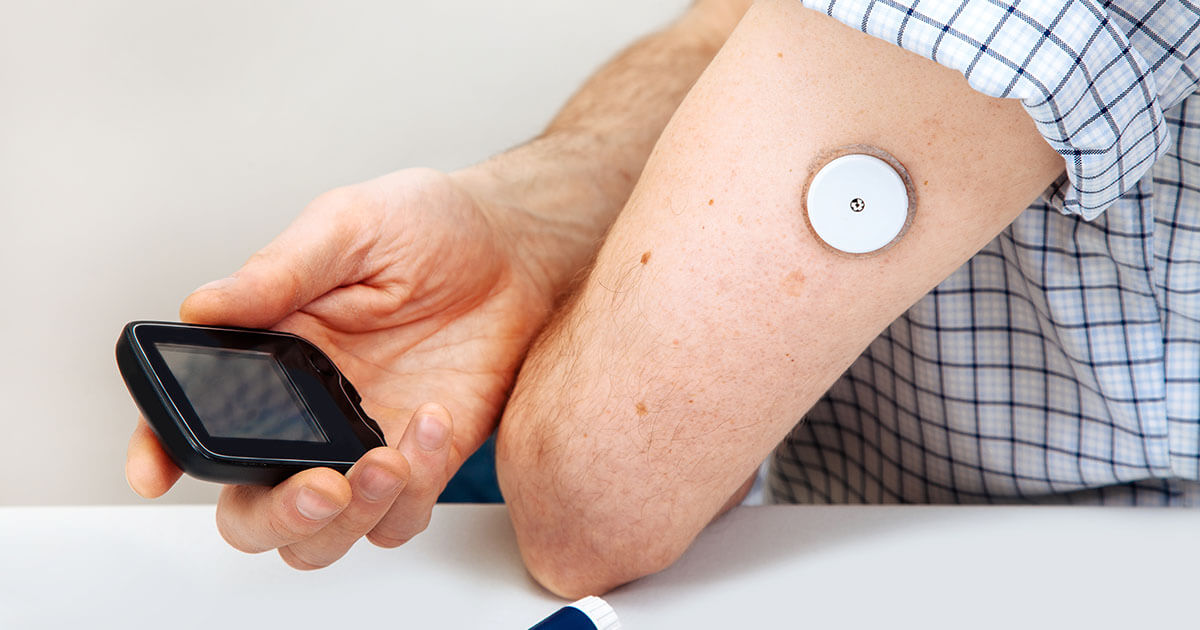
The FLASH-UK trial, funded by Diabetes UK, was an open-label, parallel-group randomised controlled trial of intermittently scanned continuous glucose monitoring (isCGM), with optional alarms, versus fingerprick self-monitoring of blood glucose in people with type 1 diabetes and suboptimal glycaemic control. A total of 156 people with type 1 diabetes (age >16 years, HbA1c 59–97 mmol/mol [7.5–11.0%]) were randomised 1:1 to either the FreeStyle Libre 2 or fingerprick monitoring for 24 weeks.
The mean age of participants was 44 years and the mean diabetes duration was 21 years. At 24 weeks, mean HbA1c fell from 72 to 63 mmol/mol in the intervention group, compared with a reduction from 69 to 67 mmol/mol in the control group (between-group difference 5.5 mmol/mol). The isCGM group were 2.47 times more likely to achieve an HbA1c ≤59 mmol/mol and 4.30 times more likely to reduce their HbA1c by 11 mmol/mol or more. Time in range increased by 9%, or 130 minutes, per day compared with the control group.
Mean Diabetes Treatment Satisfaction Questionnaire (DTSQ) scores were 7 points higher (out of a possible 36) in the isCGM arm; however, other participant-reported outcomes, including scores related to diabetes, depression, fear of injections/testing and eating behaviours, were not significantly different between the groups. The incidence of adverse events was low in both groups.
The trial was limited by an open-label design and the predominantly White ethnicity of the participants, which may limit generalisability. Furthermore, a lack of data on participants’ use of alarms means it is unknown what role, if any, the optional alarms had on these results. Nonetheless, the results demonstrate the effectiveness of isCGM in people with high HbA1c.





Amid accumulating evidence of benefits with new diabetes drugs, Vinod Patel asks whether the costs can be justified.
9 Nov 2023