Diabetes in Wales today
Julia Platts, National Clinical Lead for Diabetes in Wales
COVID-19
- COVID-19 has led to the suspension of many services and a significant backlog of care needs, but urgent services have continued.
- The situation has led to innovative ways of working and an opportunity to alter services for the better.
- Ways to combat isolation and depression, and to share important diabetes-related information for those without internet access need exploration – local and national radio broadcasts may work well.
- During the first wave of infections, the major criticism was the lack of communication.
- We know that, for many people, not seeking timely help is more risky than the possible exposure to COVID-19. We need to disseminate sick-day rules and provide guidance on who and when to contact, to all who need them.
- Welsh retinopathy screening was suspended in March, but restarted for high-risk groups from mid-September. Where this is not accessible, consider whether local opticians may be able to undertake it in the short term. This is not an official policy, but is worth exploring.
- Practices are encouraged to risk-stratify people with diabetes, as per the Wales prioritisation strategy, and to see those in the “red group” within 3 months and the “amber group” within 6 months. Ensure that those in the “green group” know to continue with current management plans and when to seek advice.
- Remote working and point-of-care HbA1c testing in car parks have been developed to reduce face-to-face contact. Home blood pressure monitoring and use of the Touch the Toes Test for foot assessment have also been used.
- It is important to empower people with foot problems. In the event of a “foot attack” – people need to have a contact number and be able to access specialist advice and care immediately (see Footnote). Delivery of such care has continued throughout the pandemic.
Ongoing initiatives across Wales
- The Association of British Clinical Diabetologist audit demonstrated improved control, decreased hypoglycaemia and decreased admissions in those using the Freestyle Libre system. 52% of those with type 1 diabetes in Wales use this technology. It can be initiated in people with type 1 diabetes remotely by emailing local diabetes units.
- The Value Based Health Care programme continues to explore ways to deliver care differently. This includes revisiting pathways for endpoints such as amputation, adverse pregnancy outcomes and retinopathy, and exploring different models of care.
- The Welsh Information Solution for Diabetes Management (WISDM) is being rolled out slowly.
- The National Diabetes Audit provides useful data, but currently these data are not easily accessible so exploring ways to access it is important.
- Empowerment is the bedrock of any system and, just before the pandemic, group consultations and peer-support models were being explored. Online X-PERT, DAFNE and DESMOND programmes have been developed. Development of PocketMedic videos continues.
- The value of support groups and apps for those with type 1 diabetes has been demonstrated (e.g. SEREN Connect for those aged 16–25 years and DigiBete for under-25s).
- Prevention: Brief intervention, as piloted in a programme across the Swansea Bay area, is cost effective at £44 per person. Discussions with Public Health Wales and the Strategic Programme for Primary Care are ongoing.
- Remission: Across Wales, four pilot remission schemes are underway for those within 6 years of a diagnosis of type 2 diabetes and with a BMI of 27–45, using remote starts.
- Pre-conception care: A new email and telephone service is being piloted by the Cardiff and Vale University Health Board that provides advice from dedicated diabetes specialist nurses who can liaise with local services. All women with type 1 diabetes should have access to continuous glucose monitoring during pregnancy.
- Microalbuminuria screening is as important as retinopathy screening – if we don’t measure it, we are missing opportunities for nephroprotection and reducing cardiovascular disease. A pilot study is underway to establish whether a centralised pathway to undertake this might have benefit. Rates of albuminuria screening are currently low – 31% for type 1 and 57% for type 2 diabetes.
Emotional wellbeing and engagement
Rose Stewart, Principal Clinical Psychologist, Betsi Cadwaladr University Health Board
- The psychological consequences of COVID-19 on people with diabetes and their healthcare professionals will be significant. Mental health services are already observing increases in demand, and this is likely to be sustained as the economic impacts of the pandemic continue to affect the country.
- Particularly vulnerable groups include young adults, people with existing mental health issues, people from low socioeconomic status backgrounds and healthcare staff. Those with a new diagnosis of diabetes will also be vulnerable to increased levels of distress. Services need to be proactive in identifying these vulnerable people and offering them additional support.
- There are many resources and organisations that can support healthcare professionals and the people with diabetes that they work with. Multiple resources specifically aimed at promoting psychological wellbeing for people with diabetes during the pandemic have been developed. These are signposted within the presentation and are summarised below. For those with an NHS Wales email address, there are additional resources on the NHS Wales SharePoint site. Please take the time to get familiar with them and use them.
- As a healthcare professional, please remember that you are not alone; NHS staff-support services will be open to primary care. Many of us survived the first wave of the pandemic on adrenaline alone, which is not sustainable in the longer term. Investing time in self-care will help to boost your resilience and increase your efficacy as a practitioner.
Resources
For you
- Supporting our people. NHS support to help its staff manage their health and wellbeing: https://people.nhs.uk
- NHS staff support line: 0300 131 7000
- PocketMedic films to “prescribe”: https://pocketmedic.org
- Diabetes UK mood prescription: bit.ly/38WvToq
For patients
- Talking Type 1 range of self-help booklets (see bit.ly/3fnV5FD). To order, email [email protected]
- Diabetes Psychology Matters. Information, news and resources: https://diabetespsychologymatters.com
- NHS Library mental health apps: bit.ly/36M7xen
- NHS diabetes advice helpline: 0345 123 2399
Frailty and diabetes
Clare Hambling, GP, PCDS Chair
Frailty and diabetes
Frailty is a medical syndrome with multiple causes and contributors, characterised by diminished strength, endurance, and physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death.
- There is a positive association between advancing frailty and adverse outcomes from COVID-19 infection.
- Frailty is distinct from multimorbidity, but multimorbidity contributes to it. The burden of multimorbidity increases with advancing age.
- Sarcopenia (loss of muscle mass with ageing) is a major contributor to frailty. It leads to poor health outcomes, reduced mobility, loss of functional capacity and increased risk of falls.
- Factors contributing to sarcopenia include poor nutrition and dentition, and low physical activity. Frailty is just as common in people who are overweight as in those who are underweight, as muscle weight is the important factor.
- In the context of type 2 diabetes, peripheral insulin resistance contributes to sarcopenia, which in turn leads to further increases in insulin resistance, leading to hyperglycaemia.
- It is important to identify those at risk and offer interventions to halt or reverse the progression of frailty.
Assessing frailty in primary care
- There are a number of tools that can be used, many of which include an assessment of walking speed.
- Tip: Walk with your patient to the clinical examination room to assess functional capacity and signs of frailty.
- The Electronic Frailty Index (eFI) pulls information from the clinical database and uses the read codes to calculate a frailty score. It can also be used to look at frailty from a population point of view.
- At the level of the individual, use the Clinical Frailty Scale (CFS). It is easy to use, descriptive and the person being assessed can be fitted into the appropriate level quickly (bit.ly/2VBzXUj).
- There is also a CFS app. This presents a series of yes/no questions that lead to a result and clinical prompts.
Hypo- and hyperglycaemia in older people
- Older people are very vulnerable to hypoglycaemia and its consequences, often suffering serious harm such as fractures, head injuries and cardiac events. It results in significant mortality, cognitive decline and dementia, and longer-term cardiovascular disease events.
- Risk factors for hypoglycaemia include advancing age and duration of diabetes; certain comorbidities, including renal disease and cognitive impairment; polypharmacy, particularly insulin and sulfonylurea therapies; and a delayed recognition of its onset. In some, confusion may be mistaken for normal cognitive impairment.
- There has been a trend to relax glycaemic targets, but hyperglycaemia can be harmful too. It puts people at risk of acute diabetes emergencies, diabetes-related complications, infections and the consequence of geriatric syndromes.
Setting holistic glycaemic targets
- Strike a balance when setting clinically appropriate glycaemic targets (see Hambling et al, 2019). Factors to consider:
- Physical: diabetes, multimorbidity, polypharmacy, therapeutics.
- Psychological: cognitive function, emotional wellbeing.
- Functional: disability, frailty, geriatric syndromes, functional status.
- Social: social circumstances, anticipated change.
- Older people often experience changes in their clinical or functional wellbeing, or in their social support, which can lead to a marked change in their general health.
- Once all factors have been taken into account, an individual’s functional status and needs can be considered, and an appropriate glycaemic goal agreed (see Table 1).
- It is appropriate when managing those with very complex needs to relax glycaemic targets, while also avoiding hyperglycaemia.
Medicines optimisation and deprescribing
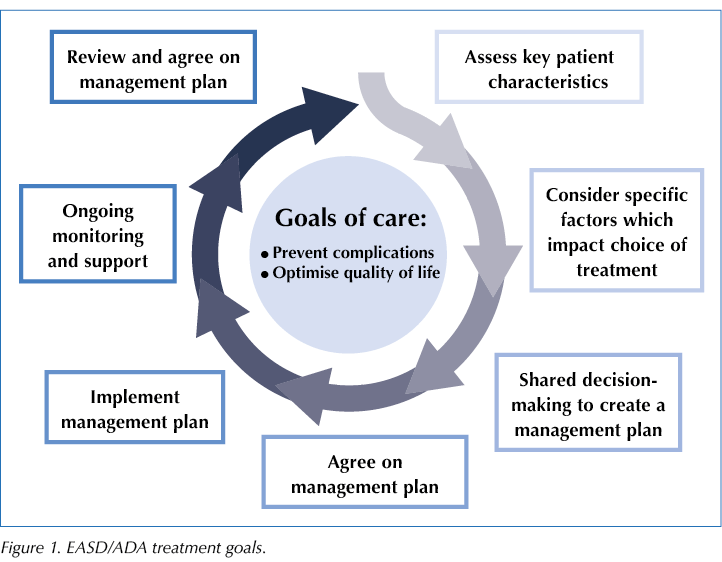
- The EASD/ADA decision cycle should be applied to person-centred glucose-management in type 2 diabetes (see Figure 1).
- NICE has a pathway for medicines optimisation that takes account of a number of factors (https://pathways.nice.org.uk/pathways/medicines-optimisation). With an older person with frailty, involve their family or carers in a review.
- As an individual gets older, the risk of a particular therapy may start to outweigh the benefit. At this point, consider deprescribing.
- Consider all drugs. Look at medications with anticholinergic properties, drug–drug interactions, drugs altering muscle power, drug-induced hyponatraemia or dehydration, and potential overtreatment with blood pressure and/or glucose-lowering medications.
- Sulfonylureas and insulins risk causing hypoglycaemia. In type 1 diabetes, review the insulin regimen and simplify, if necessary. In type 2 diabetes, limit the use of sulfonylureas, if possible.
- All glucose-lowering therapies can cause hypoglycaemic episodes, particularly when used in combination, and may carry other risks.
- Most glucose-lowering drugs require adjustment as renal impairment increases; some may precipitate or exacerbate heart failure (particularly saxagliptin and pioglitazone); SGLT2 inhibitors risk volume depletion; and SGLT2 inhibitors and GLP-1 receptor agonists promote weight loss, which may not be beneficial in frailty.
- However, glucose-lowering medications may have other added benefit, such as in established cardiovascular disease, heart failure and comorbidities where weight loss could be beneficial.
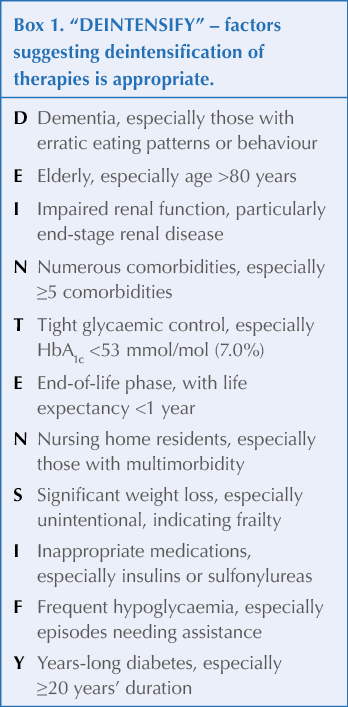
- In the context of overtreatment with glucose-lowering therapies, the DEINTENSIFY mnemonic highlights the factors that suggest a deintensification or step-down of therapies would be appropriate (see Box 1).
- Make sure that a mechanism to ensure early monitoring and review is in place to avoid rebound hyperglycaemia.
.png)





Risk ratios of 1.25 for autism spectrum disorder and 1.30 for ADHD observed in offspring of mothers with diabetes in pregnancy.
18 Jun 2025