In 2017, NHS England announced £44 million of transformation funding to improve diabetes care across the country. This included uptake of structured education and achievement of the NICE-recommended treatment targets.
The Royal United Hospitals NHS Foundation Trust (RUH) and Bath and North East Somerset CCG (BaNES) utilised funding to enhance a pre-existing integrated diabetes service to support a culture of learning and quality improvement (Academy of Medical Royal Colleges, 2016) for healthcare professionals and provide best practice. The “three dimensions” of good diabetes care – quality, integration and learning – became known as the 3D project.
Multidisciplinary integrated virtual clinics
Multidisciplinary working improves outcomes in individuals with type 2 diabetes (McGill and Felton, 2007; Bailey et al, 2013). There is now a consensus that integrated care offers benefits such as reduced costs, improved patient satisfaction and higher quality of care, with increased access to healthcare (Auschra, 2018; NHS England, 2018). Drawing on methods used in 2008 pilots (Darzi, 2008), the 3D team developed a virtual clinic model with a directed focus on priority individuals or cohorts above evidence-based treatment targets for HbA1c, blood pressure or lipids, or with HbA1c below 48 mmol/mol in the case of frail elderly or individuals on insulin.
Barriers to integrated care have been well documented and centre around administration, funding and organisation (Auschra, 2018). The transformation pilot allowed medical consultants and a Diabetes Specialist Nurse Facilitator to instigate multidisciplinary team (MDT) virtual clinics in the primary care setting, with two consultants (0.04 WTE each), covering a population of 8500 people with diabetes. A project support administrator ensured that clinics were booked and attendees confirmed. The funding also provided backfill for two members of each practice to attend: one GP (£60 per hour) and one nurse (£23.26 per hour). The virtual clinic length was 3 hours, with two visits per practice per year. All professionals within the practices were invited to attend. The clinic structure avoided the issue of non-attendance. Approximately 18–30 patient care plans were created at each clinic.
Collaborative goal setting (Wallace et al, 2016) was used to underpin discussion. Individualised treatment targets were set which reinforced lower targets for microvascular disease but also allowed relaxation of targets for frail elderly people. The practice nurse and patient discussed any recommendations for treatment changes post-clinic, to ensure a patient-agreed care plan. Patients were simultaneously referred to structured education to increase uptake amongst those who may have been missed or would benefit from more intensive education and support.
Before each practice-based virtual clinic, a one-hour, consultant-led education session was delivered. The lunchtime training allowed staff from other surgeries in the network to attend. On average, 12–20 professionals attended each meeting. Education was based on 12 core topics, including diagnosis, diabetes emergencies, complications and treatment options. The training increased the confidence and competence of primary care professionals, reducing reliance on secondary care opinion. Learning was two-way, allowing primary care to feed back on secondary care communication, policies and systems.
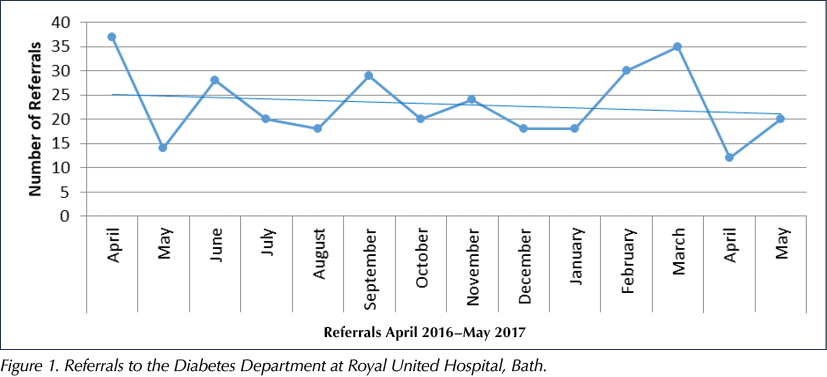
A labour-intensive process of collecting patient data during each virtual clinic for the CCG was replaced with a single Read code, added to the notes of every patient discussed, enabling retrospective searches to monitor health outcomes. A surprise finding was that referrals to secondary care had increased, although these were found to be highly appropriate and were perhaps a reflection of a decrease in clinical inertia previously seen in primary care. Referral rates to the diabetes department decreased over time as practice staff became upskilled (Figure 1). With growth in professional confidence and expertise, the patients selected for discussion became increasingly complex, reflecting changes in primary care priorities including frailty, mental health and type 1 diabetes.
Once all practices had received at least one consultant-led clinic, the MDT was assessed. Overall, 560 patients had been reviewed, with an average of 18 cases discussed per clinic. This approach doubled that of a normal Payment by Results consultant clinic at 50% of the cost, with an average saving of £5200 per month. An average HbA1c lowering of 15.8 mmol/mol (1.45%) was observed in 70% of the patients reviewed. Based on UK Prospective Diabetes Study (UKPDS, 1998) data, this can be interpreted as a potential 51% relative reduction in the rate of microvascular complications and a 20% relative reduction in myocardial infarction rates.
Practice nurse and healthcare assistant competence
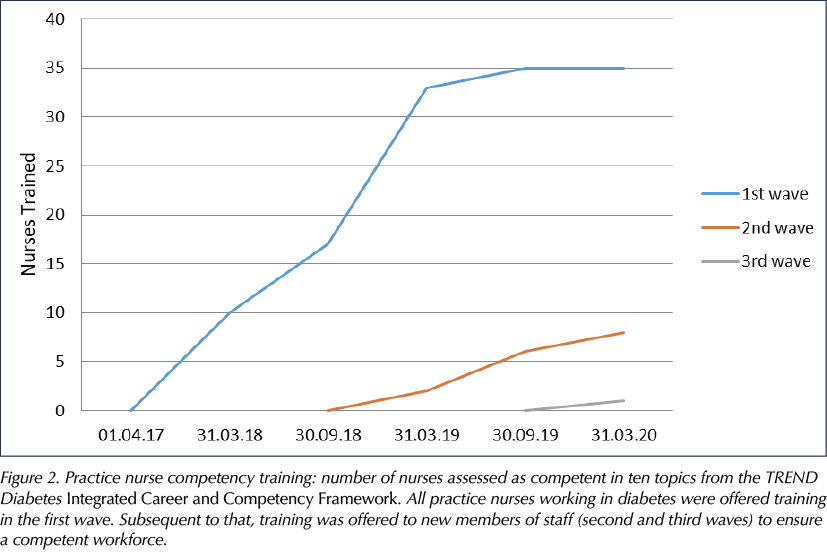
Competence is a set of knowledge, skills and abilities that allow a professional to deliver services to a set standard. Ensuring competence through education and training is essential for the provision of quality services (Kak et al, 2001). In BaNES, inconsistency of education providers and a skills gap analysis revealed variation and need for a standardised approach. Introduction of the TREND Diabetes Integrated Career and Competency Framework for Diabetes Nursing (see TREND Diabetes, 2021, for latest edition) helped to raise self-awareness and identify knowledge gaps. All practice nurses were encouraged to complete a minimum of 10 core competencies, incentivised by 3.5 hours’ backfill payment for education and support from the Diabetes Nurse Facilitator. Length and frequency of training was bespoke and provided one-to-one in practice.
Overall, 88% (n=50) of practice nurses undertook competence training and assessment, and to date 100% (n=56) have achieved level 3 competence in ten TREND core competency topics (Figure 2). In addition, clinical supervision (supported by backfill payment) was offered to help bed theory into practice. These sessions involved the nurse facilitator shadowing a practice nurse in annual review clinics, followed by verbal feedback and clinical and communication advice. Uptake of clinical supervision sessions was 50% (n=23).
Formal education was brought in-house to reflect local needs and was restructured to enable professional development. This encompassed healthcare assistant (HCA) training, a foundation course, care home training and collaboration with the University of the West of England. GLP-1 receptor agonist workshops were created to upskill primary care staff, and insulin workshops were co-delivered with industry partners. Collaboration with neighbouring Wiltshire ensured sufficient numbers for training events. To date, 15 practices (65%) currently initiate insulin. At baseline, no practice initiated GLP-1 receptor agonist therapy, whereas now 100% of practices (n=23) do.
As long-term condition projects developed, an increasing number of HCAs were taking on roles previously undertaken by registered nurses. As nearly 6% of people with diabetes develop diabetic foot disease (Mishra et al, 2017), it was considered important that HCAs be adequately trained to assess an at-risk foot. Completion of the Foot Risk Awareness and Management Education (FRAME; available at: www.diabetesframe.org) online training was mandated, and a one-day training course was developed which incorporated practical foot examination and assessment.
Health coaching
Clinical supervision and patient feedback identified a reliance on directive communication methods and lack of person-centred care. Health coaching, with its toolkit of communication skills, psychology and behaviour change theory, is well matched for diabetes care, which requires both brief interventions and longer-term collaborative working strategies. Behaviour change strategies help professionals to recognise the individual’s readiness for change and, in doing so, promote greater resilience and reduced sense of failure, a key consideration with the current practice nurse shortfall (Aston, 2018).
Transformation funding enabled five nurses (three DSNs and two practice nurses) to attend basic training with a view to setting up an integrated “train the trainers” programme which could accommodate practice staff turnover. Development of a bespoke health coaching programme enabled flexibility in programming and feedback-based change. Health coaching was promoted through an awareness-raising email campaign and through virtual clinics. Thirty-four practice staff attended the initial one-day training (now moved online). To support skills practice and reflection, a programme of email shots and roadshows were provided. The health coaching process is monitored by attaching a Read code to a patient’s notes when health coaching skills are used (embedded into the diabetes template).
Treatment targets
The Bath 3D team took active roles in the BaNES Diabetes Pathway steering group, the foundation of which was based on the NHS RightCare Pathway (NHS England, 2018). The benefits of networking on improving use of resources and bringing together different strategies are well established (Health Foundation, 2014).
Creation of a treatment algorithm, in line with the ADA/EASD Consensus Report (Buse et al, 2020) and the NICE (2015) NG28 guideline, facilitated simplified treatment decision making and included data on drug classes, cost-effective formulary choices and nationally defined targets (NICE and the Quality and Outcomes Framework) to ensure that professionals understood the aims of patient care. A “Know your target” campaign accompanied this. The algorithm was complimented by teaching in the MDT clinics, at the quarterly practice nurse forums and disseminated via the CCG medicines optimisation team. Other projects included a review of GLP-1 receptor agonists, blood pressure process mapping and insulin safety. The largest project centred on pregnancy and included creation of pop-up reminder messages on IT systems for all female patients under the age of 50 years, development of a referral pathway, and IT templates for preconception advice and pregnancy.
A diabetes care template was developed for general practice in order to combine care processes, links to local guidance and a printable care plan for patients. It also ensured consistent coding and more efficient data collection. Data analysis is central to quality improvement projects and can identify problems, track the impact of interventions and define improvements (Alderwick et al, 2017). Prior to each virtual clinic, a data dashboard was provided which allowed the MDT to target areas for discussion. Case-by-case discussion led to creation of a 12-month care plan that was recorded contemporaneously. The majority of follow-up was primary care-led, with occasional specialist intervention identified. The dashboard was developed with the South, Central and West Commissioning Support Unit in an attempt to obtain real-time data on practice achievement. Based on the metrics of the National Diabetes Audit, it consisted on a set of searches run in SystmOne that allowed the practice to see the proportion of their register undergoing the key care processes and meeting the defined key treatment targets. As a snapshot, it generated immediate areas for discussion and allowed the practices to gain a more holistic picture of their achievements.
A 12-month review revealed that practices were struggling to instigate the changes required, principally due to administrative barriers and small team size, compounded by lack of succession planning and an inability to recruit nurses with diabetes experience. Lack of practice diabetes team meetings inhibited oversight and further complicated system reviews. The response was to hire a specialist prescribing secondary care pharmacist, with a background in diabetes and quality improvement, to support better outcomes. The role of pharmacists in improving diabetes care is established (Khunti et al, 2013) and has been well discussed in the literature. Quality improvement theory has shown a benefit in improving practice and reducing variation (Solberg et al, 1997; O’Connor et al, 2005). The pharmacist was intentionally embedded in practices to allow a focus on their individual barriers and achievements, as opposed to an overarching CCG-level review.
Whilst the dashboard had proved useful in the virtual clinics, it did not allow identification of population subsets which would benefit from additional clinic input or comparison with others within the CCG. It was also restricted by governance, whereby the Commissioning Support Unit could not collect data on patients who had not consented to share data. In some practices, up to a third of the diabetes register was affected by this, which severely biased the results seen. Therefore, new searches were written in collaboration with a general practice administrator, containing a detailed breakdown of the practice diabetes population. The virtual report was instigated in primary care prior to virtual clinics to enable practices to identify areas for focus. At a later date, the CCG facilitated a data sharing agreement which enabled reports to be run on behalf of practices for use at virtual clinics. Data sharing and the benefits of MDT case discussion were communicated to patients by text, letter and the placement of posters in practices, and all patients were given an option to opt out.
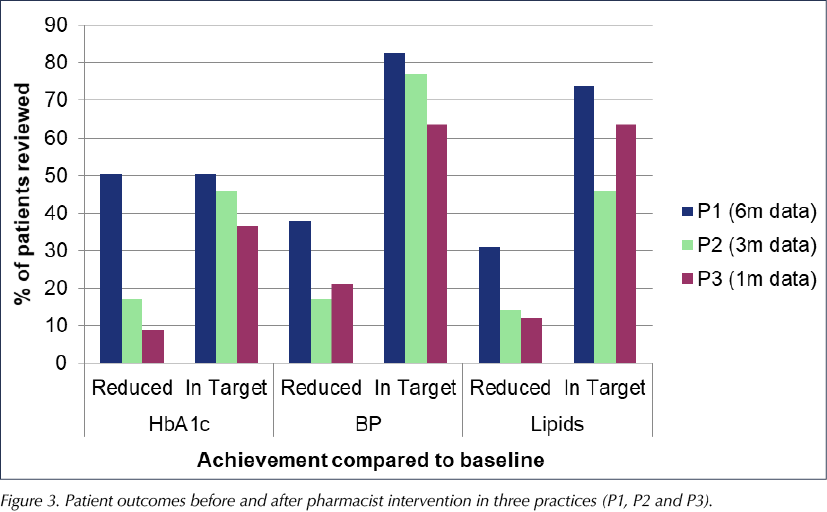
Initial plans for prescribing pharmacist clinics were altered as the priorities of upskilling practice staff and quality improvement projects were identified. In all practices, the pharmacist used process mapping to identify barriers to achievement and uncover any hidden issues. The findings were presented to practices with a basis in finding solutions and sharing practice from national or local projects. Most solutions were owned and delivered by the practices themselves. Patients with clinical interventions were Read coded to allow data collection and tracking. Treatment target achievement results improved in every practice post-visit. Practice 1 has shown the most significant improvements due to the greatest number of patient reviews (n=103) and the longest duration of monitoring (6 months). However, even at 1 month, practice 3 (n=33) has shown improvement in achieving treatment target outcomes (Figure 3).
The Integrated Pharmacist role has led to a greater understanding of where pharmacists, alongside clinicians and specialist nursing teams, add value to diabetes care. The focus on quality improvement and change management led to small changes that rapidly and successfully changed patient management and engagement.
Long-term conditions project
Funding was diverted to a project developed by one general practice and expanded across the CCG. Based on administrative changes to diabetes recalls and patient stratification by complexity (Academy of Medical Sciences, 2013), this long-term conditions (LTC) framework ensured that all patients were seen by an appropriately skilled professional. Process mapping looked at who was performing tasks and where efficiencies could be found. Increased use of HCAs freed up practice nurses for consultations. The number of HCAs across the 23 practices continues to increase and is up to 24 at the time of writing.
A data specialist was hired to provide support to practice administrative teams in writing searches and developing templates and recall systems. The role offered invaluable insight into barriers to progress. The result was increased capacity to deliver changes to systems without putting undue pressure on primary care teams, and led to increased adoption of the LTC project across the CCG. The CCG is adopting and extending this system to other long-term conditions.
Summary
The NHS England transformation fund was designed to deliver improvements in diabetes care. Additional funding has allowed BaNES CCG and RUH to deliver innovative pilots to change infrastructure in practices and how care is delivered. In doing so, it has improved the confidence, competence, knowledge and skills of those already involved in primary care diabetes. Strong leadership has created a network of professionals striving to do more with limited time and resources. Improvements have been seen in care process delivery and attainment of treatment targets. This has resulted in more patients being treated closer to home and a reduction in referrals to secondary care.





How a new model of care has improved outcomes for people with diabetes.
2 Dec 2025