Education is the mainstay of diabetes care (Phelan et al, 2018; Smart et al, 2018). On March 23rd 2020, England entered its first national lockdown due to the SARS-CoV-2 pandemic (COVID-19), and diabetes education had to adapt. Online and digital platforms were adopted widely by the NHS to facilitate ongoing care, including the apps Digibete and MyType1Diabetes (Kar, 2020), and the Twitter group Diabetes 101 (Iacobucci, 2020); this facilitated rapid dissemination of critical education on COVID-19 and diabetes management.
“Cook and Eat” carbohydrate education for children and young people (CYP) at Exeter Children and Young Person’s Diabetes Service changed from a once-a-year offer of face-to-face delivery (Leveridge et al, 2018) to three Zoom-based sessions, which were offered to all. Virtual sessions commenced in October 2020 and this article provides reflections on developing the sessions, uptake and key lessons from this process.
Cook and Eat aims and learning outcomes
Each session involves CYP cooking a recipe at home with a parent or carer. Each recipe is designed to be easy to follow and uses accessible and inexpensive ingredients. The recipes have been created to incorporate healthy fats (monounsaturates), limit added “free” sugar and include sources of fibre (oats, vegetables or fruits) as part of a healthy diet. All recipes can be adapted for gluten-free or dairy-free diets. Parents are emailed the ingredient list and an equipment list one week prior to the session.
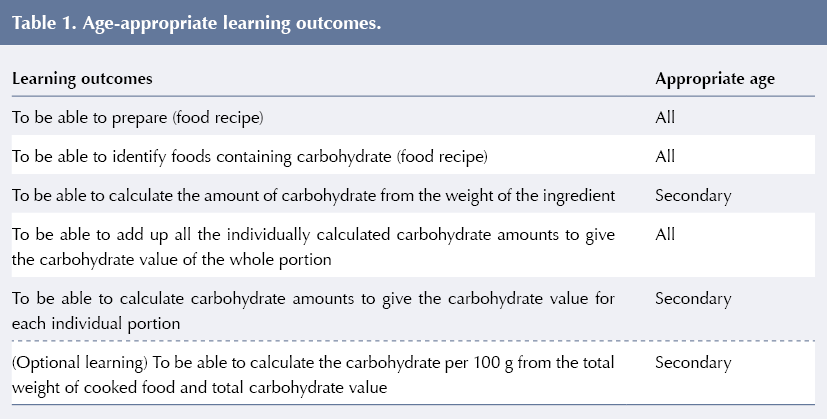
The primary aim of each Cook and Eat session is to create a fun, engaging and collaborative environment for supporting carbohydrate counting. Secondary aims include an opportunity to meet other young people with diabetes, include siblings and other family members in carbohydrate counting, and learn aspects of health and nutrition. Table 1 shows the key learning outcomes for the sessions.
Recruitment
CYP were recruited via the DigiBete app, and news, email invitation and posters were placed on parent/carer support group Facebook pages. Sessions were held during school holidays and, with the aim of increasing attendance, the days of the week and timings of sessions were varied. Each session lasted 45–60 minutes. While face-to-face sessions were for CYP up to Year 11, all CYP on the paediatric diabetes caseload were welcome to attend the virtual sessions, including those up to 18 years of age. CYP who expressed interest but were unable to attend were offered an individual session.
Digital requirements
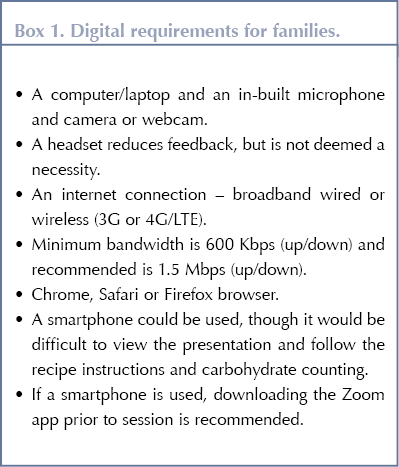
After the initial pilot in October 2020, Zoom Pro (San Jose, California, USA) was identified as the most suitable online platform. It is funded (£14.39 inc VAT per month) via The Norman Family Charitable Trust (https://nfct.org) and has been approved by local NHS Trust Information Governance for the purpose of group education. A total of eight CYP can join and remain on screen in one thumbnail section, and digital requirements are detailed in Box 1. More CYP can be accommodated if required. Health professionals delivering the sessions will require adequate WiFi and bandwidth, and a laptop or computer with webcam and microphone.
Session content
Sessions followed a consistent structure. Using the Zoom share screen function, a Microsoft PowerPoint presentation was shown to CYP. The presentation started with a welcome and introduction, a “show and tell” game in which all CYP were invited to participate (e.g. showing pets, Christmas decorations or board games) and session ground rules. The presentation was then used to work through the steps of the recipe and then the carbohydrate estimation process. Participants indicated when they were ready to progress to the next step.
Participants progress through the measuring and skills section of the recipe at differing rates; this allows “bitesize” nutrition and diabetes education opportunities. Examples of discussions included the benefits of fruit and vegetables; impact of fat and protein on glucose levels; glycaemic index; and benefits of reduced salt or increased fibre intakes. In one session, a student dietitian delivered a topic on healthy eating and the benefits of fruit and vegetables.
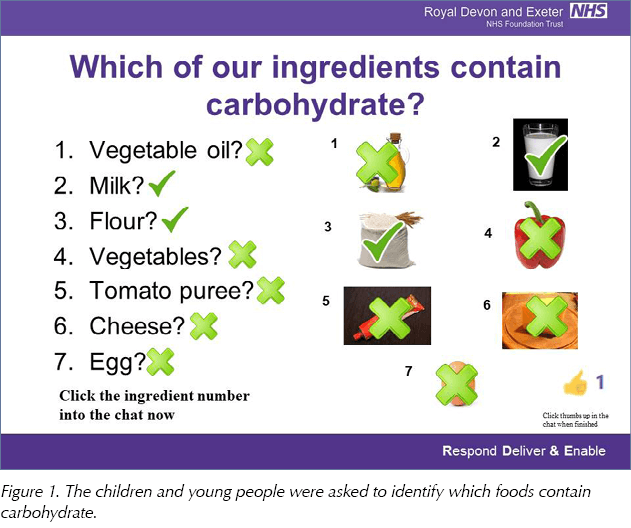
Once the recipe is completed, CYP are supported to engage in carbohydrate counting. Firstly, CYP are asked to identify which ingredients contain carbohydrates (Figure 1); secondly, they calculate the carbohydrates in each ingredient and then add the carbohydrates in all ingredients to estimate the amount in the whole mixture. Finally, the amount per portion is calculated. As participants’ ages and abilities varied, each needed differing levels of support to engage with this process. In some sessions, additional learning included calculating the amount per 100 g of a food item and managing extra carbohydrate with icing and sweet decorations.
A range of savoury and sweet recipes were used, including apple flapjack bites, ginger cookies and pizza muffins. Considerate of inclusivity, parents or carers could request a grocery voucher (funded by parent support groups) for purchasing ingredients and equipment from the facilitator.
The Cook and Eat virtual sessions have also been attended by a range of clinicians, such as a clinical psychologist and visiting dietitians from outside of Exeter.
Sessions have not been formally evaluated; however, participants were asked to feed back on the taste and acceptability and to share photographs of their food with the facilitator by email after each session. Some participants shared their feedback via Twitter to @RDE_Dietitians or the facilitator @MariaLeveridge using #CookAndEatExeter.
Attendance
In total, 11 virtual Cook and Eat sessions were offered at three time points between October 2020 and February 2021. Twenty-one (15.6%) of the 135 CYP aged under 16 years attended. Eight (38.1%) of the 21 CYP were of secondary school age. Additionally, 42 CYP aged 17 years and older were offered, but did not attend, virtual sessions.
Several CYP attended multiple sessions; 41 sessions were attended by 21 CYP, with 6 (28.6%) attending at all three time points and 8 (38.1%) attending at two time points. CYP of primary school age attended more often (2.1 sessions) than secondary school age (1.8 sessions). Six CYP cancelled on the day of the session or “were not brought” to the session, and 50% were of secondary school age. Thirteen (62%) of the CYP who attended had also attended at least one face-to-face Cook and Eat session. CYP who expressed interest but were unable to attend were offered an individual session. Four CYP have attended individual sessions with one attending a future group.
The average age of the 21 CYP who attended over the three sessions was 9.7 years (range, 5–15 years). The mean duration of diabetes was 4 years, 1 month (range, 0 months to 10 years and 6 months). Three CYP (14.3%) had been diagnosed within 6 months of their session. Slightly more males (7.6 on average per session) than females (average 6.0) attended the sessions (Table 2).
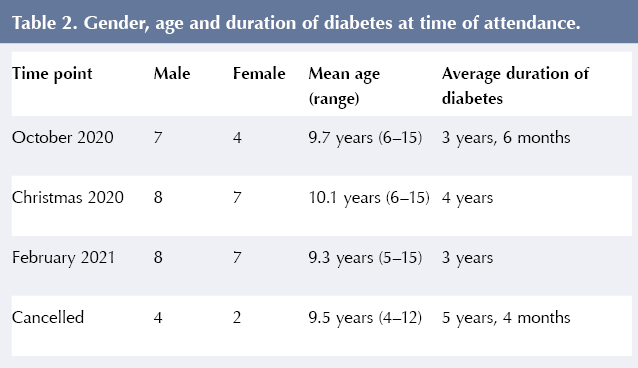
The most popular day for sessions was Monday, with Friday being the least popular; no sessions were offered on a Thursday. Three sessions were in the morning (average 4 children per session) compared to 8 afternoon sessions (average 3.6 children per session). Afternoon sessions appear more favourable, although this may reflect more sessions being offered in the afternoon.
Evaluation
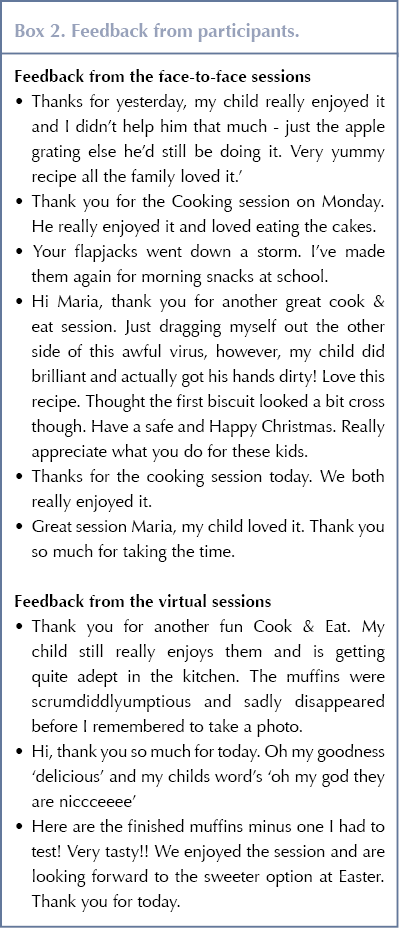
Parent feedback via email (Box 2) has been excellent and the families shared their creations online via Twitter and with the team.
Discussion
This article describes the development and delivery of virtual Cook and Eat sessions when face-to-face sessions were no longer possible due to the COVID-19 pandemic. Eleven virtual Cook and Eat sessions were offered at three time points between October 2020 and February 2021. While the sessions primarily aimed to provide opportunities for continued diabetes education, the sessions also allowed families opportunities to informally meet one another and to engage with a member of the paediatric diabetes team, both of which have been impacted by the pandemic. The feasibility, acceptability to families, benefits and limitations of virtual Cook and Eat sessions will be discussed and opportunities for future development and evaluation will be considered.
The primary aim of Cook and Eat sessions is to provide an opportunity for continued diabetes education. Structured diabetes education is one criterion in the Best Practice Tariff in England (Department of Health, 2011), and the Royal College of Paediatric and Child Health (RCPCH; 2017) states that education should be provided on an ongoing basis (including outside of clinic) throughout the CYP’s attendance at the paediatric diabetes service. Teaching “level three” carbohydrate counting (Smart et al, 2018), and maintaining skills in this area, is just one aspect of structured education. Face-to-face Cook and Eat sessions (Leveridge et al, 2018) were a popular and fun vehicle for real-life carbohydrate counting education, and virtual Cook and Eat sessions provided a similar opportunity.
Enhancing and adapting the educational opportunities during Cook and Eat sessions was considered. CYP learn best when learning is relevant to real life (Phelan et al, 2018) and a positive outcome – in this case, enjoyable food – is achieved. Cook and Eat encompasses a range of classic pedagogical learning activities (Fleming, 1995): listening (to the facilitator), tactile (handling food), visual and reading (presentation slides).
Both the content and facilitation of the sessions were considered and continually refined to enhance learning. For example, knowledge of mathematical concepts (addition, subtraction, multiplication and division) required for the carbohydrate counting aspect of sessions are dependent on age and ability. The sessions were initially divided into primary and secondary school age groups, with the aim of having homogeneity in anticipated mathematical abilities. It was observed, however, that the CYP, and in some cases parents and carers, appeared less confident to share their answers in case they were incorrect. Adults in England have low numeracy skills, with only 22% achieving Grade 4 and above GCSE maths (Department for Business Innovation and Skills 2012), so to avoid stress and embarrassment sessions were adapted so that participants could attempt a question in their own time and not share their responses; this meant that differences in mathematical ability were less problematic in sessions and all subsequent sessions were open to all age groups.
Taking an adaptable and considered approach to diabetes education within virtual Cook and Eat sessions may increase CYP’s engagement and learning from sessions.
The Cook and Eat programme not only provides a platform for educating CYP about carbohydrate counting and nutrition education, but it also offers a chance to engage with healthcare professionals in a positive way outside of clinic appointments, share experiences with peers and access community diabetes support. While CYP have the opportunity to develop a relationship with a member of the diabetes team, which is hypothesised to facilitate later engagement, the sessions also create a vehicle for team members to ascertain CYP’s understanding of diabetes and to take a targeted approach to furthering their knowledge of nutritional strategies, as defined by ISPAD Guidelines (Smart et al, 2018), which goes beyond the mathematics of carbohydrate counting. In summary, the sessions provide opportunities beyond that of providing continued education.
While virtual Cook and Eat sessions provided important educational and additional opportunities, the acceptability to families of the online session format must be considered. Examination of session attendance showed that fewer families attended online than typically attended face to face annually in previous years. In total, 21 CYP attended the virtual sessions compared to 46–51 people attending previous face-to-face sessions within the same service (Leveridge et al, 2018). Furthermore, virtual sessions were attended by both those who had previously been to face-to-face Cook and Eat sessions and those who had not. The sessions were attended by a wide age range (4–15 years), and also the diabetes duration ranged from newly diagnosed to 10 years and 6 months. This was consistent across all sessions. The majority of CYP attended at more than one time point.
The sessions have not yet been formally evaluated; however, informal feedback has been positive and suggests families found sessions enjoyable. Taking both attendance information and informal feedback into account, it is suggested that virtual Cook and Eat sessions are both acceptable to and enjoyed by families, although some may prefer the face-to-face sessions.
Furthermore, attendance indicated that the sessions are more popular with CYP of primary school age rather than secondary school age. It was noted that nobody above Year 11 (age 16 and over) opted to attend the sessions. However, as CYP in school years above Year 11 were not invited to attend previous face-to-face Cook and Eat sessions, it is not clear if their lack of attendance is an indication that the virtual format or the overall Cook and Eat process is not an acceptable form of diabetes education for this age range. Different methods of continued diabetes education should be considered for this age range.
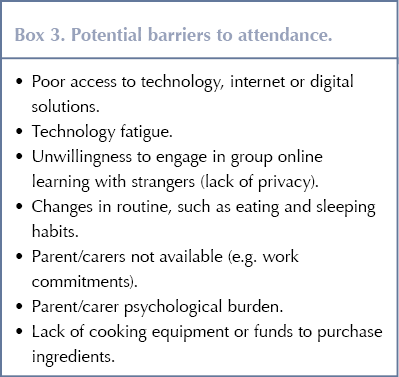
There are a number of possible reasons for reduced attendance (see Box 3). During the pandemic, parents had been significantly burdened by competing demands from work, home schooling and isolation from friends and family, which all contributed to increased psychological stress (Lee et al, 2021). It is feasible that families have wanted to switch off from online learning during school breaks and thus may not have wanted to attend the virtual sessions. Additionally, social disparities must be considered, including difficulties accessing digital resources (Ramsetty and Adams, 2020).
The recent National Paediatric Diabetes Audit 2019–20 (RCPCH, 2021) shows that the CYP caseload in Exeter is of a predominantly white ethnic background (93.9%, compared with the National profile of 78.3%). Three of the 21 participants (14.3%) were from a non-white background, indicating a similar profile to our caseload ethnic demographic. Those who cancelled or were not brought were all from a white ethnic background. The caseload is also populated with greater numbers in the least deprived postcodes (27.1% compared to a national picture of 18.5%), which may explain why the vouchers offered were not taken up.
Despite these potential barriers to attendance at the virtual sessions for some CYP, online sessions may enhance accessibility for others, for example, by not requiring families to travel to sessions or arrange for the care of other siblings.
Further understanding of families’ experiences is needed; while reasons for non-attendance have not currently been evaluated, a survey of both those who did and did not attend would aid understanding of attendance barriers and inform strategies to enhance accessibility.
The overall transition to online sessions and the specific platform selected should be considered when reflecting on the feasibility and acceptability of sessions. Previous research shows that families gave positive feedback regarding the use of virtual technologies, and it is likely that future diabetes care will continue to incorporate their use (Ng, 2020). The video platform used for sessions was important for ease of facilitation and family experiences. Zoom gave an advantage over other platforms as it is easier to operate. Additionally, up to 8 families can simultaneously be viewed by the facilitator, which increases the cost-effectiveness of session provision. Repeated attendance by CYP suggests that they find it a positive experience.
The virtual platform has an additional advantage in allowing facilitators to share resources and promote virtual learning. Not only were professionals from other services easily able to observe online sessions but session proformas have been shared with the South West Paediatric Diabetes Network and University College London Hospitals (UCLH) NHS Foundation Trust. To date, paediatric diabetes services at Bath, Gloucester, Taunton, Torbay, Swindon and UCLH have delivered sessions of a similar nature. This informal peer review has helped to further develop and refine the programme, although the authors acknowledge that future quality assurance should be addressed with review by independent assessors and measured against criteria that ensure consistency.
Aiming to enhance inclusivity and decrease the potential impact of financial burdens of session attendance, Swindon hand-delivered recipes and ingredients to families, and Gloucester provided grocery vouchers to purchase ingredients. DigiBete now hosts the Cook and Eat resources so that other healthcare professionals can deliver both virtual and face-to-face sessions. A family page on DigiBete will also host recipes for a family of four from all previous Cook and Eat sessions.
This project has shown that technology enhances the possibilities for mutual learning; however, thought must be maintained regarding identifying and combating challenges to session attendance.
Conclusions
The Cook and Eat programme remains a novel and enjoyable vehicle for continued diabetes education, specifically teaching CYP about carbohydrate counting alongside healthy eating messages and practical cooking skills. Group sessions may also have psychological benefits and promote the development of positive relationships with healthcare staff. Uptake is lower via virtually delivered education than face-to-face sessions, and further investigation is needed to address barriers to attending and participant experiences.
During the COVID-19 pandemic, virtual “Cook and Eat” sessions were found to a feasible and cost-effective dietetic education intervention, and theses sessions appear to be acceptable to families, while providing additional opportunities for developing innovation and resource sharing.





NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022