Safe use of insulin
Su Down, Nurse Consultant in Diabetes, Somerset
- Injection technique and care of injection sites are as important as the insulin prescribed.
- Always inspect and palpate injection sites to identify lipohypertrophy. Insulin absorption from these sites is unpredictable, so ensure other sites are used for injections.
- Ensure people understand never to omit insulin when they are sick, even if they are not eating normally – often more insulin is needed rather than less. Ensure everyone on insulin has a copy of a sick-day rules leaflet to refer to when ill.
- There are more than 30 different insulins available in the UK – many have similar sounding names but very different actions. Ensure you are familiar with the action of those you prescribe.
- Ensure you are familiar with the DVLA guidance and that people using insulin know to notify the DVLA.
- Patients with deteriorating renal function are at increased risk of hypoglycaemia as renal clearance of insulin decreases. This is particularly important when eGFR is <45 mL/min/1.73 m2.
- Insulin combined with a GLP-1 receptor agonist is available (e.g. as iDegLira [liraglutide and insulin degludec]). Titration is by “dose steps”, which are a combination of each product.
- U100, U200 and U300 insulins are now available, increasing the risk of overdose if confused. Insulin must never be withdrawn from a pen cartridge or pen for administration using an insulin syringe – pens automatically calculate the dose of insulins of different concentrations and this is not possible using standard U100 insulin syringes.
- Biosimilar insulins, such as Abasaglar, are now available. These are not bioequivalent to other forms of insulin glargine. All insulins should be prescribed by brand name to prevent substitution at the point of dispensing.
- Consider when de-escalation of insulin therapy is appropriate, particularly in the frail elderly and those with hypoglycaemia.
Guidelines and resources
- The Six Steps to Insulin Safety – everyone who prescribes insulin should complete this module, even if they do not initiate or titrate insulin: https://diabetesonthenet.com/course
- TREND-UK Sick-day rules leaflet:
https://bit.ly/2IvDE4I - DVLA fitness to drive guidance:
https://bit.ly/2GroY4H
Diabetes and heart failure
Mike Kirby, Visiting Professor, University of Hertfordshire
- Type 2 diabetes is associated with a high risk for cardiovascular (CV), microvascular and other complications.
- Although glycaemic control is associated with a reduction in microvascular complications, effects on macrovascular benefits have previously been unclear.
- Concerns have been raised about the CV risks of some antidiabetes therapies. Regulatory authorities have, therefore, mandated CV risk assessment of all new diabetes treatments, including insulins.
- Cardiomyopathy in diabetes is characterised by ventricular hypertrophy, myocardial fibrosis and fat droplet deposition. Physical characteristics include early changes in diastolic function (up to 75% of asymptomatic patients with diabetes) and collagen deposition, and the presence of advanced glycosylation end-products [AGEs], followed by the late compromise of left ventricular systolic function.
- Individuals with diabetes are at high risk of developing heart failure (HF) and increased risk of dying from it.
- Anti-HF therapies, such as ACE inhibitors, beta-blockers and mineralocorticoid-receptor antagonists (MRAs), work similarly well in those with and without diabetes.
- Key points from NICE (NG106):
– Urgent (2-week) referral is needed if NT-proBNP is >2000 ng/L.
– The specialist HF multidisciplinary team should work closely with primary care.
– A stable patient should be reviewed at least every 6 months by their primary care team.
– Triple therapy with ACE inhibitor, beta-blocker and MRA is recommended for HF with reduced ejection fraction (HFrEF), with further options (such as sacubitril valsartan and ivabradine) available to the specialist team.
– An exercise-based cardiac rehabilitation programme should be offered to all with HF.
- In the management of HF with preserved ejection fraction (HFpEF):
– Address all coronary artery disease risk factors.
– Restore sinus rhythm (SR) in atrial fibrillation (AF), if possible.
– Control ventricular rate in permanent AF.
– Use diuretics for pulmonary congestion or peripheral oedema.
– Coronary revascularisation may be necessary in symptomatic patients or where myocardial ischaemia is affecting diastolic function.
– There is no evidence base for ACE inhibitors, ARBs or beta-blockers to treat HFpEF, but use if other indication (e.g. CKD).
- Take-home messages:
– Restore SR in AF if possible, control ventricular rate in permanent AF, up-titrate medications wherever possible, with dynamic diuretic dosing.
– Review regularly and use specialist HF nurses, if available.
– Refer if deterioration occurs and consider resynchronisation therapy.
– The multifactorial approach is very important in people with type 2 diabetes.
– Intensive management of hyperglycaemia reduces the risk of microvascular complications and, to a lesser extent, the risk of CV disease (CVD). However, targets should be relaxed in the elderly, frail, those with long-duration diabetes and those with existing CVD.
– In people with diabetes with existing CVD, the use of an SGLT2 inhibitor substantially lessens CVD and total mortality and HF hospitalisation without major adverse effects. SGLT2 inhibitors should be considered early in the course of diabetes management in such people.
- NICE chronic heart failure in adults guideline (NG106):
http://bit.ly/2CCdc8l - NICE chronic HF overview:
http://bit.ly/2HzyZ4T
Inspiring the patient
Mark Davies, Consultant Clinical Psychologist, Belfast City Hospital
- Healthcare professionals widely employ psychological theories, such as CBT, and approaches, such as motivational interviewing, to build and enhance patient motivation to change and maintain health behaviours. In contrast, the theories and approaches used in performance psychology are rarely employed.
- Performance psychology is a branch of applied psychology that focuses upon the factors that allow individuals, teams, and groups to achieve their aims. These ideas are used most frequently in the fields of sport, the military and the performing arts.
- Sports people, soldiers and performance artists are required repeatedly to perform complex actions to a high standard under huge pressure. Likewise, people with diabetes – especially those who are diagnosed with type 1 diabetes – are required daily to perform a range of self-care behaviours that have a huge impact on both their quality and their quantity of life.
- People in each of these groups have been reported to experience mental ill health more frequently than the general population.
- All are judged by outcomes – such as HbA1c with people with diabetes – and are held by others and themselves to be responsible for those outcomes.
- These outcomes, however, are multi-factorial. A wide range of variables determines whether a sports person wins, whether a production is successful or whether a soldier can do his or her duty. Capillary blood glucose is influenced by many factors (e.g. stress, illness, pain, medication, menstrual cycle, variabilities in insulin and background temperature), many of which are beyond the control of the person with diabetes.
- Holding others, or ourselves, responsible for outcomes they, or we, do not have full control over is counter-productive, and frequently leads to burn-out and depression.
- Performance psychology helps individuals to recognise what they have (and do not have) control over, and to take control (control the controllables) and optimise (marginal gains) the processes that influence the desired outcome. The outcome remains imperative, but the focus of the person with diabetes is re-directed from the outcome (HbA1c) to processes, such as attitude, insulin decisions, carbohydrate counting and CBG monitoring, over which they have full control.
- If the processes are optimised, this increases the chance, though does not guarantee, that the desired outcome will be achieved (the score will take care of itself).
- Diabetes healthcare professionals and diabetes services tend be very outcome focussed. Consider the reasons for this and whether healthcare professionals and people with diabetes alike would benefit from being discouraged from feeling responsible for things they do not have full control over, whilst being gently encouraged to perform the tasks they are in control of to the best of their ability and circumstances.
- Davies M (2018) Controlling the Controllables: http://bit.ly/2FnWZnR
- Nash J (2013) Diabetes and Wellbeing: Managing the Psychological and Emotional Challenges of Diabetes Types 1 and 2. Wiley-Blackwell, Oxford
David Millar-Jones, GPSI, Cwmbran
A person with diabetes is likely to live with complications of the condition and, possibly, other comorbidities. Be aware of the safe-driving criteria and advice published by the DVLA.
- Notification. All drivers who are on insulin must, by law, notify the DVLA. Drivers of Group 2 vehicles (including large lorries and buses) should notify the DVLA when any therapy prescribed to lower blood glucose has been started.
- Glucose monitoring. With regard to diabetes, the DVLA is concerned about the risk of hypoglycaemia.
– Blood glucose testing is currently required, but Flash or continuous glucose monitoring (CGM may be accepted in the future*.
[*In February 2019, the DVLA approved these methods of testing for insulin-dependent drivers of Group 1 vehicles.]
- Hypoglycaemia
– Group 1 drivers have more lenient criteria, unless the episode occurs whilst driving. They are allowed one severe episode before having to report, and episodes that occur whilst asleep are no longer counted. If there have been two episodes, the 12-month restriction is from the date of the first, but there is now a clause stating that the licence can not be issued within a 3-month period from the last episode.
- Retinopathy. Laser treatment for retinopathy needs to be reported. Visual fields are as important as acuity.
- Neuropathy. The diagnosis of neuropathy may cause concerns requiring special adaptations of the vehicle. It may also raise suspicion of autonomic dysfunction that is linked with arrhythmia, ischaemic heart disease and postural BP changes.
- Documenting fitness to drive.
– All advice given should be documented. Give written information to the patient.
– It is currently the patient’s legal responsibility to report to the DVLA and not the clinician’s.
– If there is concern about a person continuing to drive contrary to medical advice, it may be considered the clinician’s ethical duty to report. However, first ensure and record that the patient has been informed and attempts made at engagement are documented. Take advice from a defence union before divulging patient information.
– Remind the patient to inform their car insurance company as well as the DVLA.
- Vehicles you can drive: http://bit.ly/2TpcoJN
- Assessing fitness to drive: for medical professionals: www.gov.uk/dvla/fitnesstodrive
- TREND-UK Diabetes: safe driving and the DVLA leaflet: http://bit.ly/2FubeJ9
- Tiredness can kill: advice for drivers (INF159): http://bit.ly/2Ftcn3N
- DVLA D4 Medical examination and report for a group 2, bus or lorry licence: http://bit.ly/2U3PH2
Hypos and glucose monitoring
Nicola Milne, Community Diabetes Specialist Nurse, Manchester, and Jane Diggle, Specialist Practitioner Practice Nurse, West Yorkshire
Hypoglycaemia: ten key messages.
- Hypoglycaemia is a lower-than-normal level of blood glucose. It is defined as mild if self-treated, or severe if requiring third-party assistance or if blood glucose is <3 mmol/L (International Hypoglycaemia Study Group, 2015).
- Thresholds for hypoglycaemia vary with age. Delayed reaction times often occur in older adults, so this cohort may have asymptomatic hypoglycaemia and increased cognitive impairment.
- Symptoms may be autonomic (sweating trembling, hunger), neuroglycopenic (drowsiness, odd behaviour, confusion) or non-specific (headaches, malaise).
- There are multiple risk factors for hypoglycaemia, both medical and lifestyle. It is important to be proactive in reducing such risk factors when caring for and educating those with diabetes.
- Do not to be misled by HbA1c when assessing for hypoglycaemia, as HbA1c does not give an indication of possible glucose variability.
- The initial treatment option for hypoglycaemia in those that are conscious and able to swallow is 15–25 g of quick-acting carbohydrate: 60 mL Gluco Juice; 200 mL (small carton) of smooth orange juice; 5 or 6 dextrose tablets; 5 large jelly babies; 7 large jelly beans; 2 tubes of 40% glucose gel inserted slowly into the buccal cavity if the person is unable or unwilling to take other oral treatments*. (*This treatment cannot be given if the person is unable to swallow.)
– Call 999 for any unconscious person and put in recovery position.
- The Soft Drinks Industry Levy came into effect in April 2018. Many soft drinks manufacturers have changed product formulations to reduce the sugar content. Check the label of any sugary drink before using for hypoglycaemia treatment, as a greater volume may now need to be given to ensure effectiveness.
- Do not underestimate the impact of hypoglycaemia (especially recurrent hypoglycaemia), which can lead to: cardiovascular damage; accidents and injury; physical morbidity; reduced quality of life; psychological effects; and economic impacts, such as the need to take days off work (Frier et al, 2016).
- DVLA guidance relating to diabetes is updated regularly. Be aware of how to access the newest information (DVLA, 2019).
- Remember that hypoglycaemia is often unreported, owing to unawareness or worries about lifestyle implications. It is important to discuss this point at each review with those at risk, and to include their families and carers.
Glucose monitoring: ten key messages.
- Blood glucose monitoring is recommended for: all those with type 1 diabetes; for those with type 2 diabetes who take medications that might cause hypoglycaemia; and in special circumstances, such as pregnancy, using steroids, periods of illness, when fasting or when changing treatment (TREND-UK, 2017).
- Studies have shown that blood glucose monitoring has greater effect when associated with appropriate education. This can empower the person with diabetes or their carers to understand what readings mean and how to make necessary changes to lifestyle or medications based on them (TREND-UK, 2017).
- Often people with diabetes complain that healthcare professionals (HCPs) are not interested in their monitoring results. HCPs also need effective education on glucose monitoring and to be mindful of working with people with diabetes to achieve best outcomes.
- Flash glucose monitoring (currently via the FreeStyle Libre system) is indicated for measuring interstitial fluid (ISF) glucose levels in people from the age of 4 years with diabetes, including pregnant women.
– DVLA guidance also requires finger-prick blood glucose testing, although this is likely to change, so watch for DVLA updates* (DVLA, 2019).
[*Guidance updated February 2019.]
– A water-resistant sensor penetrates the skin on the upper arm to a depth of around 5 mm. A glucose reading is obtained by scanning the sensor with a reader. This negates the need for frequent finger-prick testing and the system does not need to be calibrated.
– The sensor continuously records data for up to 14 days and then needs replacement. It records a reading every minute and stores a reading every 15 minutes. An app can link the sensor to a user’s smartphone or the smartphones of carers or family members. A trend arrow shows the direction and rate of glucose change, and data can be downloaded for analysis. Training on such analysis can be obtained via the online FreeStyle Libre Academy.
– There has been variation across the UK in access to Flash technology, but NHS England has recently advised that access should be available to all those with type 1 diabetes from April 2019; it is also noted in the NHS 10-year plan. An awareness of any local access policies relating to Flash technology is important.
- CGM is available for those with type 1 diabetes that meet local criteria for access, but these people should be under specialist care. CGM systems require finger-prick calibration, but have alarms to alert a user when glucose levels are too low or high. CGM can be used from the age of 2 years.
Guidelines and resources
- Free glucose monitoring e-learning module: http://bit.ly/glucose-monitoring-cpd
- Assessing fitness to drive: for medical professionals: http://bit.ly/2OxQ67E
- TREND-UK guidelines on blood glucose monitoring: http://bit.ly/2Yzakm9
- FreeStyle Libre Academy: https://bit.ly/2v7T2z9
Diet – what advice would you give now?
Karen Jones, Senior Teaching Fellow, Warwick Medical School, and Diabetes Specialist Dietitian
- Encourage people with type 2 diabetes to “take control”. Losing weight and changing diet can have a big effect on the progression of type 2 diabetes – help patients to understand their role in this.
- In the prevention of type 2 diabetes, target weight loss of at least 5%, combined with an increase in exercise. There is no evidence of the best diet for weight loss – whatever suits the patient is best. Foods with evidence of protection against type 2 diabetes include wholegrain carbohydrates (moderate portion size for weight loss), fruit and vegetables, yogurt and cheese, and coffee and tea. Reduce processed and red meat, refined carbohydrates and sugar-sweetened drinks.
- There is compelling evidence that remission of type 2 diabetes can be induced by weight reduction in those diagnosed <6 years (DiRECT trial; Lean et al, 2018). 73% of people treated with an 800-calorie/day diet who lost over 10 kg were in remission at 1 year.
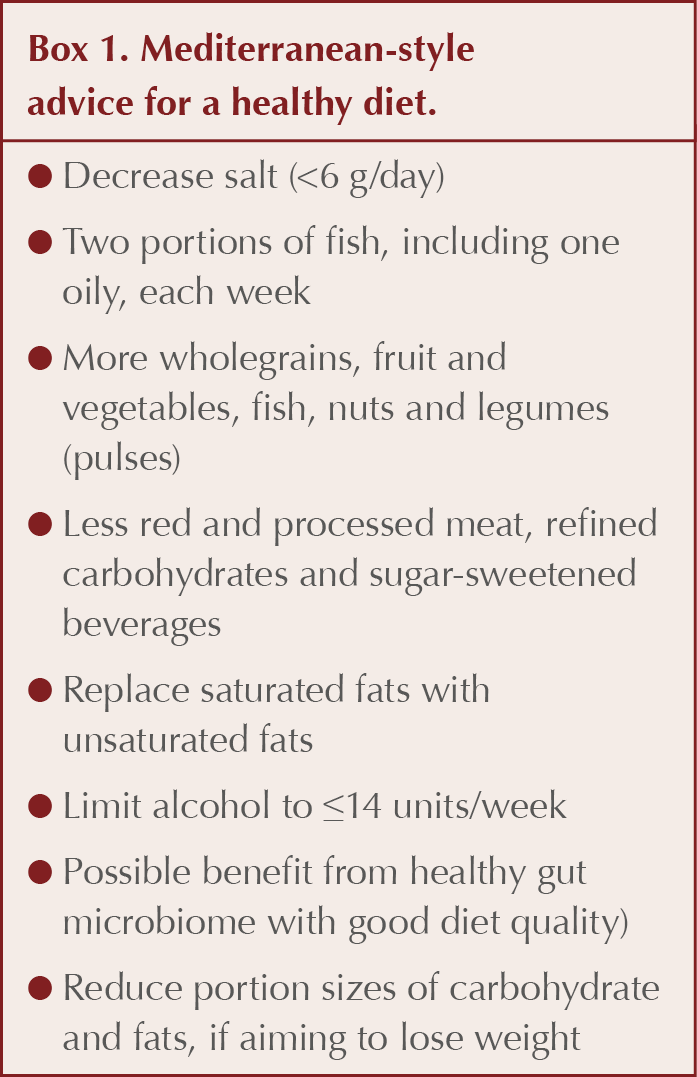
- To improve glycaemic control, weight reduction of at least 5% is still a primary aim, the sooner after diagnosis the better. There is no convincing evidence of the best diet to induce weight loss, although there is some evidence for the benefit of a Mediterranean-style diet (see Box 1) in weight reduction, improving glycaemia and CVD risk reduction (Farouhi et al, 2018).
- The best level of carbohydrate intake for type 2 diabetes remains unclear, but we should consider restriction as an option. A very-low-carbohydrate diet (30–50 g/day) improves glycaemia, but long-term evidence is lacking and adherence can be difficult. A low-to-moderate carbohydrate diet of 50–130 g/day may be more realistic for most, and is more easily adapted from a “normal” diet. Any reduction in carbohydrate intake should be accompanied by a medication review to avoid possible hypoglycaemia.
- Education on controlling carbohydrate intake when intensifying treatment can help to prevent weight gain as a consequence of commencement on insulin.
- Offer dietary advice along with diabetes education at identification of pre-diabetes, diagnosis and annual review, and before intensification of treatment. Refer to a diabetes specialist dietitian for further advice.
- Even if diabetes is well controlled, consider whether the patient can do more to prevent progression.
- Diabetes UK guidelines for the prevention and management of diabetes: http://bit.ly/2Yi1Q2r
- BDA Food Facts Sheets: http://bit.ly/2JxZA44
- Diabetes UK tips for healthy eating with diabetes: http://bit.ly/2JwJhnS
- Diabetes UK meal plans and diabetes: http://bit.ly/2WnOQa7
Complex cases: De-escalating therapies
Stephen Lawrence, GPSI, Kent, and Principal Clinical Teaching Fellow, Warwick University Medical School, and Sanjay Tanna, Clinical Practice Pharmacist, Blackpool
- De-escalation should be considered: when individuals choose not to have treatment; where there is treatment failure (i.e. control does not improve); and when patients become increasingly frail, have worsening cognitive decline or are approaching end of life.
- Individualise treatment for all, but especially for older people with multiple morbidity.
- Remember that individuals have a “big say” in their treatment – some may be non-adherent or may not be motivated to manage their condition.
- HbA1c can be a misleading measure of glucose control with pregnancy, haemoglobinopathies, chronic renal failure, anaemia, increased red-cell turnover and alcoholism.
- Manage acute intercurrent illness appropriately and remember that glucose levels usually rise with illness. Calorie intake should be maintained. If that is not possible, maintain hydration. Monitor for ketones and recognise when further medical attention is needed.
- Monitor renal function. Many antidiabetes drugs are processed by the kidneys and doses may need to be adjusted accordingly. Renal impairment increases hypoglycaemic risk in people with diabetes. In older people (>70 years), hypoglycaemia occurs more frequently in those with CKD stages 3–5 (Haneda and Morikawa, 2009).
- In older people, cognitive decline is very common. Diabetes greatly increases the risk of dementia, including vascular and Alzheimer’s types (Gudala et al, 2013).
- Be aware of, and allow for, frailty. This is a medical syndrome with multiple causes and contributors in older people.
- For older people, ask the “surprise question”: Would you be surprised if this patient were to die in the next few months, weeks or days? Depending on the answer, and drawing from clinical status, comorbidity, social status, etc, think about what measures need to be taken to improve quality of life and to prepare for future decline.
Resource
- Diabetes UK guidance on end-of-life diabetes care: https://bit.ly/2l4rZja
Mental health – depression, dementia, antipsychotics
Peter Bagshaw, GP, Director SW Dementia Clinical Network
- Although not at first obvious, there are intimate links between depression, dementia and diabetes.
- Preventable risk factors for dementia include hypertension, obesity, smoking, depression, physical inactivity, social isolation and diabetes. Preventable risk factors for depression include obesity, chronic conditions, physical inactivity and excess alcohol.
- In serious mental illness, there is a roughly 20-year premature mortality, primarily from CVD, and mainly as a result of increased rates of smoking, physical inactivity and obesity. Antipsychotic medications increase this risk as all these agents, including the newer ones, tend to increase weight and dyslipidaemia.
- In diabetes, depression is around three times as likely as in the general population, and is the most common psychiatric condition. People with diabetes with depression are, in turn, at greater risk of poorly controlled diabetes, with increased complications from their condition.
- This vicious cycle of inactivity, obesity, depression and metabolic syndrome turning to type 2 diabetes can lead to early death from heart disease and complications of diabetes.
- In addition, poor CV health increases the risk of dementia, for which preventable risk factors are believed to account for around a third of cases. Depression and social isolation are additional risk factors for this condition.
- There are things we can do to reverse this “death cycle”. Improved diet, focussing on weight reduction to reverse metabolic syndrome, is probably the single most important factor. Increased exercise and social engagement are also critical: “What is good for the heart is good for the brain.”
- The DiRECT study showed that, with weight loss, remission in type 2 diabetes was an achievable target in around half of the studied cases (Lean et al, 2018). Examples in the public eye of the success of this approach include that of the politician Tom Watson.
Avoiding errors in diabetes diagnosis
Patrick Holmes, GP, Darlington, and Sri Mada, Consultant Endocrinologist, Durham
- HbA1c cannot be used to diagnose diabetes in people with rapidly changing glucose levels or in pregnancy.
- Diagnostic dilemmas are common and easily missed. Some are not as uncommon as we think.
- The MODY Probability Calculator makes it easier to identify uncommon types of diabetes.
- When symptomatic (4Ts – toilet, thirsty, tired and thinner), always consider type 1 diabetes.
- Consider other types of diabetes when the patient phenotype is atypical; family history may provide clues. Consider specialised tests or referral.
- Type 2 diabetes is a very heterogeneous condition.
- – Look for clinical signs of insulin resistance (such as acanthosis nigricans), as renal outcomes are worse in this sub-type.
- – High HbA1c at diagnosis is strongly associated with insulin deficiency and the need for early initiation of insulin.
- Consider pancreatic cancer in people aged >60 years with a new diagnosis of diabetes or sudden loss of diabetes control, new-onset back pain or gastrointestinal symptoms. CT or MRI scans are the investigations of choice.
- Latent autoimmune diabetes in adults (LADA) diagnosis is difficult.
– Test for two autoantibodies to diagnose type 1 diabetes or LADA. A GAD-positive result is associated with an earlier insulin need; an islet antigen-2 (IA2)-positive result usually indicates a more insidious course.
– Both tests are 100% specific, while GAD has higher sensitivity and persists longer.
MODY Probability Calculator: http://bit.ly/2Fzd3Vi
Exercise: Evidence and engagement
Tom Yates, Professor in Physical Activity, Sedentary Behaviour and Health, University of Leicester
- Exercise interventions are powerful therapeutic options in the management and prevention of type 2 diabetes, with effects that are equivalent or superior to many glucose-lowering therapies (Yates et al, 2009).
- Exercise has a “halo” effect. It benefits over 20 other health conditions, including cancer, depression and musculoskeletal health.
- Only a small proportion (around 5%) of the population achieve 30 minutes/day of moderate-intensity phy




Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025