Preventing illness is at the heart of the NHS Long Term Plan (NHS, 2019a). It suggests that the NHS should be more differentiated in the support it offers to individuals by making progress on prevention, inequalities and responsiveness to the diverse people who use and fund the health service. Moreover, it acknowledges that a one-size-fits-all statutory service has often failed to engage with the people most in need, leading to inequalities in access and outcomes. So why are we waiting until the age of 40 years to commence the NHS Health Checks in ethnic minority groups?
Type 2 diabetes can be undetected for up to 10 years, with complications beginning at 5–6 years before the actual diagnosis (Diabetes UK, 2019a). Furthermore, people with a family history of diabetes are 2–6 times more likely to have diabetes than people without (Diabetes UK, 2019b). Moreover, the National Institute for Health and Care Research (2022) suggests that body mass index (BMI) is a major contributor to many chronic health conditions, with many ethnic groups having an increased risk of type 2 diabetes and hypertension at lower BMIs than White populations.
In 2021, CORE20PLUS5 was introduced by NHS England. This initiative focuses on reducing healthcare inequalities in the 20% most deprived populations in the nation, plus high-risk population groups identified locally, which may include ethnic minority groups (NHS England, 2021). Five clinical areas of focus are identified – maternity, severe mental illness, chronic respiratory disease, early cancer diagnosis and hypertension.
With this in mind, the staff survey reported here focused on ethnic minority groups working within the Liverpool University Hospitals NHS Foundation Trust (LUHFT), and the chronic health conditions of type 2 diabetes and hypertension. The survey aimed to establish the groups most at risk and to raise awareness of the importance of early intervention.
Methodology
A staff survey (Box 1) was devised based on the NICE guideline for the prevention of type 2 diabetes in people at high risk (PH38; NICE, 2017), and the known risk factors for type 2 diabetes and hypertension (Diabetes UK, 2020; Blood Pressure UK, 2021). Before the survey was registered with the Clinical Audit Management Systems, consent to conduct it in the Trust was obtained from the Chief Nurse; the Equality, Diversity and Inclusion Lead; the Deputy Director of Nursing Workforce Development; the Programme Lead for Health Inequalities; and the Health & Wellbeing Lead at LUHFT.
This was a voluntary and anonymous study, so no personal details were collected and any completed survey implied informed consent. Any staff member that wanted to be invited to future health days in the Trust had the option to leave their email address upon completion of the survey.
The survey was circulated to the four LUHFT sites through the Trust’s communications system. Participants were able to complete it electronically (in about 10 minutes) in Microsoft Forms. To enhance its success, the survey was also emailed to ethnic minority forums, ward managers, matrons, doctors and various leads in the Trust. Printed copies with the survey link and scan code, were circulated on the wards, notice boards and during the international nurses’ celebratory day. Above all, the study preserved confidentiality in accordance with the Nursing and Midwifery Council (2015) guidelines by ensuring all data collected was only stored in NHS password-protected computers.
The survey was conducted over 6 weeks (at the end of October to the beginning of December 2022). It only involved people from an ethnic minority background who were aged 25–45 years, with no diagnosis of type 2 diabetes, hypertension or high cholesterol.

Results
Although the Trust has 1445 staff aged 25–45 years who are from an ethnic minority group, only 66 individuals completed the online survey. One submission was excluded, as the participant fell outside the inclusion criteria.
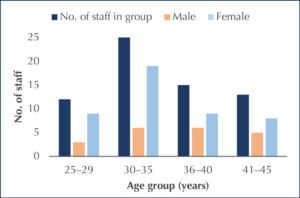
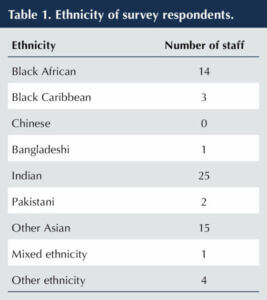
Of the 65 survey responses that were analysed, 45 (69%) were from female participants and 20 (31%) from male. The age group and sex of the respondents is summarised in Figure 1. Asian ethnic groups were most commonly represented (25 respondents), followed by 14 with a Black African background, 3 with a Black Caribbean background, 1 with mixed ethnicity and 4 from other ethnic groups (see Table 1).
Close family histories of diabetes (31) and high blood pressure (31) were the chronic conditions most commonly mentioned, followed by high cholesterol (18), myocardial infarction (5), stroke (3) and heart failure (1).
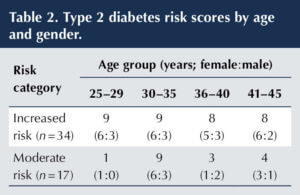
Analysis of the “Know your risk” responses for type 2 diabetes showed that 13 respondents reported a low risk score, 34 an increased risk, 17 a moderate risk and 1 a high risk. A breakdown of those in the increased risk and moderate risk groups by age group and gender is shown in Table 2.
Heart age scores from the NHS calculator were reported by 53 participants aged >30 years, with 18 (11 female and 7 male) reporting a heart age older than their actual age. Of these, 11 (61%) were of Asian ethnicity, 5 (28%) were of Black African or Caribbean ethnicity, and 2 (11%) from other ethnic groups.
Worryingly, of the 13 staff >40 years old, only 5 (all females) had been invited for an NHS Health Check to spot early signs of stroke, kidney disease, heart disease, type 2 diabetes or dementia.
Discussion
This snap-shot survey represented various ages and ethnic minority groups. It should be noted, however, that more women completed the survey than men, and it was difficult to get good engagement from the male staff. This is not unusual in the UK. A large study showed that women aged 16–44 years are twice as likely as men of the same age to visit their GP and engage in their health care (Wang et al, 2013). Additionally, the Office of National Statistics (2021) reported that UK males are more likely to die from causes that are considered avoidable (in the presence of timely and effective healthcare or public health interventions) than females. It is paramount, therefore, that more work is done to improve male engagement in health.
Certain ethnic groups, such as South Asians, have a predisposition to type 2 diabetes in the presence of risk factors, such as obesity and central fat distribution that result in insulin resistance, compared to White populations (Oldroyd et al, 2005). They may also develop the condition at an earlier age. Furthermore, evidence shows that people from Black African or Caribbean groups have a high prevalence of hypertension, with or without diabetes. The high number of our survey participants reporting a close family history of diabetes or hypertension reflects this.
Although, a family history of myocardial infarction, stroke and heart failure were reported less often in the survey, these cardiovascular diseases must be taken seriously as they are closely associated with type 2 diabetes and hypertension, and often arise as complications in individuals without good blood pressure and/or glycaemic control (Petrie et al, 2018; Diabetes UK, 2020). A further potential complication of diabetes, diabetic retinopathy, is a leading cause of blindness in working-age people in developed countries; over 60% of people with type 2 diabetes develop some degree of diabetes retinopathy in the 20 years after diagnosis (Broadbent et al, 2019). With a high proportion of staff in our survey reporting increased, moderate or high risk scores for type 2 diabetes, and 34% calculating a heart age older than their actual age, it is vital that ethnic minority groups become more aware of their risk factors so that they can make lifestyle changes earlier and reduce risks of future complications (Sattar and Gill, 2015).
Despite the guidelines recommending that NHS Health Checks should be offered every 5 years in those aged 40–74 years without a pre-existing condition (Public Health England, 2019; NHS, 2019b), this survey indicated that 62% (8/13) of respondents aged ≥41 years had not received an invitation. Moreover, only female staff confirmed that they had received an NHS Health Check invitation, which emphasises the need for greater engagement with men and their health. While this data is worrying, it should be noted that GP services have been under immense pressures following the COVID-19 outbreak, and there is a declining number of GPs in the service. Additionally, the rising demand in community services and struggles in staff recruitment and retainment inevitably have an effect on service provision (BMA, 2022).
In 2010/11, the direct costs of diabetes (treatment, intervention and complications) to the NHS was estimated to be £9.8 billion, with type 2 diabetes accounting for £8.8 billion of this (Diabetes UK, 2014). Diseases caused by high blood pressure have been estimated to cost the NHS over £2 billion every year (Public Health England, 2014). There is clearly, therefore, a need for greater awareness of the risk factors for these health conditions. Furthermore, studies done in the USA (Iqbal, 2013) and UK (Nazar et al, 2016) suggest that early screening, treatment and education can prevent or delay the onset of diabetes and other long-term health conditions.
The findings of this survey of support the recommendation of expansion of eligibility of the new NHS Health Checks to include people aged 30–39 (Office for Health Improvement & Disparities, 2021), and the supporting evidence from NICE (2017) that risk assessments should be done from the age of 25 in people from ethnic minority groups. There is a need to raise awareness early of the risk factors for chronic conditions, such as type 2 diabetes and hypertension, in NHS staff from ethnic minorities.
Study limitations
The survey response rate was small owing to a number of factors. It was an electronic survey conducted during the autumn–winter period when there were high hospital pressures, and staff from one of the Trust’s sites had recently moved into a new hospital building, limiting their time to complete surveys. As there was lack of prior research in this area, and only 5% of staff aged 25–45 years and from an ethnic minority group completed the survey, the authors recommend that a larger cohort is studied in four phases, with each phase concentrating on the four LUHFT sites in turn. The study should be conducted in person and over a period of 6 months to ensure that ethnic minority staff in the Trust are well represented.
Conclusions
Since having a family history of diabetes, hypertension, high cholesterol, myocardial infarction, stroke or heart failure increases one’s risk of developing other chronic health conditions, this snap-shot survey supports the view that there is a need for more awareness of risk factors in the ethnic minority groups. A greater awareness of NHS Health Checks, and the importance of people >40 years requesting one through their GP centre if they have not received an invitation, is needed. Additionally, if a younger individual has additional risk factors, such as a strong family history, they should have the opportunity to opt in for a health screen despite their age.
The survey showed there is a need for men working in the NHS to engage more with their health. Signposting health services, in places such as community centres, and working collaboratively with faith leaders may help improve this.
Because of this project and collaborative work with the Equality, Diversity and Inclusion Lead, and the Health and Wellbeing Lead, this Trust will hold health days in January 2023 to support staff with all aspects of their health. Although this is a small step in supporting staff health, it may help to reduce staff sickness, increase awareness of chronic health conditions and improve health outcomes not only for the staff, but also for their patients.
Acknowledgements
The authors would like to thank: 1. Steven Colfar and Patricia Hughes for this secondment opportunity and support in conducting this project in the North West; 2. Julie Brake and Dr Reza Zaidi for their guidance and support in getting this project registered in LUHFT; 3. Pauline Whitby, Laura Crompton, Yvonne Browne, Vanessa Laber and Farhana Darwich for their guidance on diabetes data, health inequalities programmes and how to undertake this project; 4. Caroline Holtom for her guidance in the NHS Health Checks data and Public Health policies; 5. Tinei Kochai and Rajesh Karimbath for their guidance in workforce data analysis; and 6. Kamali Smith, Roehl Gaerlan, Tom Southern and Alice Ndebu for their continuous help to circulate this survey in the LUHFT sites.





Developments that will impact your practice.
26 Feb 2026