvantages include: the very hard initial work (a 2-week training course is required); the rapid deterioration of blood glucose control if the pump malfunctions and the increased risk of DKA (ketones appear within 4 hours of pump failure); concealment; and there can be occasional supply problems.
- If blood glucose is >14 mmol/L, pump users need to follow a DKA protocol that includes administering a bolus of short-acting insulin from a pen, replacing insulin and disposables related to the pump, testing for ketones and seeking help.
- Continuous interstitial glucose monitoring via a body sensor provides frequent estimates of glucose, but needs to be calibrated with a blood glucose measurement at least every 12 hours. There is a 5–12-minute lag phase compared to blood glucose testing. Currently blood glucose testing is still needed before driving.





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025