It is recommended that children and young people (CYP) with type 1 diabetes should access ongoing education for self-management of their diabetes, including carbohydrate counting (Phelan et al, 2018). Effective self-care is essential for CYP with type 1 diabetes and, depending on age and developmental needs, self-care is administered either by parents/carers or by the CYP with adult support. Families must be supported to implement medical advice regarding metabolic control goals (American Diabetes Association, 2018).
Diabetes self-care requires knowledge of blood glucose and of the effects that diet, insulin and exercise have on that individual child. As CYP grow and mature, they typically take an increasing amount of responsibility for their own care; thus, diabetes education programmes need to be repeated and be age-appropriate to take into consideration changing developmental stages (Phelan et al, 2018). The Royal College of Paediatrics and Child Health (RCPCH, 2017) states that education should be provided on an ongoing basis, including outside of outpatient clinics, throughout the CYP’s time within the paediatric diabetes service. Level 3 carbohydrate counting education should occur from diagnosis of type 1 diabetes (Smart et al, 2018) and be delivered in an age-appropriate way, targeted at the CYP as they transition towards adulthood and independence (Phelan et al, 2018).
The Cook and Eat programme in the Exeter Children and Young People’s Diabetes Service (ExCYPDS) commenced in 2015 for CYP and their friends or families. It is a group programme designed to engage CYP in food preparation, cooking skills and education, based on the principles of carbohydrate counting, in a real-life setting (Leveridge et al, 2017; 2021). “Family Fun” sessions (for primary-school-aged children, attending with parents and siblings) occur in summer holidays. “Fun” sessions (for secondary-school-age CYP, attending with friends) occur during term time and half-term holidays. CYP build on mathematical skills as these develop alongside the National Curriculum. Attendees get a new recipe to trial each year, make food to take home (or eat within the session) and have a chance to meet others living with type 1 diabetes. Sessions are an open forum for families to ask questions to healthcare professionals or peers.
The RCPCH (2017) states that multidisciplinary teams should evaluate their education programmes to ensure they meet the needs of their targeted population. Informal parent/carer and CYP feedback for the Cook and Eat programme was positive (Leveridge et al, 2017); however, consideration also needs to be given to the impact of ongoing carbohydrate counting education on clinical outcomes, such as BMI, hypoglycaemia frequency and HbA1c. Enhancing diabetes knowledge is perceived as one influential factor in reducing HbA1c levels and, thus, decreasing the risk of later microvascular complications (Phelan et al, 2018).
The impact of group-based cooking and education on HbA1c are unknown. Therefore, this article describes the demographics and HbA1c outcomes in Cook and Eat attendees compared with non-attendees, as part of the retrospective service evaluation of five years of face-to-face group sessions.
Method
All CYP aged 16 years or under who attended Cook and Eat between 1 April 2015 and 31 March 2020 were included in the analysis and matched, based on age and time since diagnosis, to CYP within the service who had never attended sessions.
Over the 5 years, CYP could attend up to six sessions as, to aid school transition, they were invited to attend in their final year of primary school summer holidays and again within the first two terms of secondary school. This means some attendees attended twice within the same audit year.
HbA1c levels were captured from National Paediatric Diabetes Audit (NPDA) raw data. CYP were excluded from the analysis if there was no record of their HbA1c in the NPDA audit year. HbA1c data within the first 6 months from date of diagnosis were excluded in both groups due to stabilisation of glucose levels immediately after diagnosis and to be consistent with NPDA data analysis.
Demographic data and HbA1c were collated from the NPDA raw data. For each matched pair, HbA1c data were collected from the date that the attendee first participated in a Cook and Eat group and continued until 31 March 2020. Each CYP’s (attendees’ and matched non-attendees’) mean annual HbA1c levels (from up to six tests per year) were calculated for each NPDA audit year. This annual mean HbA1c was used in further analysis between Cook and Eat attendees and non-attendees. Duration of type 1 diabetes for attendees and matched non-attendees was calculated from the date the attendee first attended a Cook and Eat session.
Statistical analysis
One-way independent ANOVA was used to determine whether the number of years attended affected HbA1cvalues in the most recent year (2019/20). A two-way repeated-measures ANOVA was run on mean yearly HbA1c values to compare those who first attended in primary school compared to those who first attended in secondary school. A further two-way repeated-measures ANOVA was run on mean yearly HbA1c values to compare attendees and non-attendees. Mauchly’s test of sphericity was run to determine sphericity, and if violated, Greenhouse–Geisser corrections were applied. Bonferroni post hoc analysis was used where there was a significant main effect. Statistical analyses were conducted on SPSS Statistics version 28 (IBM Corp., Armonk, NY, USA), with statistical significance accepted at a level of P<0.05.
Results
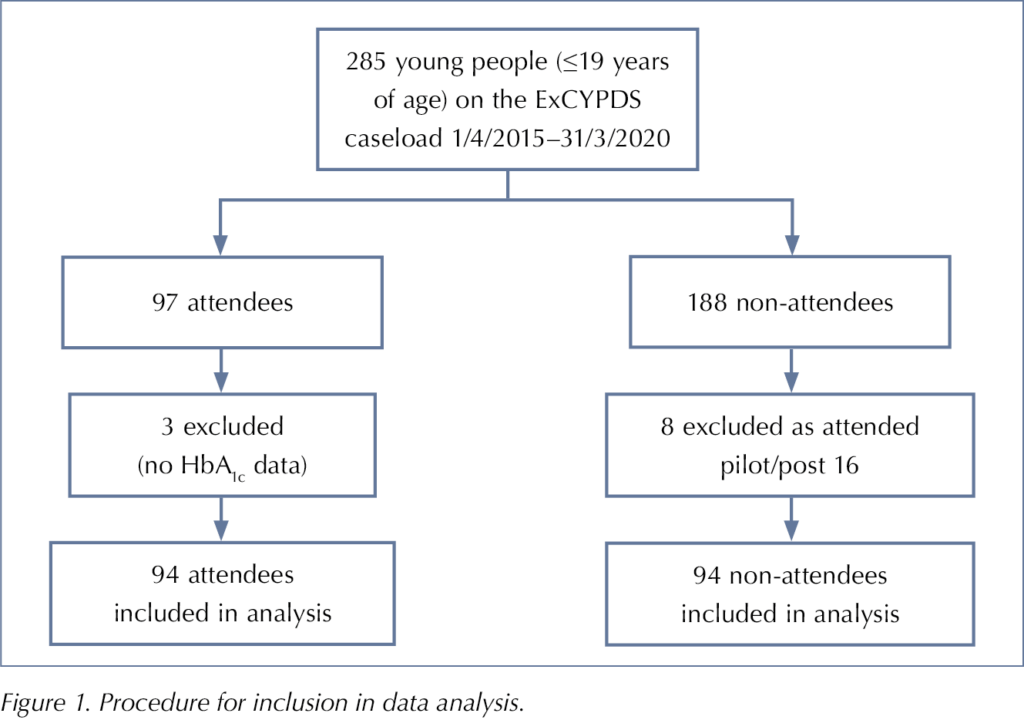
There were 285 eligible CYP with type 1 diabetes on the ExCYPDS caseload over the study period, 97 of whom attended at least one Cook and Eat session (Figure 1). Three attendees were excluded due to insufficient HbA1c data for analysis and, therefore, 94 Cook and Eat attendees were included in the analysis. Of the 188 CYP who did not attend a Cook and Eat session, eight were excluded from the analysis as they had attended a Cook and Eat pilot or a post-16 session. Ninety-four CYP were selected for analysis as non-attendees based on a similar age and diabetes duration to an attendee.
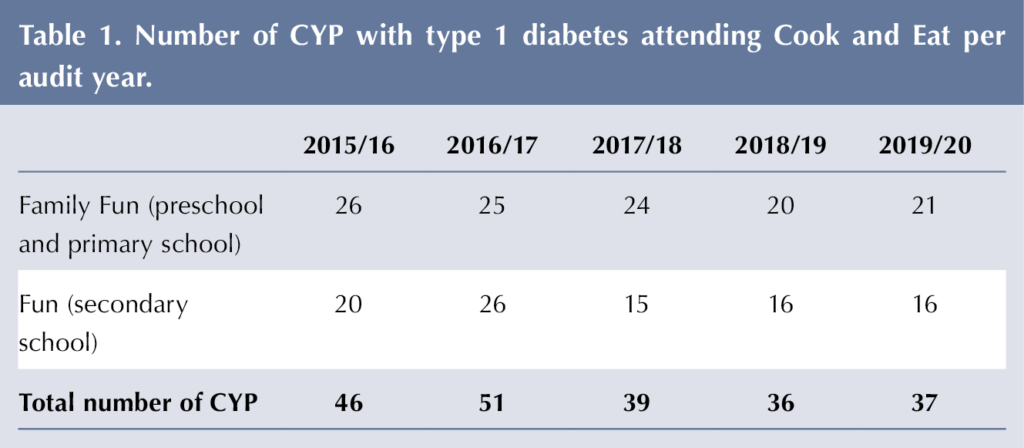
Thirty-one Family Fun (pre-school and primary school) sessions and 44 Fun (secondary school) sessions were held between 27 August 2015 and 18 February 2020. The numbers of CYP with type 1 diabetes attending Cook and Eat per audit year are detailed in Table 1. A total of 364 people (including siblings, parents or carers) attended Family Fun sessions and 157 (including friends) attended the Fun sessions. Thirty-six after-school secondary Fun sessions were held in eighteen schools (CYP attended in their own school) and eight in half-term (double-session in a local school). Many of the 97 CYP with type 1 diabetes attended multiple times, so there were 209 attendances at Cook and Eat sessions over the 5 years.
Demographics of attendees and non-attendees
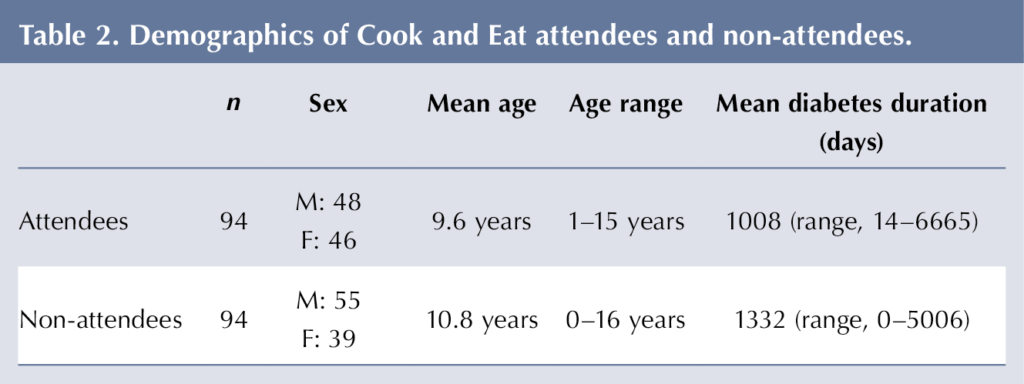
Similar numbers of males and females accessed Cook and Eat (Table 2); however, more males were represented in the non-attendee than attendee group. Ages across the two groups were similar. The mean diabetes duration of attendees was lower that of non-attendees.
HbA1c data
The number of HbA1c tests analysed for attendees and non-attendees is shown in Table 3. More HbA1c values were available for analysis in the attendee (n=333) than non-attendee (n=294) groups. The difference in the number of HbA1c tests is partially explained by 22 (23.4%) of the non-attendees being diagnosed after the age-matched attendee had attended their first Cook and Eat session.
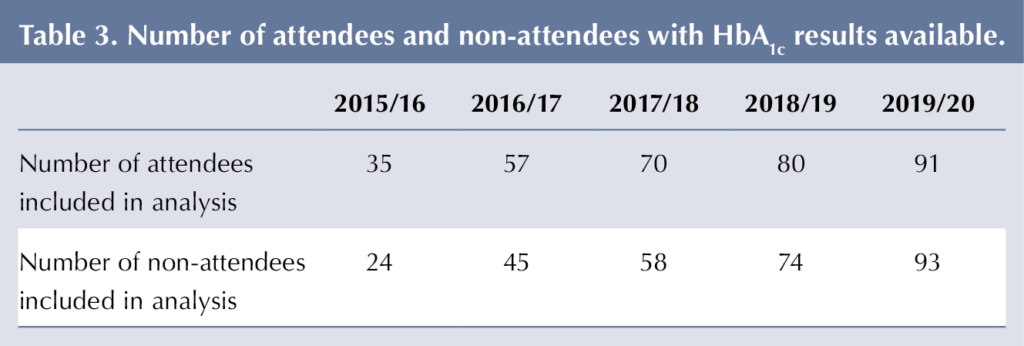
Table 4 shows that both attendees’ and non-attendees’ mean HbA1c increased after 2017/18. This is consistent with the whole-caseload increase in HbA1c in the nationally reported NPDA ExCYPDS (PZ060) caseload-adjusted mean and median (Table 5). Adjustment by the NPDA uses a logistic regression model taking into consideration patient characteristics (deprivation, age, gender, duration of diabetes and ethnicity), and this was not applied to Cook and Eat data.
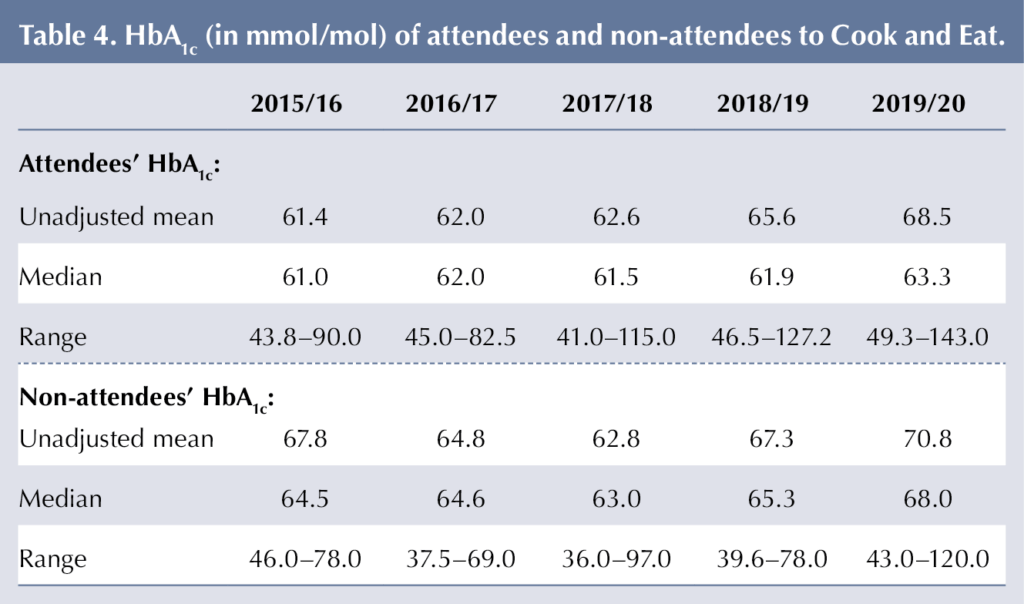
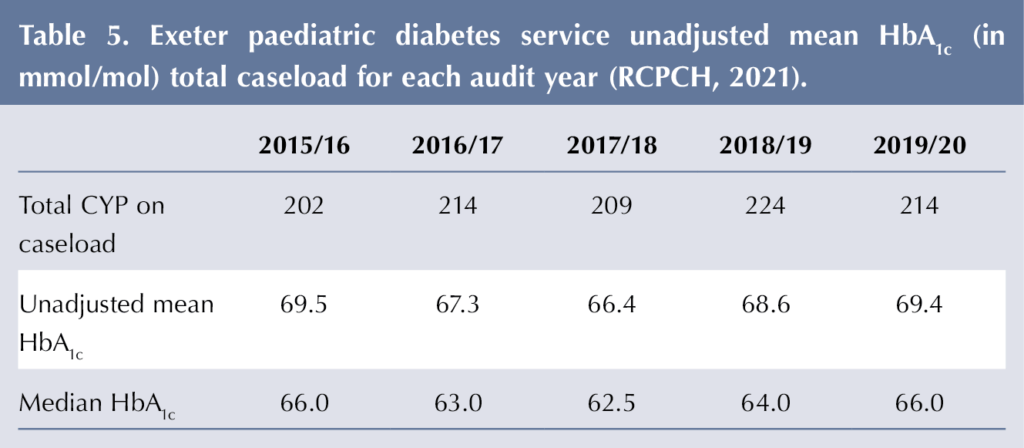
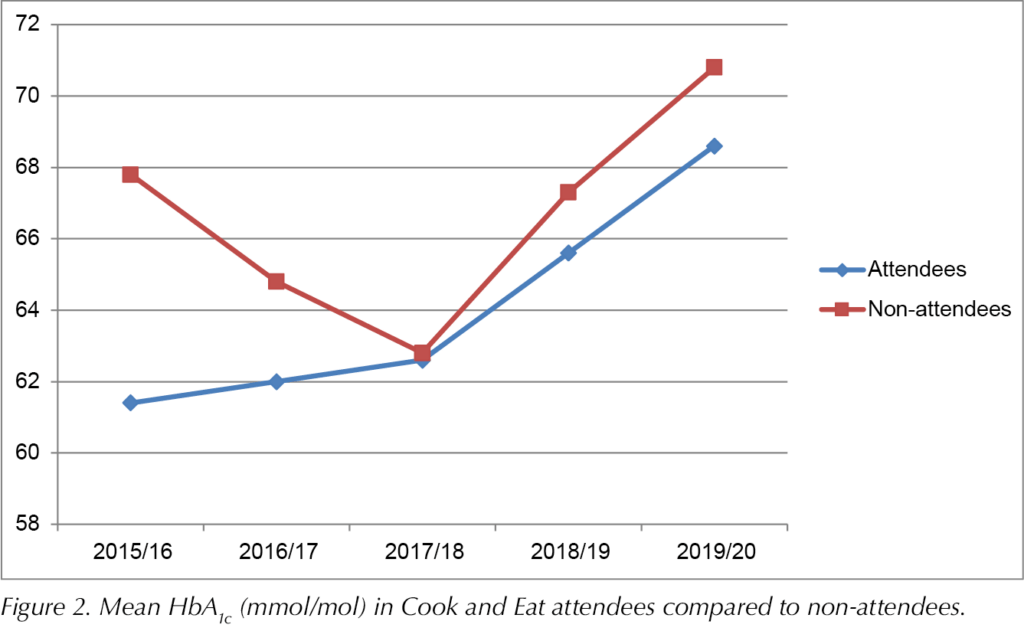
Figure 2 shows the mean HbA1c of group attendees and age-matched non-attendees per audit year. There was no group/time interaction, so no significant differences in HbA1c values between groups were identified at any time point (P=0.366). There was a significant effect of time (P=0.007). Bonferroni post hoc analyses revealed an increase in HbA1c of 6.4 mmol/mol from 2015/16 to 2019/20 (P=0.034). HbA1c increased by 7.6 mmol/mol from 2016/17 to 2019/20 (P=0.003). From 2017/18, HbA1c increased by 3.6 mmol/mol to 2018/19 (P=0.002), and by 9.1 mmol/mol to 2019/20 (P<0.001). From 2018/19, HbA1c increased by 5.4 mmol/mol to 2019/20 (P<0.001).
Repeated attendance and HbA1c
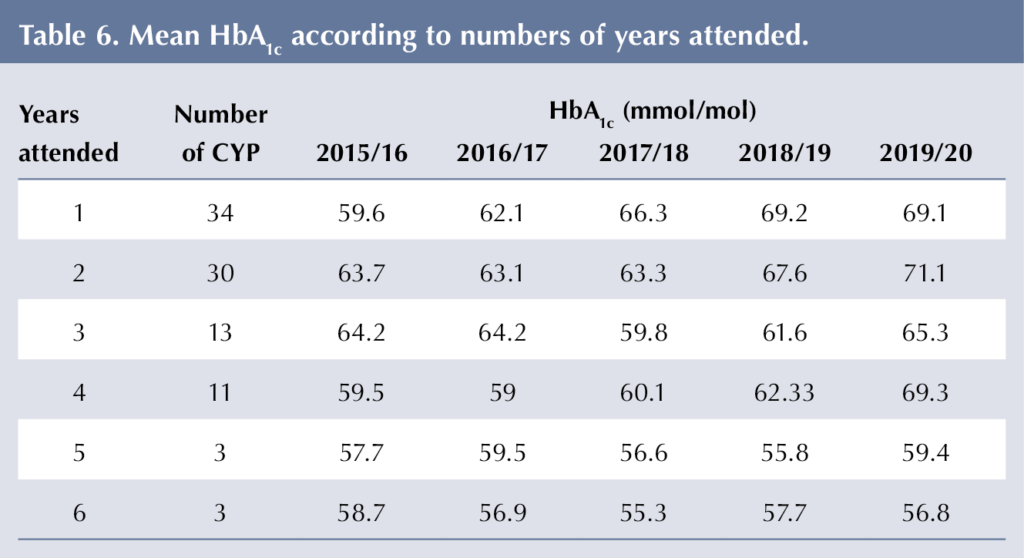
Sixty (63.8%) CYP attended Cook and Eat groups on more than one year. It was more common for CYP to attend for one or two years than for three or more (Table 6). There was no significant difference in 2019/20 HbA1c values between those who attended Cook and Eat for 1, 2, 3, 4, 5 or 6 sessions (P=0.734).
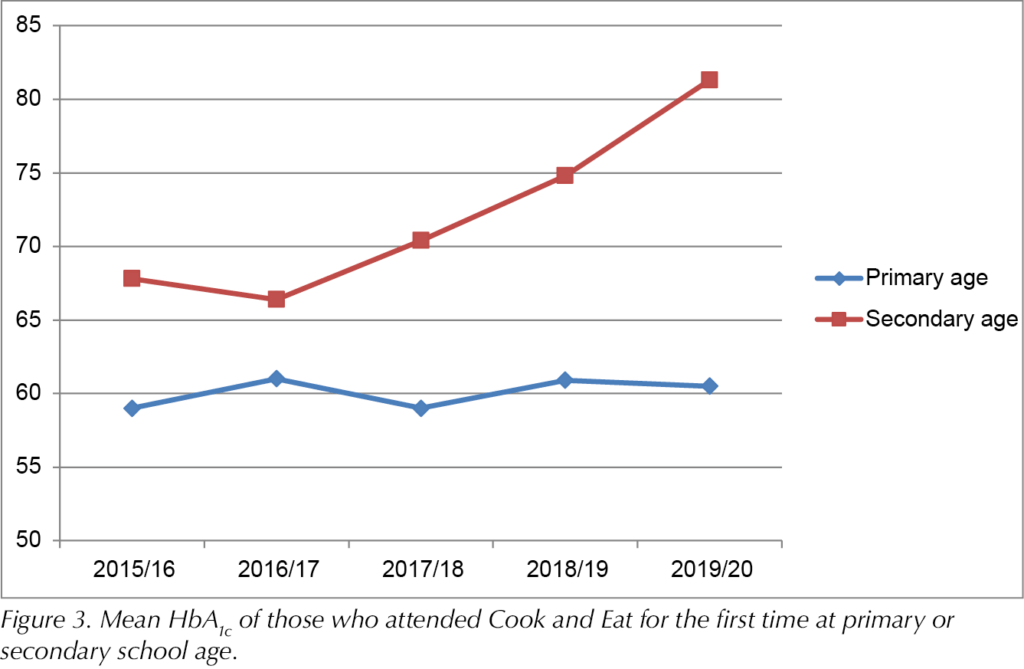
Sixty-six CYP attended their first session while at primary school age (average age, 8.2 years), while 28 attended their first session whilst in secondary school (average age, 13.1 years). There was no group/time interaction, and thus no significant differences in HbA1c values between starting in primary school or secondary school, at any time point (P=0.055). However, there was a significant effect of time (P<0.001), with HbA1cincreasing over time (Figure 3). Bonferroni post hoc analyses revealed an increase of 11.1 mmol/mol from 2015/16 to 2019/20 (P=0.01). HbA1c increased by 11.7 mmol/mol from 2016/17 to 2019/20 (P=0.004). From 2017/18, HbA1c increased by 4.4 mmol/mol to 2018/19 (P=0.045), and by 12.1 mmol/mol to 2019/20 (P<0.001). From 2018/19, HbA1c increased by 7.7 mmol/mol to 2019/20 (P<0.001). It appears that those who commenced at primary school age remained more consistent in their HbA1c level over time compared to those who commenced at secondary school age.
Discussion
There was no difference in mean HbA1c between attendees and non-attendees of the Cook and Eat (carbohydrate counting) education sessions. However, group participation appeared to be linked to a slower increase in HbA1c than that observed within the overall patient cohort.
CYP who joined Cook and Eat during primary school years tended to have a lower HbA1c than those joining for the first time in secondary school. It is also noted that HbA1c did not rise as sharply over time in the CYP who began attending at primary school age as it did in those who commenced Cook and Eat in secondary school; this reflects the established finding that HbA1c typically increases in adolescent years (RCPCH, 2021).
Findings were also suggestive that repeat attendance was associated with lower HbA1c. It is hypothesised that there may be a protective effect of ongoing engagement with level 3 carbohydrate counting education and confidence building as young people move towards independence in nutrition-related diabetes tasks. However, the low number of attendees who attended 5–6 times (n=3) limits the opportunity to draw clearer conclusions.
Caution needs to be taken when interpreting these findings; there are limitations due to the cohort size and demographics related to the matching of attendees and non-attendees. While attendees and non-attendees were matched in terms of age, it was not consistently possible to match by other factors such as gender or diabetes duration. Additionally, some of the matched non-attendees were diagnosed after the attendee’s first group attendance, contributing to the lower number of HbA1c measurements in the non-attendee group.
In addition to limitations in data availability, it is important to consider that HbA1c is affected by a multitude of factors, including insulin treatment, psychological distress, social circumstances and duration of diabetes (DiMeglio et al, 2018). Thus, within the cultural context of a strong focus on HbA1c, the large and varied number of factors influencing HbA1c should not be discounted. It seems problematic both to make assumptions that Cook and Eat attendance was the only factor that influenced HbA1c and, conversely, to only evaluate the value of group education based on HbA1c changes.
Just as HbA1c is affected by multiple factors, the impacts and value of structured education programmes such as Cook and Eat are multifactorial; overly focusing on HbA1c outcomes limits consideration of the holistic value of group education and may prevent understanding of how group participation interacts with HbA1c. It is challenging to scientifically evaluate education programmes (Lange et al, 2012), and classical double-blind randomised controlled trial programmes are difficult to apply to education, an indispensable part of standard care.
More than half of the CYP who went to Cook and Eat attended multiple times, with some young people attending every year; this strongly suggests that CYP and their families consider the content valuable and enjoy the sessions. Seeking to understand what attendees and their families and friends value about Cook and Eat, and what increases accessibility, may refine the sessions and further enhance potential benefits of participation on HbA1c and other clinical outcomes.
Previous research suggests that CYP value practical and engaging brief group education sessions held outside the hospital and which are strength-orientated, focusing on what they can, rather than cannot, do (Chaney et al, 2012; Coates et al, 2013). Cook and Eat sessions are run in a way consistent with this research. Additionally, a focus group of CYP and parents in the Yorkshire and Humber region reported learning more from others with type 1 diabetes than from healthcare professionals (Kime, 2014). Cook and Eat groups encourage dynamic discussion and peer-to-peer learning as well as level 3 carbohydrate counting. However, as the Cook and Eat sessions in Exeter are yet to be more formally evaluated, detailed attendee perspectives are unknown.
The involvement of family members and peers may be important to attendees engaging with Cook and Eat sessions and the benefits of the sessions in terms of HbA1c. Therefore, future research should aim to determine the relationship between involvement of family members, peers and HbA1c.
Cook and Eat Family Fun (primary school age) includes parents/carers and siblings. Everyday engagement by parents is a positive determinant of the health and wellbeing of that child (Boman et al, 2012). However, Chaney et al (2012) reported that adolescents prefer education without their parents, as they appreciate that they will have to cope when they are at university or leave home. CYP enjoyed bringing their peers to Cook and Eat in secondary sessions (Leveridge et al, 2017), while larger groups generated more broad discussion around living with diabetes and led their peers without diabetes to understand more about their condition and increase their support.
In addition to understanding what attendees value about Cook and Eat sessions in order to further enhance engagement and potentially improve clinical outcomes, including HbA1c, it is important to consider what impacts participation. While it is hoped that the sessions being free and held locally to the child increases accessibility, not all CYP on the ExCYPDS caseload access group education in the form of Cook and Eat. Previous research shows that those who attend group education find it helpful (Christie et al, 2016; Kime, 2014), although many may be reluctant to join group interventions and prefer individual sessions (Price et al, 2016).
Coates et al (2013) describe potential barriers to education session engagement, including CYP being unable to get time off school, gaining education from other sources or already feeling able to cope. Cook and Eat attempted to address some of these issues by offering sessions in and outside of school times and by providing resources for the sessions. Those who do attend structured education may be the most engaged, well-informed families or more resourced families, so sessions may have less of an impact on physical or psychological health (Charalampopoulos et al, 2017). This, rather than Cook and Eat attendance itself, may explain why overall those young people who attended Cook and Eat were less affected by the overall increase in HbA1c observed in the ExCYPDS caseload after 2017/18. However, attendees and non-attendees all had a wide range of HbA1c, suggesting that HbA1c was not a barrier to engagement with the structured education.
The potential benefits of session engagement may be greater for some of the families who felt least able to engage. Further evaluation of attendance and non-attendance of Cook and Eat sessions is needed to understand barriers and facilitators to session engagement.
Conclusions
The Cook and Eat sessions are popular with both CYP and their families and friends, with many attending multiple times. Sessions provide a clear educational pathway for teaching CYP level 3 carbohydrate counting skills in preparation for adulthood. Although this review showed no difference in HbA1c between attendees and non-attendees, findings were suggestive of a protective effect against increasing HbA1c over time for those who attended multiple times and from a younger age.
While this evaluation focused on HbA1c, we strongly argue that a more diverse and holistic approach to considering the value of group education is warranted in order to engage attendees, reduce barriers to attendance, further understand CYP, their peers and families’ experiences of group participation, and impact on clinical outcomes. Future research should investigate the facilitators and barriers to attendance at Cook and Eat sessions and assess how young people would like to design and change the Cook and Eat model moving forward.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022