Diabetes affects 6.6% of the UK population, with almost 3.7 million people living with diabetes in the UK (Diabetes UK, 2018). NICE (2014) has identified a list of eight key care processes (Box 1), which should be measured and achieved to identify areas where the quality of care can be improved for people with diabetes.
The annual National Diabetes Audit (NDA) aims to assess the achievement of these key care processes and the effectiveness of diabetes care across the UK, in both primary and secondary healthcare settings. However, people with diabetes are often seen in both primary and secondary care settings, and inadequate communication between healthcare providers can result in gaps in measurement and poor documentation of these care processes, thereby having a negative impact on patient care. This may include patients not receiving the appropriate screening and identification for kidney or foot disease, or having multiple tests carried out, resulting in the patient becoming frustrated with the healthcare system and disengaging with future screening.
The problem
Previous studies have shown a number of factors that may affect the measurement and recording of the eight key care processes (Gadsby and Young, 2016; Gadsby et al, 2016). It can be argued that the documentation of key care processes may be further reduced when people with diabetes are seen in both primary and secondary care settings. This may be due to a lack of communication between the two settings.
The lack of integrated IT systems between primary and secondary care often results in difficulties for GPs. Poor communication between primary and secondary care may result in GPs not realising that certain investigations have been carried out in secondary care. The GPs may then call patients in specifically for these tests, duplicating results and leading to unnecessary appointments, wasting time and resources for both patients and the practice. Conversely, GPs may assume that certain investigations have been completed in secondary care, whilst hospital physicians may assume they will be carried out in general practice. These investigations thus remain incomplete. Subsequently, all eight key care processes may not be measured, resulting in a failure to meet NDA targets and compromising patient care.
People with type 1 diabetes, as well as those with poorly controlled type 2 diabetes, are often seen in specialist diabetes clinics in hospitals. The lack of integrated IT systems between primary and secondary care is likely to have a greater impact on the care of these patients.
The solution: Diabmail
It is evident that good-quality, person-centred care can be further improved by ensuring effective communication between primary and secondary care. At Oxford University Hospitals NHS Foundation Trust (OUH), the Diabmail web application was designed and implemented in 2018 to achieve this aim.
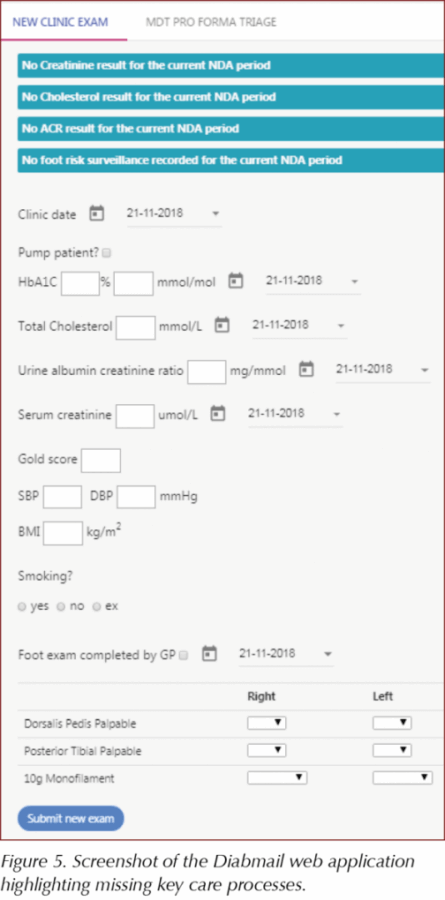
Diabmail was developed using the Play! web framework, chosen for its iterative and scalable nature. Play! has been the web framework for well-known websites such as LinkedIn and The Guardian. Diabmail allows the documentation of the eight key care processes when patients are seen in specialist diabetes pump clinics. Accessed via a secure web link, Diabmail is used during clinics to document the eight key care processes, and to clearly visualise the results. It highlights any incomplete care processes for that NDA year, acting as a reminder for healthcare professionals, who can then request additional investigations to ensure the standards of care are in keeping with NICE (2014) Quality and Outcomes Framework indicators.
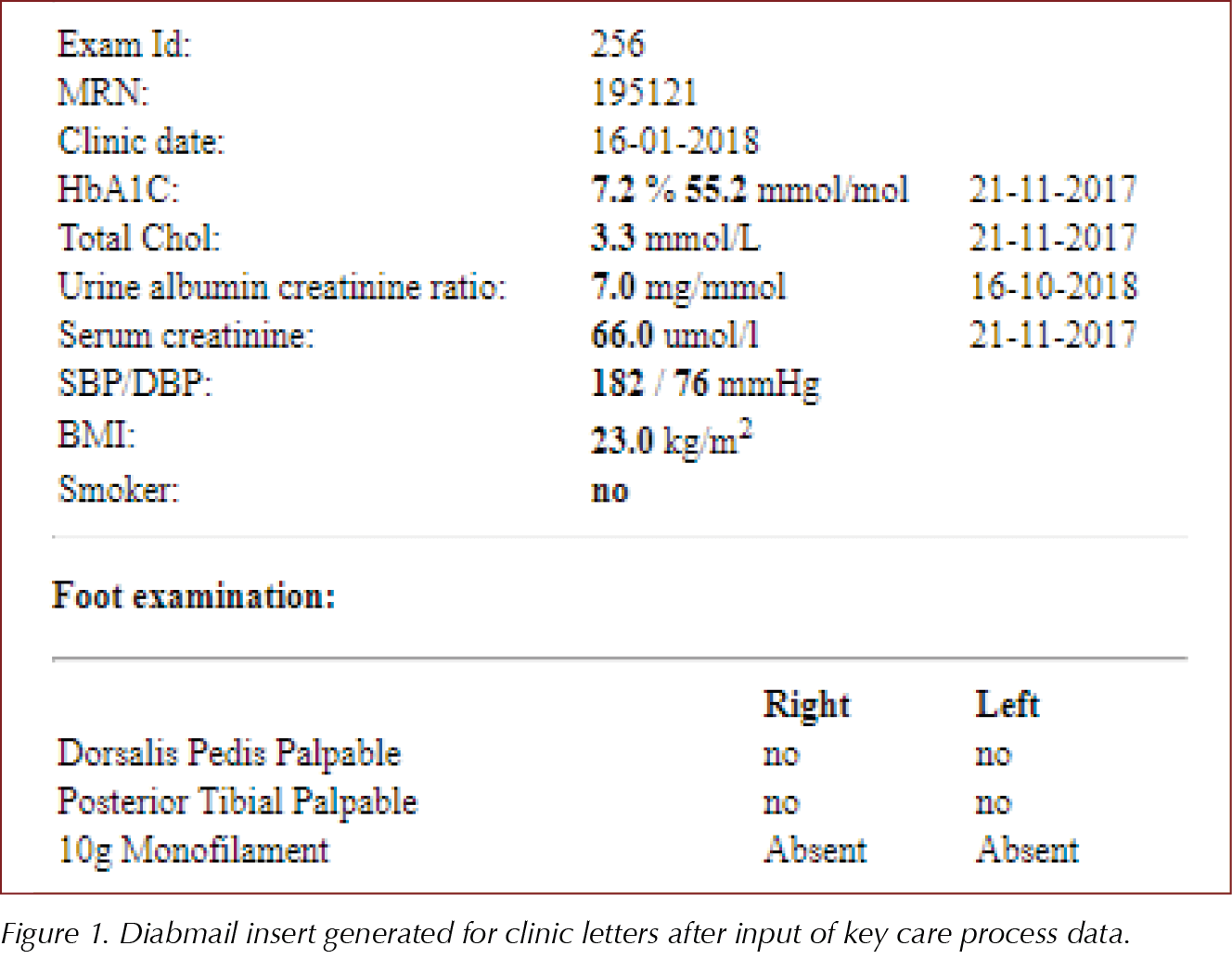
Once the parameters have been entered onto Diabmail, they can be added as an insert into clinic letters to GPs (Figure 1), thereby improving communication between primary and secondary care. The GPs now have an up-to-date list of the NDA investigations that have been carried out in specialist diabetes clinics and can identify any incomplete processes. Subsequently, they can ensure that investigations are not unnecessarily repeated and that missing key care processes can be completed in the primary care setting.
While the data currently need to be entered in the GP systems, we are working to produce a single patient record that will automatically transfer these data and remove the need to input any additional data.
Currently, Diabmail is being trialled for more than 350 people with diabetes who are being seen in specialist pump clinics within OUH. The department plans to expand the use of Diabmail to all patients seen within diabetes clinics at OUH.
Diabmail as an audit tool
By sharing relevant investigation results with GPs, Diabmail has an additional benefit. It acts as a useful audit tool, allowing quick analysis of the recorded data over the 15-month NDA period, identifying missing key care process values and pinpointing gaps in care which can then be addressed.
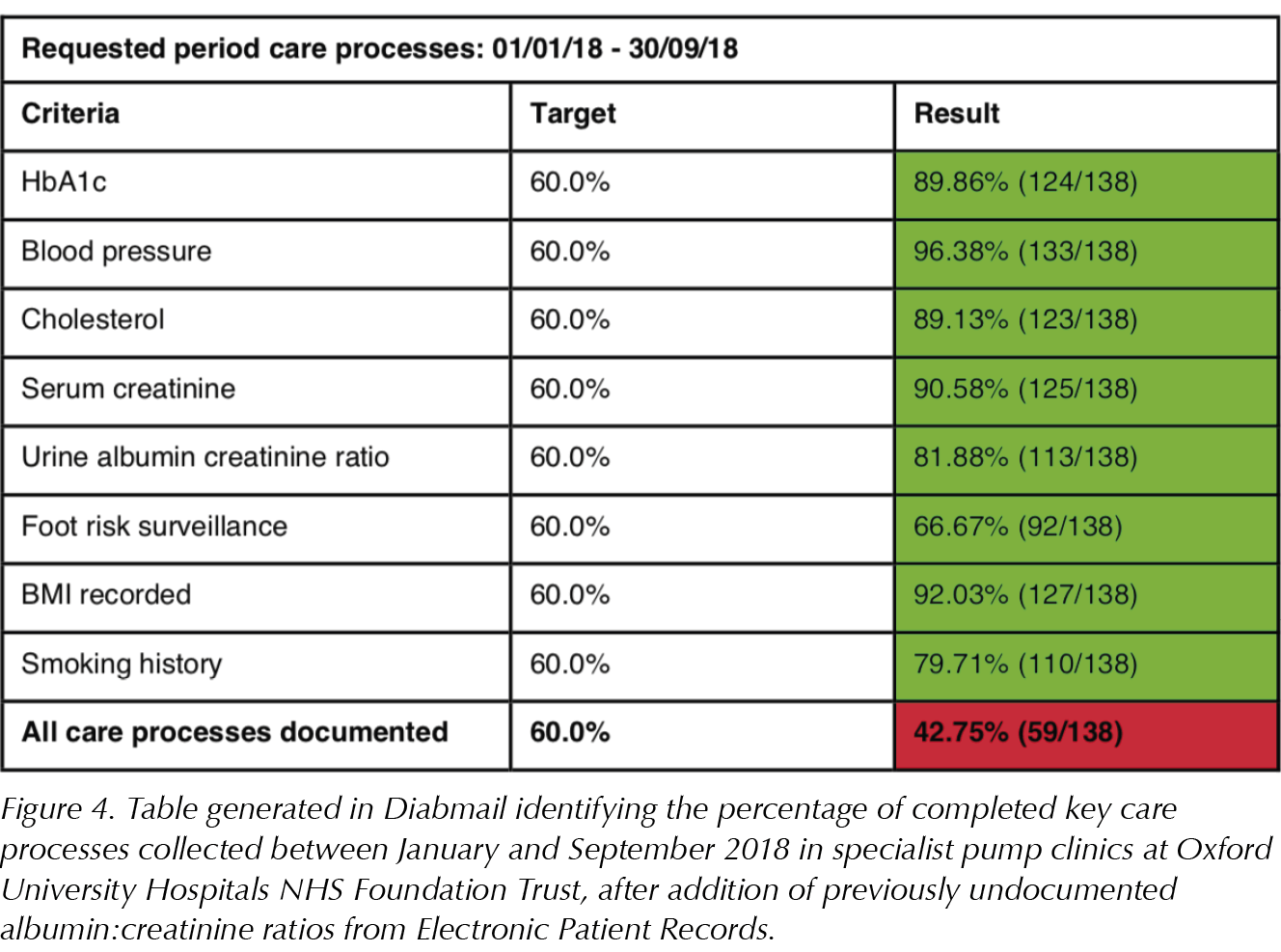
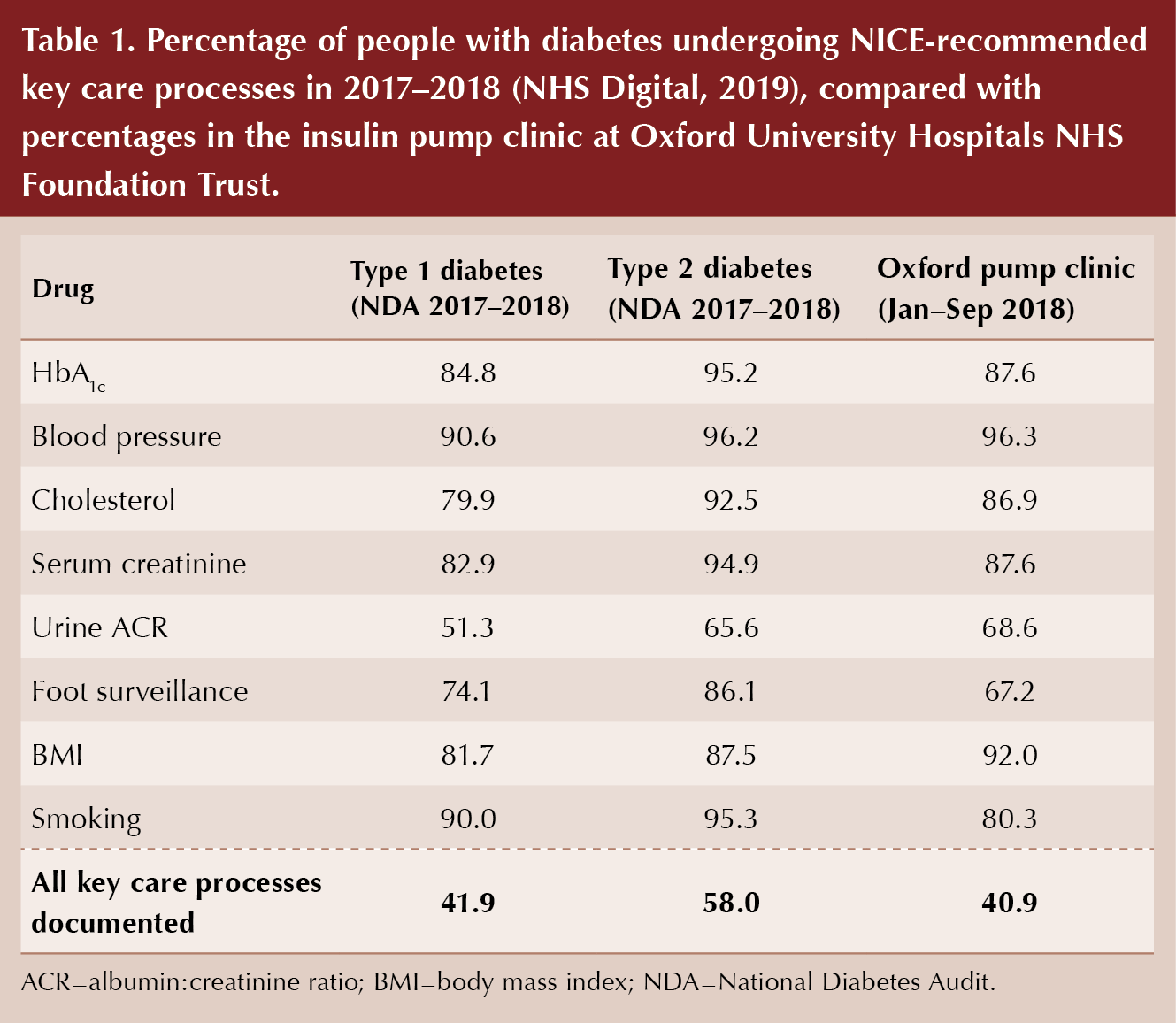
Diabmail was used in this way at OUH to provide a summary of the captured key care processes between January and September 2018, identifying areas for further improvement (Figure 2). Preliminary analysis using Diabmail for the insulin pump clinic suggested that, although national targets were being met for most individual key care processes, only 41% of patients had all eight key care processes documented.
Diabmail can be used to generate a list of people with incompletely documented key care processes. For example, it can generate a list of people with an incomplete smoking history, who can then be contacted to obtain the relevant information. This can then be shared with GPs for individual patients, enabling them to carry out the missing investigations as deemed necessary.
From the audit, it was clear that healthcare professionals were particularly good at recording blood pressure, BMI and blood test results for HbA1c, cholesterol and creatinine; however, smoking history, urinary albumin:creatinine ratio (ACR) and foot risk surveillance were recorded in fewer patients. These findings echo national figures: in the 2017–2018 NDA, ACR and foot surveillance were the lowest completed indicators nationally (NHS Digital, 2019; Table 1).
Implementing improvements using audit findings
In the pump clinic at OUH, urinary ACR was identified as a poorly recorded parameter. This may be the case for a number of reasons. Often, ACR may be ordered by healthcare professionals but patients may not provide a sample at the time of the appointment and may forget to bring one at a later date. The ACR results appear on the Electronic Patient Record (EPR) 1–2 days after the clinic appointment, and thus, while healthcare professionals may complete the Diabmail entry at the time of the appointment, they may forget to add the ACR entry when they check the results at a later date. At present, there is no automatic population of the Diabmail template from the EPR, but this work is currently in progress. This means that even though ACR testing has been carried out, the incomplete record in Diabmail decreases the percentage of documented ACR in the specialist clinic audit.
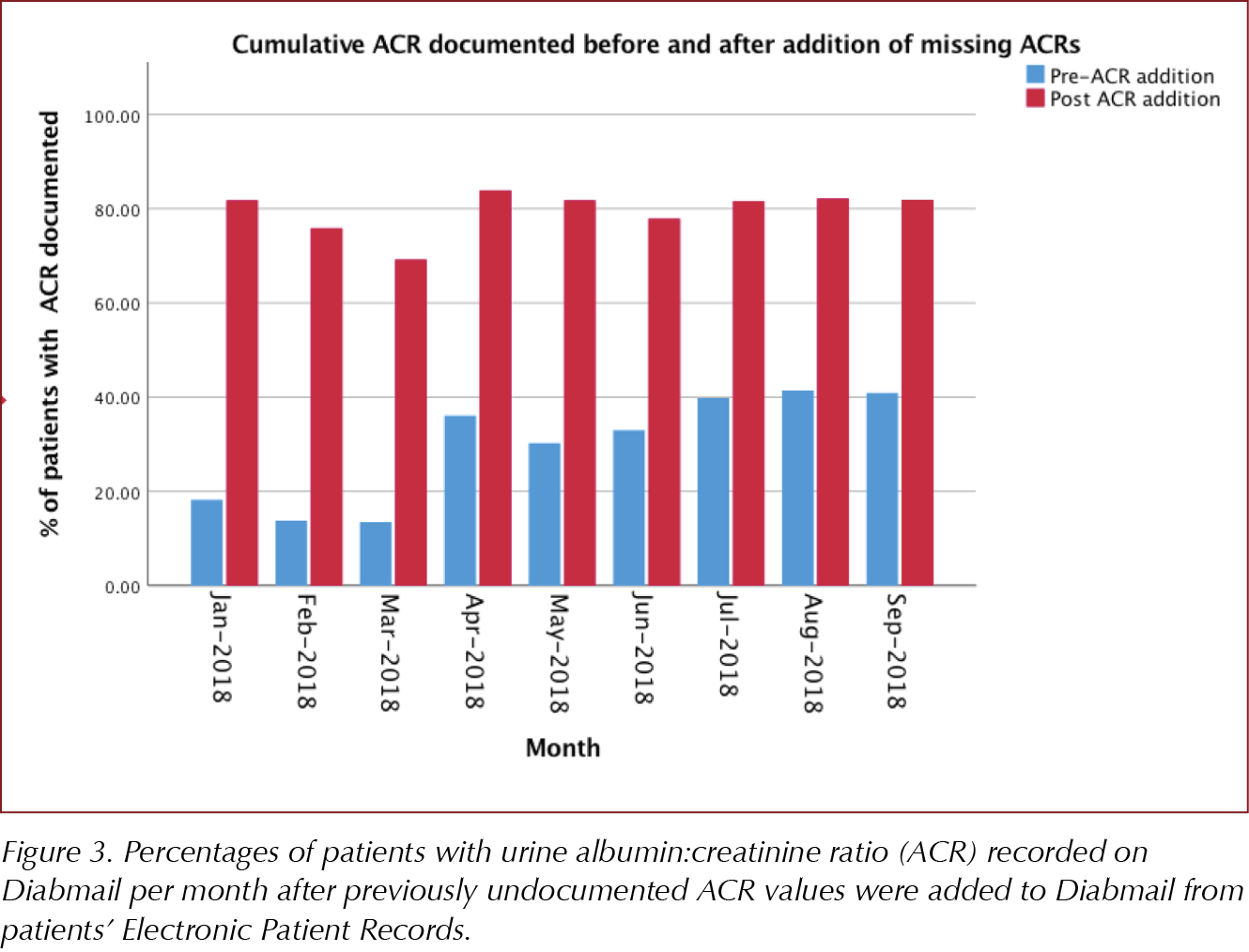
Following identification that incomplete documentation of ACR onto Diabmail contributed to lower NDA percentages, the Diabmail database was queried for individuals with missing ACR data. This generated a list of 55 individuals. EPRs were reviewed for each of these people to determine whether an ACR had been carried out within the 15-month NDA period. All ACR values present on the EPR were subsequently documented in Diabmail, thereby more accurately identifying all recorded key care processes within the clinic.
This resulted in a significant improvement in the documentation of ACR on Diabmail (Figures 3 and 4). However, although a notable increase was seen in the percentage of ACRs documented, from 68.6% to 81.9%, the percentage of people with all eight care processes showed only a marginal improvement, from 40.9% to 42.8%. This indicates that the percentage of all care processes documented may be impacted significantly by other parameters such as foot risk surveillance and smoking history, suggesting there is room for further improvement to meet the NICE-recommended indicators.
Further improvements
Since the design and implementation of Diabmail, new features have been added to help meet NICE-recommended indicators and further improve the documentation of the key care processes. For example, during an appointment, when physicians access a patient’s Diabmail record, incomplete processes are highlighted. This data can also be shared with GPs through the insert generated in Diabmail, which is added to the clinic letter (Figure 1). Figure 5 shows an example where an individual has not had their creatinine, cholesterol, ACR or foot risk surveillance checks carried out in the 2018–2019 period. This is easily seen by the clinician accessing the record, who can then order the relevant investigations.
As smoking history and foot surveillance were identified as poorly documented parameters in OUH, attempts have been made to improve the documentation of these parameters in particular. To improve smoking history documentation, healthcare assistants have received training to ask patients about their smoking history as part of their initial assessment. This should help make a significant difference to the documentation of smoking history on Diabmail over the next 6 months.
To further improve documentation of foot surveillance, Diabmail now allows foot examinations that have been carried out by GPs to be documented. This means that foot surveillance can be accurately recorded, avoiding repetitive foot checks and saving time and resources.
The future of Diabmail
Diabmail is already regarded as a useful system by many GPs in the Oxford area, with one GP stating: “It is really notable and really helpful that [the doctors at the pump clinic] are brilliant at documenting in letters all the data that we all need re. the eight key care processes, so thank you for doing so”.
As Diabmail is a secure web application, it can be accessed easily from all clinics by healthcare professionals who have permitted access. It is easy to use, with minimal training required, and prompts will be placed in clinic rooms as a further reminder to complete entries on Diabmail during appointments. The prompts provide details of the key care processes as well as information about accessing Diabmail. This should help increase the use of Diabmail by all clinicians in specialist pump clinics at OUH, aiding the accurate recording of the key care processes.
Work is currently in progress to automatically pre-populate the Diabmail template from the EPR. This should ensure that all investigations carried out in a secondary care setting during that NDA period will be relayed to GPs and will be included in the audit, significantly improving the documentation of the key care processes in accordance with the Quality and Outcomes Framework.
Due to the successful use of Diabmail in pump clinics, this application can be rolled out for use in all diabetes clinics in the Trust, improving documentation of the key care processes as well as communication between primary and secondary care in this patient group. As the NDA evolves to include statin treatment, Diabmail can be modified to include additional fields, enabling it to remain relevant and useful in the future.
Conclusion
The Diabmail platform has successfully addressed many of the problems encountered when completing the NDA: it improves the documentation of the eight key care processes, enhances communication between primary and secondary care, and functions as an effective audit tool. It is already regarded as a useful system by many GPs in the Oxford area.






Jane Diggle examines the draft update to the NICE NG28 clinical guideline, plus new advice regarding the discontinuation of Levemir.
10 Sep 2025