As a complex condition, diabetes affects all aspects of daily life and requires intensive treatment to prevent long-term complications (Speight et al, 2019). Healthcare professionals can offer person-centred support within consultations, by considering the impact of lifestyle factors on young people (YP) when making clinical and treatment decisions. This requires asking potentially sensitive questions, including about dietary intake and daily activities, with varying levels of information gathering.
Consequently, YP and their families may feel as though they are “under the spotlight” during routine consultations, particularly with the growing use of data gathered by diabetes technology. This is an opportune time to review the experience of intrusiveness in clinical practice and research, as the extent of it during consultations remains unclear owing to its limited evidence base.
Background evidence
Consultation experiences
During adolescence, YP transition through a period of rapid physical, cognitive and psychosocial growth, ultimately affecting the way they feel, think and make decisions (World Health Organization, 2023). During this period, it is developmentally appropriate for YP to engage in risk-taking behaviour whilst seeking increased independence and privacy (Deeb et al, 2018). Healthcare professionals (HCPs) can recognise that discussions around daily routines, including social activities, can hold different meanings for YP than for younger children.
YP often consider their diabetes as paradoxical, as they try to balance a “normal” way of living with the burden of self-management. This complicates the challenges of adolescence and impacts on their concordance with positive diabetes-related behaviours (Christie, 2019; Ingersgaard et al, 2021), meaning HCPs need to adapt their communication styles and support provided for YP.
Consultations aim to engage YP with their diabetes management by supporting them in overcoming difficulties, whilst harnessing their current goals. HCPs should realistically balance the need for YP to achieve optimal glycaemic management with an appreciation of their efforts, to avoid them feeling “like a piece of machinery” (Davison et al, 2021). In practice, supporting increased autonomy and privacy, whilst information gathering during consultations, engages YP by recognising their psychological needs.
Sharpe et al (2021) acknowledged that YP often “edit out” information regarding their diabetes management and may not be fully transparent within their consultations to keep aspects of their routines undisclosed. Equally, parents report feeling anxious going into consultations, resulting in them omitting or fabricating information (Lawton et al, 2015; Overgaardd et al, 2020). Although unintended, YP and their families may feel overwhelmed and experience feelings of intrusiveness, particularly as there are usually multiple HCPs present during consultations (Kime et al, 2022).
Despite this, across England and Wales, 82.5% of children and YP report having a positive relationship with their diabetes teams (Royal College of Paediatrics and Child Health, 2022). HCPs achieve this by remaining friendly and interested, and by ensuring they are not too personal in their attitude to gathering information, demonstrating they are helpful rather than intrusive (Archibald and Ashford, 2018). This creates a comfortable atmosphere for YP and their families, enabling a shared approach and rapport building, which are fundamental in achieving optimal care outcomes.
Use of technology
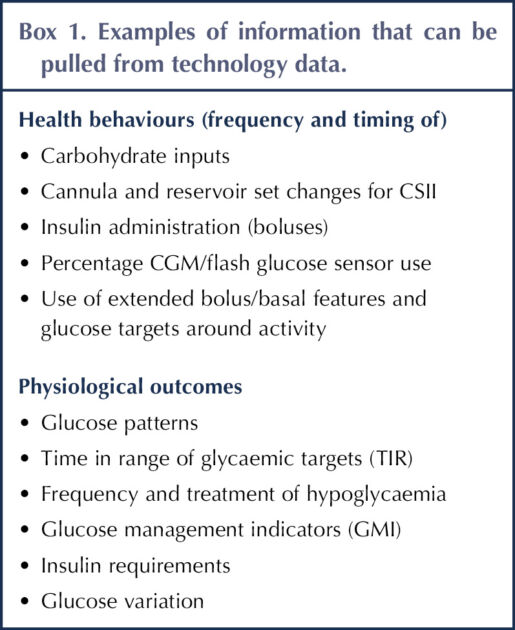
The rapid evolution and growth of diabetes technology has created a lag in the literature and gaps in evidence, which are mirrored in wider technology uses, such as social media (Kubiak et al, 2020). Wider access and funding to technology, such as continuous glucose monitoring (CGM), continuous subcutaneous insulin infusion pumps (CSII) and automated insulin delivery systems (AIDs), has improved the quality of life for many YP and their families, whilst helping to achieve glycaemic targets and lower HbA1c (Brew-Sam et al, 2021). In practice, diabetes technology provides information around health behaviours and physiological outcomes (Box 1) that assists HCPs in their support for YP and their management.
Moreover, Piras and Miele (2019) advocated that “digital intimacy” can develop between patients and HCPs as technology increases the quantity and quality of communication between them. Technology can create stronger familiarity within the patient–HCP relationship, extending to face-to-face encounters and ultimately enhancing the consultation experience for YP. Despite this, it is possible that the use of digital monitoring can feel intrusive to users and as if they are under surveillance, by revealing the “truths” about their diabetes management to HCPs (Oikonomidi et al, 2021).
This potential intrusiveness afforded by technology is particularly felt around food monitoring and receiving real-time feedback. Young people can feel nervous of consultations as “the data from the blood tests don’t conceal anything”, highlighting a lack of privacy that may be felt as HCPs have unfiltered access to technology data displaying their daily management (Wang et al, 2010). Technology use and remote uploading can cause initial discomfort for parents too, as they feel that their private lives’ are being watched by HCPs (Kimbell et al, 2022).
Overall, this presents a unique challenge within consultations for YP with diabetes, their families and HCPs, particularly when compared with other long-term health conditions where this level of technology data is not available. Nevertheless, when used sensitively with an open-minded approach, YP and their families can build trust and rapport with HCPs over technology data.
Patient feedback
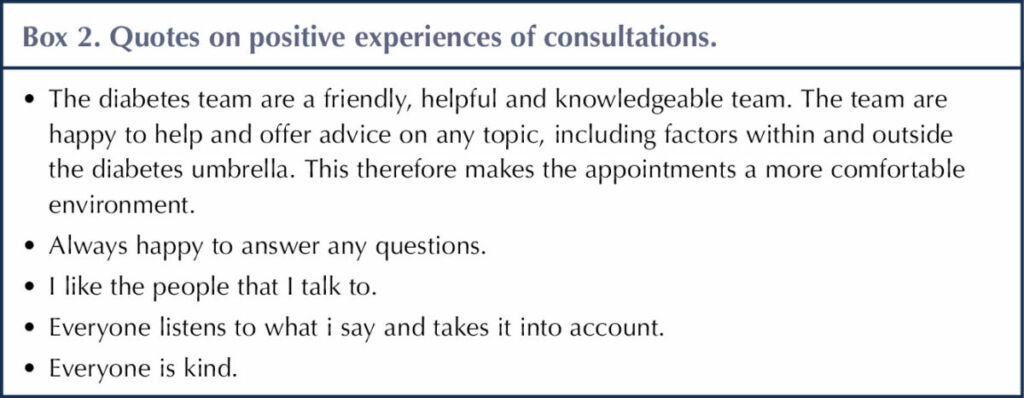
Within a local paediatric diabetes unit (PDU), feedback was collected from 12 YP (aged 12–17 years) to draw together their experiences of diabetes consultations. 91% of them reported feeling comfortable during consultations, as they are “welcoming” and “friendly” (Box 2).
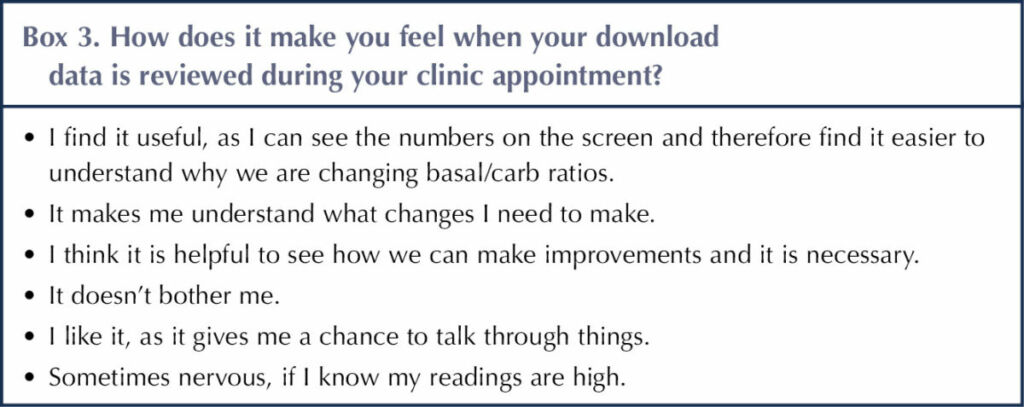
Most of the feedback showed that YP find it helpful for HCPs to review their technology data, as it facilitates discussions around diabetes management, allowing HCPs to share their knowledge and advice (Box 3).
Responses also indicated that most YP did not feel that discussions or questions during their consultations were too personal or intrusive, although a small number have occasionally felt “awkward”. Despite this, 33% of the YP felt that reviewing data increases opportunities to be “caught out”, focusing on areas of management they are unhappy about or finding difficult. Acknowledging this highlights the impact of communication around technology data and diabetes management, to ensure YP feel guided, rather than judged, by HCPs.
Interestingly, YP expressed that they did not feel it necessary for HCPs to gain their consent to review their data as it “is their job”, “doesn’t bother [them]” and “is needed to make decisions”. This may demonstrate their appreciation for technology in supporting clinical treatment decisions, as part of routine care. However, it may warrant further exploration into whether YP do not consider ownership over technology data, treating it as if it is not “theirs”. Research hasn’t yet captured the deeper impacts this may have on the relationships YP have with their diabetes diagnosis and multidisciplinary team (MDT) over time.
Although reporting positively of their experiences (Box 2), YP presented that consultations can be overwhelming. They can be “daunting, as there are many people in the room”, making them “nervous sometimes” and “dreading it, as managing diabetes is very hard”. One young person highlighted that they “want to give [them] all the answers they need”, revealing the pressure YP may feel coming into consultations, despite the best intentions of HCPs.
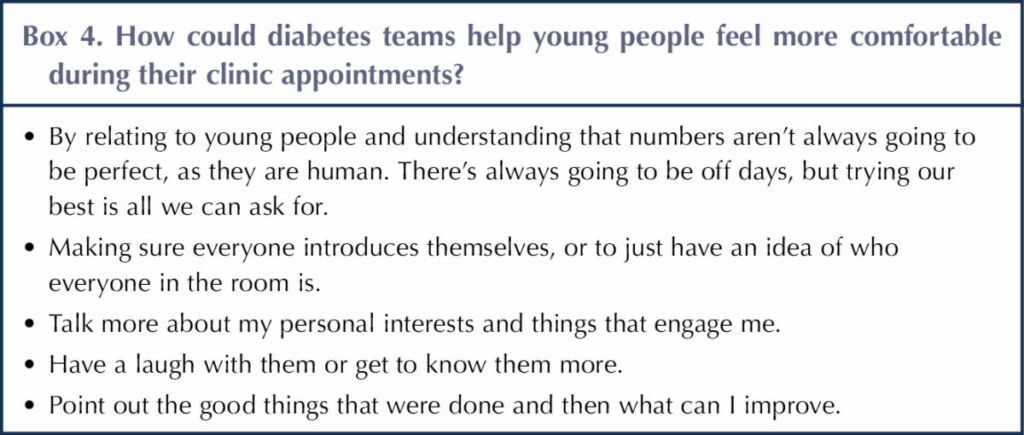
To ensure YP feel able to engage in discussions around their technology data as a factor that could exacerbate feelings of pressure and intrusiveness, and to maintain a relationship with the MDT, feedback suggested that HCPs explore their interests and get to know them holistically (Box 4).
Young people appreciate the benefits of HCPs reviewing technology data to support decision-making in their role. They can, however, feel exposed in consultations, and there is potential for unintended intrusiveness around technology use. Considering the small scale of this feedback and possible social desirability in the responses, it would be helpful for wider research to be conducted around the long-term impact of reviewing technology data within consultations, to guide HCPs on the best practice.
Implications on practice
Using person-reported outcomes
Widely used as screening tools to evaluate healthcare services, person-reported outcomes (PROs) are increasingly being implemented into clinical care to represent a person’s own perspective on their health and quality of life (de Wit et al, 2020). Using PROs to guide clinical interactions allows YP to become more transparent with HCPs, broadening consultation discussions by making them strengths-based and motivational, whilst identifying any concerns (Snyder and Aaronson, 2009; de Wit et al, 2020).
The local PDU has recently implemented the use of a Well-being in Diabetes questionnaire within annual review appointments, or in individual cases where difficulties have been noted. The questionnaire is provided to YP and their families before consultations, encouraging them to assess their current feelings around aspects of diabetes management, relationships, education and mood. They can document any questions or comments alongside their interests and goals, to draw upon the thoughts of YP and to facilitate a person-centred approach.
Although physiological outcomes can be addressed by pulling data from diabetes technology, the well-being questionnaire enables YP to discuss their priorities and needs during consultations. Use of the questionnaire could be extended across all diabetes consultations to prevent any potential feelings of intrusiveness for YP and their families when reviewing technology data, by supporting their multifaceted needs and encouraging their involvement.
Written information is useful when YP find it difficult to express themselves verbally. Additionally, HCPs experience improved satisfaction as consultations become more collaborative and rewarding, and facilitate closer professional relationships (Rotenstein et al, 2017), which has been felt in local practice.
Motivational interviewing
Motivational interviewing (MI) is a guiding style of communication that can reduce the sense of intrusiveness within consultations, as it aims to guide YP to recognise their own areas for change by harnessing their motivation (Steinberg and Miller, 2015). Rather than implementing the agenda of HCPs, MI encourages YP to explore their own thoughts, with the guidance of HCPs, to achieve the best outcomes.
MI enables positive interactions with YP, as it emphasises the expression of empathy, use of open-ended questions, support of setting their own incremental goals and the asking of permission to give advice (Schaefer and Kavookjian, 2017). This allows interactions around diabetes management and technology data to be informative, rather than intrusive, meeting the wider needs of YP and focusing on positive affirmations to set future goals. Promoting this non-judgemental MDT ethos, and including YP in decisions around their care, encourages trust with HCPs and facilitates open discussions (Davison et al, 2021; Pembroke et al, 2022).
The latest International Society for Pediatric and Adolescent Diabetes (ISPAD) guidelines recommend the use of MI by clinical psychologists (Gregory et al, 2022). Despite this, the clinical psychologist within the local PDU has arranged training in the use of MI for the whole diabetes MDT, as this investment incorporates enhanced communication skills into all consultations and can obtain the same benefits for YP with a variety of HCPs.
Language Matters
With increasing use of diabetes technology, communication and use of language in clinical practice needs to be adaptable to ensure YP and their families feel supported by HCPs, to avoid judgement and recognise their experiences of healthcare. As a global movement, the Language Matters campaign aims to increase HCP awareness of the impact of language on motivation, health behaviours and care outcomes and, consequently, improve communication within diabetes care (Odiase et al, 2020). By communicating effectively, HCPs can inspire, build confidence and increase motivation to engage in self-care behaviours for YP with diabetes (Holt and Speight, 2017), whereas unconscious or even well-meaning poor choices in language can be hurtful and reverse any positive efforts of self-care.
People with diabetes will mostly prioritise what their HCPs communicate to them, over the influences of the media and their peers (Walker, 2018). HCPs should, therefore, seek to be empathetic, empowering, respectful and clear in their approach, and mirror this in their choice of words and phrases when reviewing technology data (Bateman, 2021).
It is acknowledged that increasing time constraints and provider burnout within healthcare can impact on communication with YP, the support they receive and their health outcomes, highlighting the importance of making each interaction count (Patel et al, 2018). Considering the positive impact of Language Matters principles, HCPs can efficiently direct time-limited consultations to gather information and discuss technology data, whilst providing support and listening to the needs of YP.
Conclusion
Evidence suggests a potential for YP and their families to experience intrusiveness within diabetes care. HCPs can remain mindful of this within practice, using effective communication to create positive consultation experiences, alongside technology uses, for YP and their families.
Diabetes technology is proving beneficial in many ways, but are there unintended future consequences on the psychosocial well-being of YP that may have not been fully brought to light? To gain this deeper understanding, further research into technology use and its impact on consultation experiences would be beneficial. It would also be interesting to evaluate its implications on family relationships and conflict, and psychosocial development. Considering the perspectives of YP in future research ensures that clinical practice continues to develop to meet their needs holistically, parallel to the growth of diabetes technology.





Developments that will impact your practice.
22 Dec 2025