Conditions such as type 2 diabetes, which are more prevalent among the South Asian population, are associated with poorer dietetic outcomes such as weight loss and the achievement of glycaemic targets. South Asians are less likely to follow a healthy diet than the general population (Sohal et al, 2015). Traditional South Asian diets are high in carbohydrate (>45% total daily energy intake), the main sources being chapattis or rice, pulses and fruit. Add to this the convenience foods plus sugary drinks and foods readily available in the UK, and the total daily energy intake from carbohydrates can be close to 70% (O’Keefe et al, 2016).
Globally, some people with diabetes within the South Asian community are aware of the impact carbohydrate-based foods have on their blood glucose levels, while others acknowledge gaps in their carbohydrate knowledge (Patel and Iliffe, 2017; Zhuoshi et al, 2018). It would seem pragmatic to provide South Asians with targeted carbohydrate education to address any gaps in knowledge.
The extent to which South Asian non-English speakers engage in diet and lifestyle behaviour change is shaped by language barriers, a tendency to prefer medication to diet, and low health literacy (Greenhalgh et al, 2015). Introducing a more prescriptive consultation style may be key to improving outcome measures in non-English speaking South Asians in the UK.
Barriers to behaviour change and self-management
Patient and healthcare professional communication plays a key role in patient health, knowledge, decision-making and motivation. For people with long-term conditions necessitating life-long behaviour changes in addition to activities of normal living, successful self-management skills seem to be best cultivated by a narrative-based approach to dietetic management. This involves listening to the patient and understanding their health from their broad perspective, rather than as a medical problem. It enables the clinician to better understand the patient’s story and identify barriers that may be resulting in medical outcomes that are less than optimal. Narrative-based medicine, at its very least, gives patients permission to unburden themselves, and attentive listening is intrinsically therapeutic.
People with diabetes frequently complain that doctors do not listen, they appear disinterested, they interrupt, they make assumptions, and they do not address patient concerns (Zaharias, 2018). Undoubtedly a language barrier further challenges any therapeutic relationship; with a reported 58% of UK Pakistanis not proficient in the English language (Office for National Statistics, 2013), many practitioners will need to overcome language barriers (for example, by using Language Line or interpreters) to improve outcomes in practice.
Health literary and numeracy skills are fundamental to diabetes self-management, including interpreting food labels, quantifying portion sizes, following written instructions, understanding medication dosage and adjustment, and comprehending test results (Bibi, 2017). Diabetes self-management tasks encourage the development of problem-solving skills and motivate change. In South Asian communities, family and friends are likely to play a pivotal role in making dietary strategies relevant and accessible – and behaviour change possible – where language is a barrier (Emadian et al, 2017). Communities may also present barriers to any change. Alternative health messages, such as the use of traditional remedies, may be more readily heard and accepted by the patient than other diabetes management strategies. Furthermore, diabetes may be viewed as socially unacceptable. Social stigma is likely to negate self-management efforts (Kumar et al, 2016) and may heighten a patient’s feelings of anxiety and hopelessness about their condition. Conversely, some people of South Asian origin reason that their role in health is externally influenced, if not controlled, inducing a more passive approach to health (Lucas et al, 2013).
Audit of dietary education in practice
UK dietitians use food models and photos of chapattis to quantify carbohydrate amount and tailor dietary goals. A retrospective audit presented positive dietetic outcomes in people with insulin-treated diabetes (Boocock, 2013). Outcomes for English speakers of White and South Asian (predominately of Pakistani ethnic origin) backgrounds proved comparable. However, the outcomes for the sub-group who did not speak English were noticeably poorer. On average, English speakers lost 2.0 kg in the year after the intervention (1.85% of their original weight; P=0.007), while non-English speakers lost just 0.6 kg (0.65%; P=0.13).
Despite guidance from the dietitian to moderate chapatti intake, patients often disregarded advice in favour of replacing their usual chapatti and curry with grilled meat and steamed vegetables. Although this client group is generally able to monitor blood glucose without problems, for some, limiting carbohydrate further than intended without diabetes specialist nurse (DSN) advice resulted in hypoglycaemia; for others, their resultant eating plan was bland and unsustainable. Misconceptions about diet, such as the avoidance of traditional foods, may impede the adoption of healthy dietary advice (Sohal et al, 2015). Acculturation (i.e. assimilation to the dominant culture) is evident in the dietary practices of South Asians but arguably less visible in non-English speakers (Gupta et al, 2018).
Consultations in this audit took a patient-centred, behaviour change approach and used a comprehensive toolkit of dietary strategies. The language barrier, alongside a preference for medical management of diabetes and the deep cultural significance of food in maintaining social relationships and tradition, are likely to have made integrating dietary self-management in this South Asian community of non-English speakers difficult.
Literature review
A literature review was performed to explore knowledge and attitudes around a healthy diet for diabetes and identify barriers to behaviour change and self-management in South Asian non-English speakers in the UK. Three databases – Medline, AMED and CINAHL – were searched for relevant articles published from 2013 to 2018, inclusive, with 23 relevant publications being identified.
UK guidelines for people with diabetes emphasise an individualised approach to dietary management (Diabetes UK, 2018). The joint American Diabetes Association and European Association for the Study of Diabetes consensus recommends individualised medical nutrition therapy focusing on the nutritional quality of food choices, with or without energy restriction (Davies et al, 2018). No single dietary approach is recommended. Low carbohydrate diets (<26% total daily energy intake) are currently a popular dietary strategy for people with type 2 diabetes and healthcare professionals alike, not least due to their short-term clinical effectiveness (British Dietetic Association, 2018; McArdle et al, 2018). Moderate carbohydrate diets (26–45% of total daily energy intake) have not demonstrated clinical effectiveness (Sainsbury et al, 2018).
Greater reductions in HbA1c on carbohydrate-restricted diets are likely to be driven by increased weight loss. While weight loss of 2–6 kg offers health benefits, including improved glycaemic control for people with type 2 diabetes, it is unlikely to bring about diabetes remission (Brown and Leeds, 2019). Prescriptive dietary approaches, previously viewed critically by healthcare professionals, are offering clinically meaningful benefits (Lean et al, 2019).
A prescriptive approach to practice
It has been 5 years since the audit was carried out. The primary care weight management clinics for people with insulin-treated diabetes are run by a diabetes specialist dietitian in partnership with a DSN. As noted, previous attempts to improve glycaemic control in our non-English-speaking patients in the clinic setting, using the current weight management and diabetes dietetic toolkits, were ineffective. It was decided that a prescriptive approach to management should be taken with our current group of non-English-speaking patients. This would determine whether this was more effective than the patient-centred, behaviour change approach previously taken.
This prescriptive approach has, for some non-English-speaking patients, been the key to successful diabetes management. The case study presented here demonstrates the potential positive dietetic outcomes of using this dietary strategy.
Case history
Mrs A is a 65-year-old woman of Pakistani ethnic origin who speaks Punjabi. She attends appointments with her English-speaking daughter. A designated diabetes specialist language support worker acts as an interpreter during consultations.
Mrs A’s diabetes treatments include twice-daily biphasic isophane insulin Humulin M3, metformin and glimepiride. She describes her role as one of homemaker, where she is actively involved in the preparation of meals for her extended family. On initial presentation, her activity levels were limited by osteoarthritis. Emphasis was therefore placed on dietary change to manage her weight and blood glucose levels.
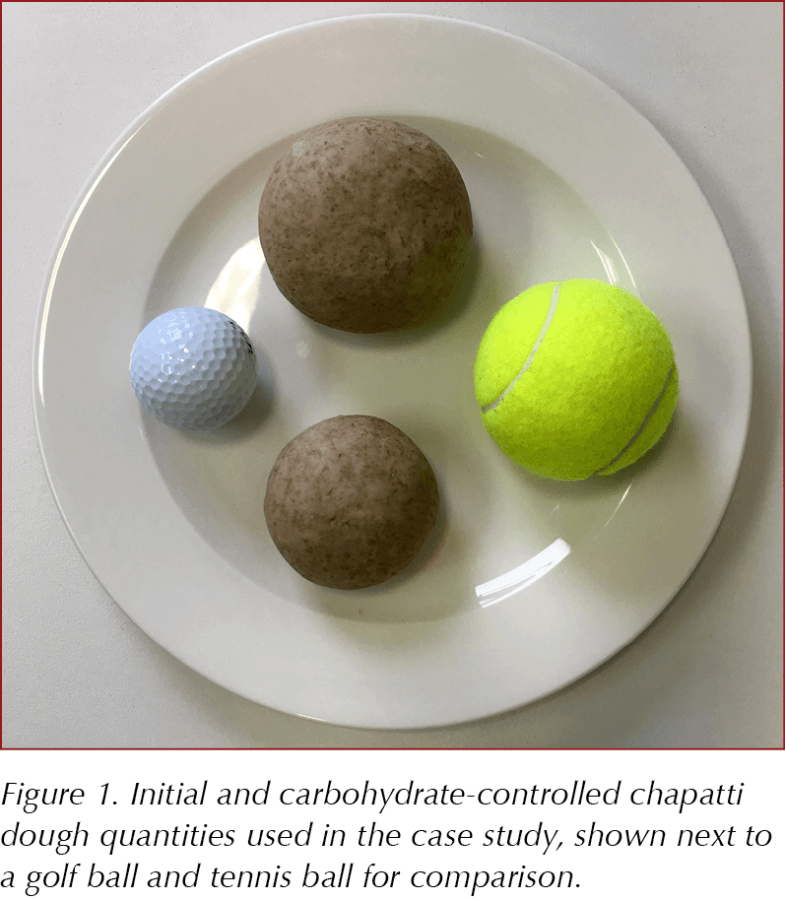
The dietary strategy employed, which was one dietetic management option from which she could choose or be offered by the dietitian, was moderate carbohydrate restriction (26–45% total daily energy intake). Initial (200 g) and portion-controlled (100 g) chapatti dough balls were shown in comparison with a tennis and golf ball, respectively (see Figure 1). As this food is the main source of carbohydrate in the South Asian diet, the reduction in carbohydrate consumption was achieved by weighing and limiting Mrs A’s chapatti dough ball size at her two main meals; her daughter purchased food scales to facilitate this behaviour change. The weighing of her chapatti dough balls – while unfamiliar and a source of amusement and conversation within Mrs A’s social network – was supported by her family. Celebratory events were successfully negotiated with the support of her daughter, combatting considerable social pressure to eat. Mrs A attended the dietitian on six occasions over 9 months during 2018.
Outcomes
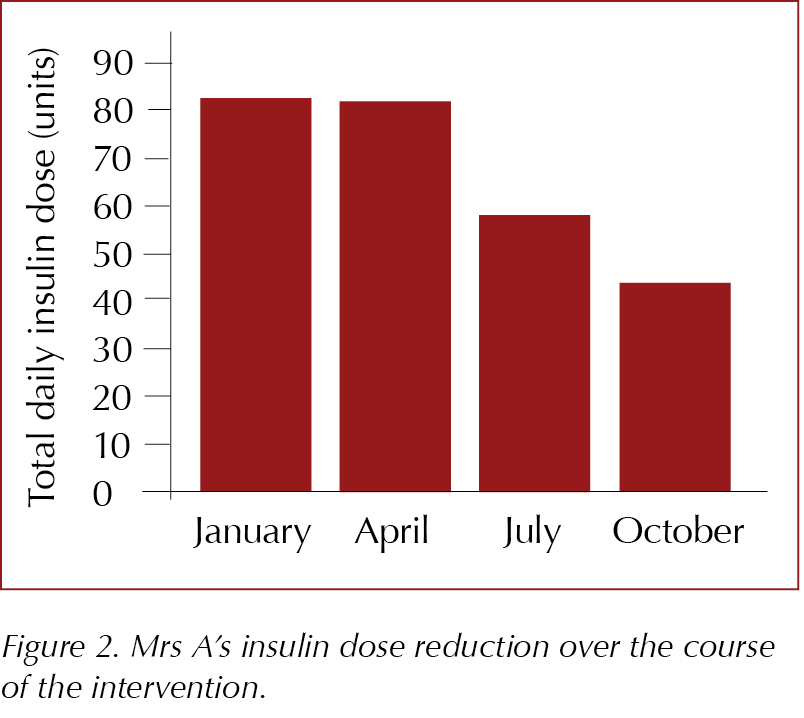
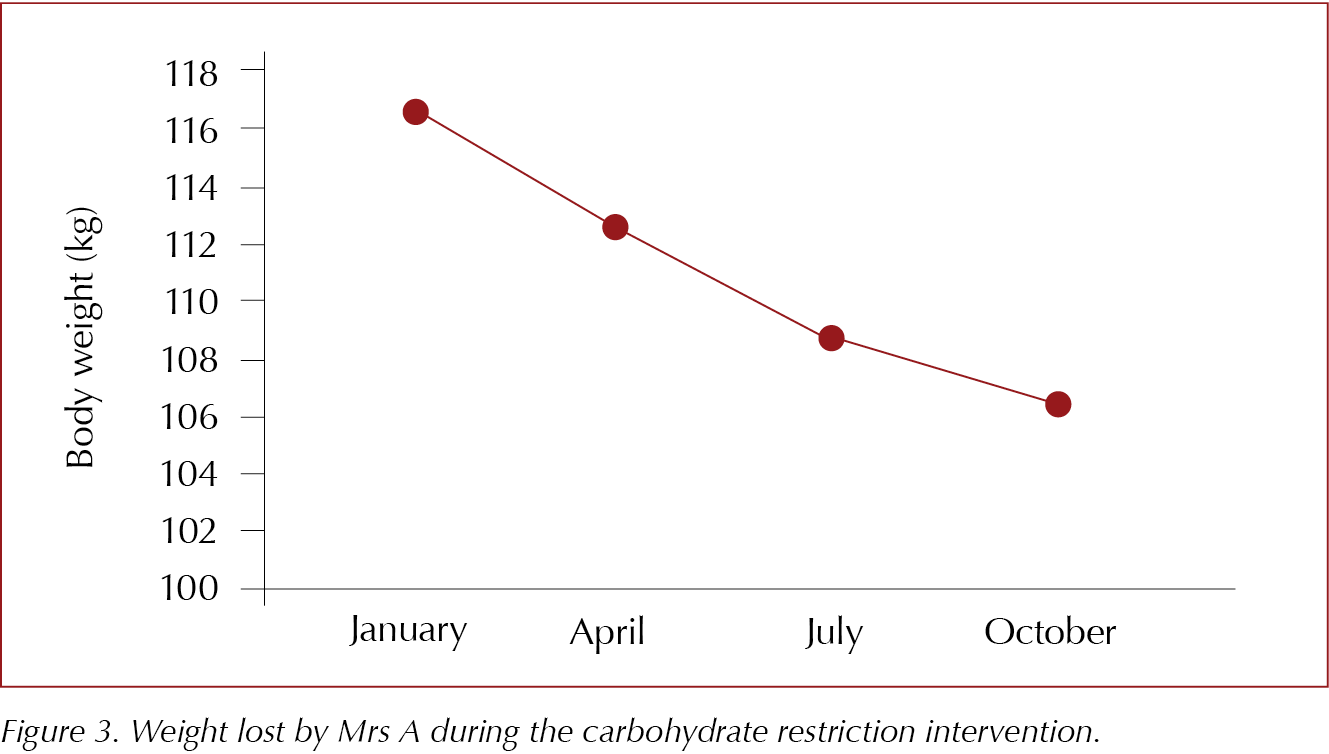
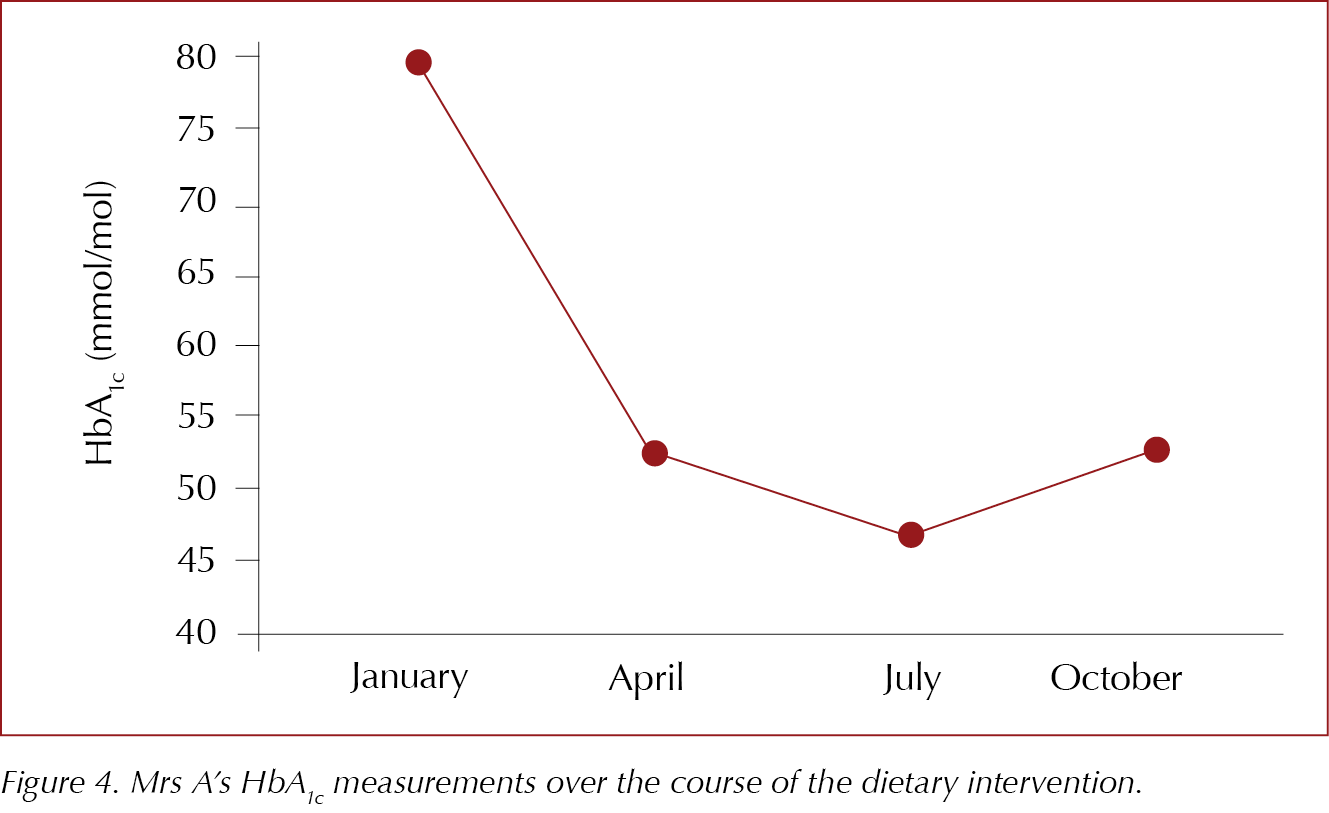
To optimise glycaemia and minimise the risk of hypoglycaemia following the introduction of a moderate carbohydrate diet, Mrs A’s insulin doses were adjusted by the DSN according to home blood glucose readings (see Figure 2). After 9 months, she had reduced her total daily insulin dose by almost half, from 82 units to 44 units. During this time, she lost 10.2 kg in weight (see Figure 3) and reduced her HbA1c level from 80 mmol/mol (9.5%) to 53 mmol/mol (7%; see Figure 4).
After 6 months, Mrs A’s HbA1c dropped to 47 mmol/mol, which was below her safe target. Following a face-to-face review, the preference of the patient and DSN (under whose care she remained throughout the dietetic intervention) was to reduce her insulin dose further. While stopping her glimepiride was an option, Mrs A was more comfortable taking tablets than injecting insulin. Patients or family members can access DSN advice through a helpline and no hypoglycaemic episodes had been flagged for Mrs A. Having consistent carbohydrate amounts at meal times can help to keep blood glucose levels more stable enabling lower HbA1c levels to be achieved without hypoglycaemic episodes.
The prescriptive food-based change made a big difference to Mrs A’s health and quality of life. As a result of the changes following the implementation of the prescriptive diet, she overcame barriers to increasing activity, including negative body image, joint pain and limitations in mobility. Reducing insulin dose, with its associated weight loss, is likely to contribute to the success of this dietary intervention.
Conclusion
A prescriptive approach to dietetic management involving accurately quantifying the carbohydrate portion of chapattis has proven a more achievable dietary self-management strategy for South Asian non-English speakers with insulin-treated diabetes than standard dietetic education. As described in the case history, this offers positive dietetic outcomes previously not attainable in the patient sub-group. Identifying a family member who had a genuine interest in the health and wellbeing of the person making dietary changes and who supported the change process helped the patient overcome perceived barriers. As South Asian communities within the UK are not a homogeneous group, further research into prescriptive dietetic management and behaviour change is needed.
Acknowledgement
With thanks to the Dietetic and Diabetes teams at Bradford Teaching Hospitals NHS Foundation Trust.





Jane Diggle examines the draft update to the NICE NG28 clinical guideline, plus new advice regarding the discontinuation of Levemir.
10 Sep 2025