Some adults with type 1 diabetes also choose to follow low-carbohydrate diets. There has been a small number of trials and observational studies in this population. A recent systematic review of nine studies found inconsistent results and concluded that, due to heterogeneity between studies, an overall effect could not be determined (Turton et al, 2018). The authors suggested that more primary studies investigating both the short- and long-term effects of low-carbohydrate diets were necessary to support their use in practice.
Low-carbohydrate diets are not currently recommended for children and young people with diabetes due to insufficient evidence either for or against this way of eating. However, there are concerns about other potential risks to health that such diets may pose beyond HbA1c. This article aims to discuss the limited available evidence, highlight potential risks and offer information regarding the management and monitoring of the children and young people who choose to follow this way of managing type 1 diabetes.
What counts as low-carbohydrate?
The generally accepted levels of carbohydrate per day for the differing definitions of low-carbohydrate are listed in Table 1 (Dyson, 2015). These are based on the percentage contribution that carbohydrate makes to daily energy intake. However, they are based on mass-population adult daily energy requirements of 2000 kcal/day.
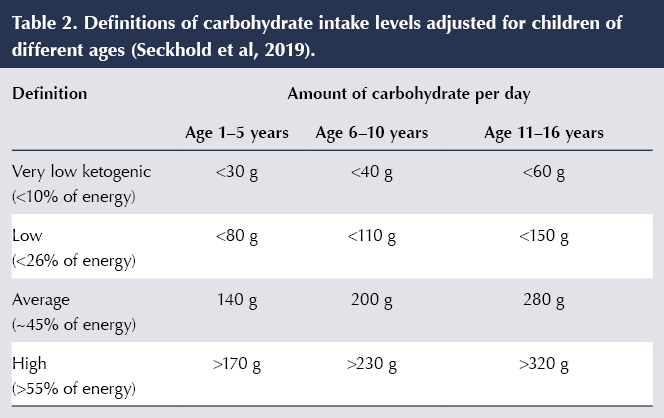
Individual energy requirements for children are constantly changing based on age, gender, size and activity levels. An example of how the definitions above can be applied to children was suggested in a review by Seckold et al (2019), and are shown in Table 2. However, again, these are based on estimations of average energy requirements rather than individually calculated.
Very-low-carbohydrate diets
A very-low-carbohydrate diet means that meals and snacks contain no obvious starchy carbohydrate foods – no bread, potatoes, rice, pasta, cereals, grains, pulses or flour. Fruit and much dairy are restricted due to their fructose and lactose content. Many of these foods provide valuable energy, vitamins, minerals, fibre and antioxidants, which are associated with good health. The diet is largely gluten-free by default. Small amounts of carbohydrate come from vegetables, nuts, berries (low-carbohydrate fruits), salads, seeds and, sometimes, small amounts of high-protein yogurt (e.g. Greek yoghurt). Protein intake is usually extremely high, to create extra glucose by gluconeogenesis. Intake of fat is high to provide valuable energy, and the fat may come from animal and vegetable sources. There are many high-fat and high-protein snacks to make up the energy deficit, available either commercially or home-made using nut flours, fats, sweeteners and coconut products.
What does the evidence say?
There are very few publications involving children and low-carbohydrate diets, presumably due to lower numbers of people following this dietary approach. De Bock et al (2018) published a series of six case studies in which children aged between 3 and 13 years followed very-low-carbohydrate diets for between 6 months and 8 years. The case series described detrimental effects on growth, increased cardiovascular risk factors, deficient intake of some nutrients and eating distress for some of the children. These are the potential adverse events that concern some healthcare professionals.
Lennerz et al (2018) published the results of a survey in which nearly half of the subjects were children, self-selected from TypeOneGrit, an international online community for people with type 1 diabetes who follow a very-low-carbohydrate diet. Following adherence to the diet for at least 3 months, children or their parents reported low rates of adverse events and excellent glycaemic control, as measured by HbA1c.
Both of these studies have inherent limitations due to their designs. It is also notable that both articles reported significant patient distrust of mainstream diabetes services, where their treatment choices had been challenged and discussed.
There are no long-term safety data for this type of management in children with type 1 diabetes. The International Society for Pediatric and Adolescent Diabetes (ISPAD; Smart et al, 2018) advises that “There is international agreement that carbohydrate should not be excessively restricted in children and adolescents with diabetes”, and recognises the potential for difficult conversations by adding: “An emphasis should be on maintaining positive relationships between the family and the treating team”.
Both Diabetes UK (2017) and Diabetes Australia (2018) identify children as a vulnerable group for whom a low-carbohydrate diet is not advised at the current time. These organisations support these diets as one possible treatment option for adults with type 2 diabetes. For adults with type 1 diabetes, they acknowledge a limited number of studies showing potential benefits to glycaemic control but emphasise that these cannot form the basis of recommendations at present, due to limitations in robustness of their methodology and small numbers of participants. Both organisations call for larger and longer-term studies (minimum of 12–24 months) in order to justify potential recommendations on low-carbohydrate diets for people with type 1 diabetes.
What are the potential risks?
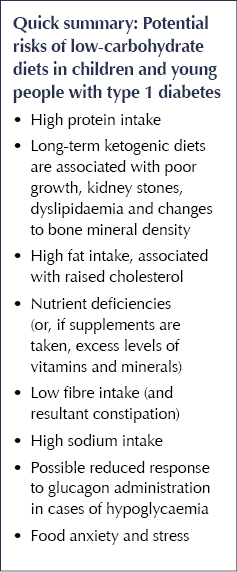
The goal of management of diabetes is all about lowering risk of both acute and chronic effects of the condition. Many children following very-low-carbohydrate diets achieve a low HbA1c, between 30 and 40 mmol/mol, and often report reduced variability in blood glucose levels, which would suggest a reduced risk of diabetes-related complications. However, it is possible that they may be exposing themselves to other risks, irrespective of diabetes status.
By necessity, very-low-carbohydrate diets for diabetes involve very high intakes of protein to create extra glucose through gluconeogenesis from amino acids. These levels can be as high as 2–4 g/kg/day, every day. Power athletes require less than this. Little is known about the safety of such high protein intake over long periods of time. Some long-term ketogenic diets used for the treatment of drug-resistant epilepsy, which are high-fat, moderate-protein and low-carbohydrate, have been associated with a number of adverse effects. These include poor growth, kidney stones, dyslipidaemia and changes to bone mineral density (Groesbeck et al, 2006; Groleau et al, 2014).
There is an increased risk of nutrient deficiencies if very-low-carbohydrate diets are not sufficiently planned, balanced and resourced. Sufficient calcium may be lacking during a significant growth period, and insufficient vitamin D (common in all society) may mean poor absorption of what is eaten, which may have detrimental effects on bone health. Multivitamins and minerals may be taken to rectify deficiencies but should be checked to ensure that excess levels are not consumed.
Due to the low intakes of fruit and avoidance of whole grains, cereals and pulses, it may be challenging to achieve recommended fibre intakes; therefore, very-low-carbohydrate diets have the potential to be low-fibre. Together with a high protein intake, this can lead to constipation and possibly a less favourable gut microbiome. Sodium may be eaten in excess from unlimited bacon, ham, sausages, cheese and nuts, ultimately affecting blood pressure and cardiovascular risk.
Insulin interacts with growth hormone and other growth factors. If it is restricted, will this affect growth irrespective of a fuel/energy deficit? Insulin doses of <0.5 units/kg/day are common in established adherents to very-low-carbohydrate diets. A prepubertal child with established diabetes would typically require 1 unit/kg/day. Both Lennerz et al (2018) and de Bock et al (2018) found some decrease in growth in those following these diets. There is an increased risk of raised cholesterol due to the high fat intake. Saturated fat intake is often high. The limited, poor-quality evidence available in children with type 1 diabetes who follow very-low-carbohydrate diets suggests that LDL and total cholesterol can increase, although HDL and triglyceride levels may be more favourable (de Bock et al, 2018; Lennerz et al, 2018). Foods that can actively reduce cholesterol (e.g. whole grains, oats, pulses, whole fruits) are avoided for their carbohydrate content. The potential for these dietary issues highlights the importance of involving dietitians, as part of the multidisciplinary diabetes team, with young people following low-carbohydrate diets. Indeed, ISPAD recommends that “if a child or family chooses to routinely consume a diet <40% energy from carbohydrate it is recommended that they discuss this with a dietitian to ensure the diet is nutritionally complete, particularly in regard to calcium, B vitamins, iron and fiber” (Smart et al, 2018). Advice regarding good heart health is essential, with preference for fats to come from monounsaturated and omega-3-rich sources rather than saturated fats, and encouragement of at least 60 minutes of physical activity each day.
An additional concern over very-low-carbohydrate diets is that the response to glucagon administration in order to raise blood glucose levels in mild hypoglycaemia has been found to be impaired compared with high-carbohydrate diets (Ranjan et al, 2017).
There is potential risk of increased anxiety over the demonising of a food group, and the fear of what carbohydrates will do to blood glucose levels. Whole-family change, making healthy choices for all, is difficult with this way of eating. Should the whole family adopt a very-low-carbohydrate diet to support the child with diabetes? What about other siblings; what is their motivation for such restrictions? Who will monitor the health of the other family members regarding the risks described above? Will social opportunities for young people be restricted if they do not participate in social occasions involving food? At a time where young people are desperate to “fit in” and conform, will this make them feel more different? Meal planning and insulin calculations can be quite complex, to account for the additional fat and protein, and this may delay independence in diabetes management.
A young person with diabetes may choose to reject this way of eating as part of their emerging independence. It is acknowledged that type 1 diabetes is difficult to manage during puberty due to the presence of growth and sex hormones, irrespective of any teenage behaviour that may exacerbate suboptimal management. A very-low-carbohydrate diet will not suppress these hormones and, coupled with a raging appetite and social pressure to eat “normally”, exclusion of a major food group may be a difficult task. Those who follow a low-carbohydrate diet may argue that improvements in glycaemic control and HbA1c are worth the additional work and difficulties the approach requires; however, this diet will undoubtedly pose additional challenges to the growing young person with diabetes.
Care of children/families who opt for the low-carbohydrate approach
In the absence of high-quality, long-term evidence about safety, recommending this dietary approach would be inadvisable professionally. However, an environment should be fostered where open and honest conversations can be had with the families choosing to follow this way of eating. We should act on the information in front of us, openly sharing any findings causing concern. Consistency in staffing will help nurture this relationship. It is also our responsibility to support the children practically, and to monitor for the risks highlighted previously.
Insulin management
Low-carbohydrate meals are hard to match with rapid-acting insulin analogues, due to their composition. Regular/short-acting insulin may be preferable because of its longer time–action profile, in order to match the delayed rise in glucose from protein and fat. While its use is outside usual paediatric practice, it is still insulin, and using it means that more units can be tolerated at a meal, which may be beneficial. In the UK, short-acting insulin is available as Humulin S (in a pen device), Actrapid (vial only) or Insuman Rapid (available in both formats but very rarely used in paediatric practice). Insulin syringes have a standard 8 mm needle, whereas 4 mm is now the preferred length for paediatric patients using a pen device. Rapid-acting analogues may still be used for correction doses.
Tresiba twice daily or Levemir three times daily are commonly used, although such dose frequencies are against the manufacturer’s instructions. Rapid-acting insulin analogues can be used in pumps with enhanced basal rates or extended bolus doses, with additional insulin used to manage the delayed glucose rises associated with the higher fat and protein content of the meals. Continuous glucose monitors are commonly used for monitoring of glucose values and often are self-funded.
Frequent mild hypoglycaemia is commonplace and tolerated, with hypoglycaemia only treated at levels below 3.6 mmol/L, and with less fast-acting carbohydrate than guidelines, and standard practice, suggest. This may pose difficulties for schools and the paediatric diabetes team where care plans are concerned.
Monitoring
In clinic visits, growth should be monitored on a centile chart and blood pressure taken, as is standard practice. It is useful to assess protein intake to estimate the level per kg. Check any supplements and doses to prevent excessive intakes. Carry out full cholesterol screening (including total cholesterol, LDL, HDL and total cholesterol:HDL ratio) on children of all ages, not just those over 12 years, as would be usual practice. If a random sample is high, this should be repeated with a fasting level.
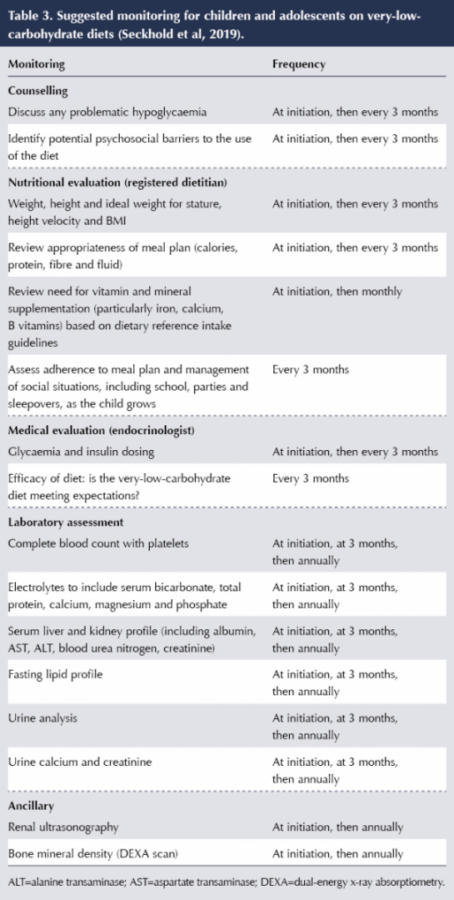
Seckold et al (2019) propose an approach to monitoring children with type 1 diabetes who are following a very-low-carbohydrate (<10% energy from carbohydrate) diet (Table 3). These proposals are adapted from guidelines for monitoring children following ketogenic diets for epilepsy, and are significantly more in-depth than would usually be done at annual review, including renal and bone scans. It is worth noting that, due to the intensive monitoring required for people on ketogenic diets, staff ratios allow for close supervision of much smaller numbers of patients than is typical in diabetes care for children and young people.
Lessons to learn
Part of the criticism of standard diabetes management by families who choose to eat this way is that they were told at diagnosis, “eat what you like, just give insulin for it”. This is not a useful message to hear at diagnosis, either for parents or a child; it is just not true for successful diabetes management. Most specialist teams would no longer say this, but junior medical staff, ward staff and well-meaning relatives may reinforce this myth. All carbohydrates are not of the same quality, and inevitably changes will need to be made to meal patterns and/or food choices for optimal diabetes management. It is important that nutritional education at diagnosis considers the diet as a whole and focuses on nutritious sources of carbohydrate (vegetables, beans and pulses, fruits, wholegrains and dairy foods), aiming to minimise the intake of highly refined and/or high-sugar sources of carbohydrate that are less nutritious. Education on glycaemic index and the effect of different foods and meals on blood glucose levels is also important.
Strategies that may help with management of blood glucose levels and prevention of large postprandial fluctuation may include giving patients and their families a carbohydrate “prescription” – the appropriate amount that the child should be eating for age, weight, height and activity levels. It is essential that these are individually calculated to reflect the child’s specific requirements based on gender, weight and activity levels, as population estimates often overestimate energy requirements. This will help prevent excessive portion sizes and consequent glucose load. More glucose and more insulin may result in more variability if in excess of requirements. In paediatrics, all families should be carbohydrate counting from diagnosis and, therefore, should be able to follow rough guidance at meal times. Downloads from meters and pumps can be used to identify habitual excess intakes.
Dietary and insulin adjustment education at diagnosis should include strategies to prevent large postprandial fluctuations in blood glucose levels. This will enable target levels and HbA1c to be achieved whilst maintaining a healthy diet containing nutritious sources of carbohydrate. Blood glucose meter downloads, and especially flash/continuous glucose monitor downloads, can be utilised to manipulate timings of meal-time insulin administration and allow meal content to be altered to reduce the glycaemic index in order to help minimise postprandial variation. Advanced bolus techniques, including dual-wave, extended and multiwave boluses, can be utilised on insulin pumps, and a “super bolus” can further fine-tune insulin delivery to cope with differing types of meals.
Concluding remarks
The use of very-low-carbohydrate diets in children is controversial; however, the number of families following this way of eating is likely to increase. There is a lot anecdotal information in online forums, communities and social media, from which families trying to follow very-low-carbohydrate diets seek advice and management strategies. Encouraging and starting a child on such a diet would be inadvisable professionally based on the lack of evidence and the combined international professional opinion at the current time; however, it is vital to create an environment where families feel listened to, where monitoring can take place and constructive conversations are encouraged for the benefit of the child.





Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025